INTRODUCTION
Conjunctival and corneal pigmented lesions, ranging from benign to malign lesions, are observed in numerous conditions including nevus, primary acquired conjunctival melanosis (PAM) with and without atypia, and malignant melanoma. PAM is an important benign pigmented condition that can result in melanoma, and it is most common in middle-aged or elderly Caucasian individuals(1). The histological appearance of melanocytic proliferation including melanocytes with atypical features found in all levels of the epithelium is observed in PAM with atypia and that of melanocytes lacking atypical features is observed in PAM without atypia(2). In this case report, we present a corneal PAM without atypia in a patient with a history of limbal malignant melanoma.
CASE REPORT
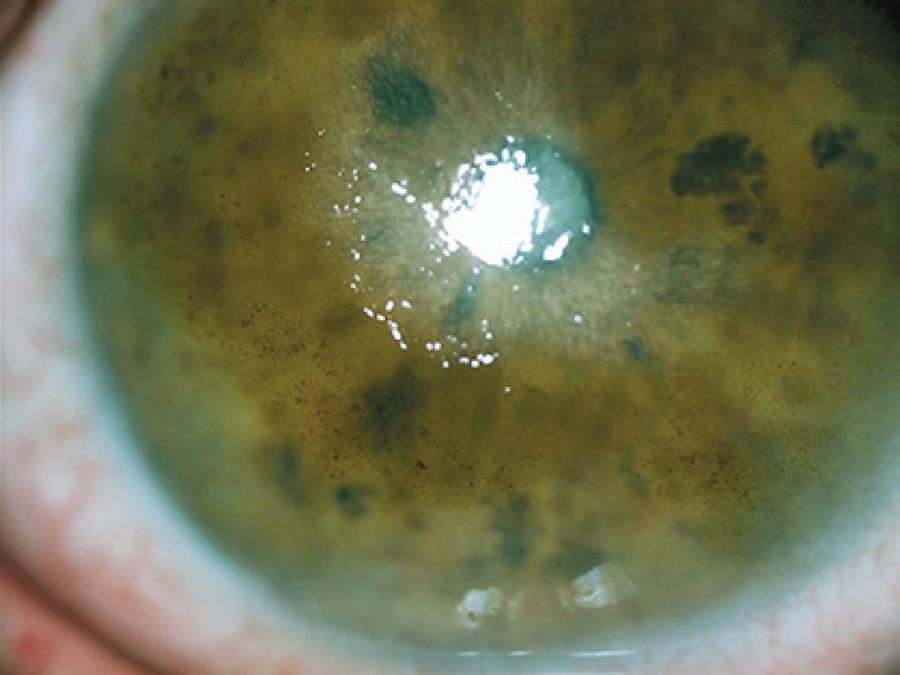
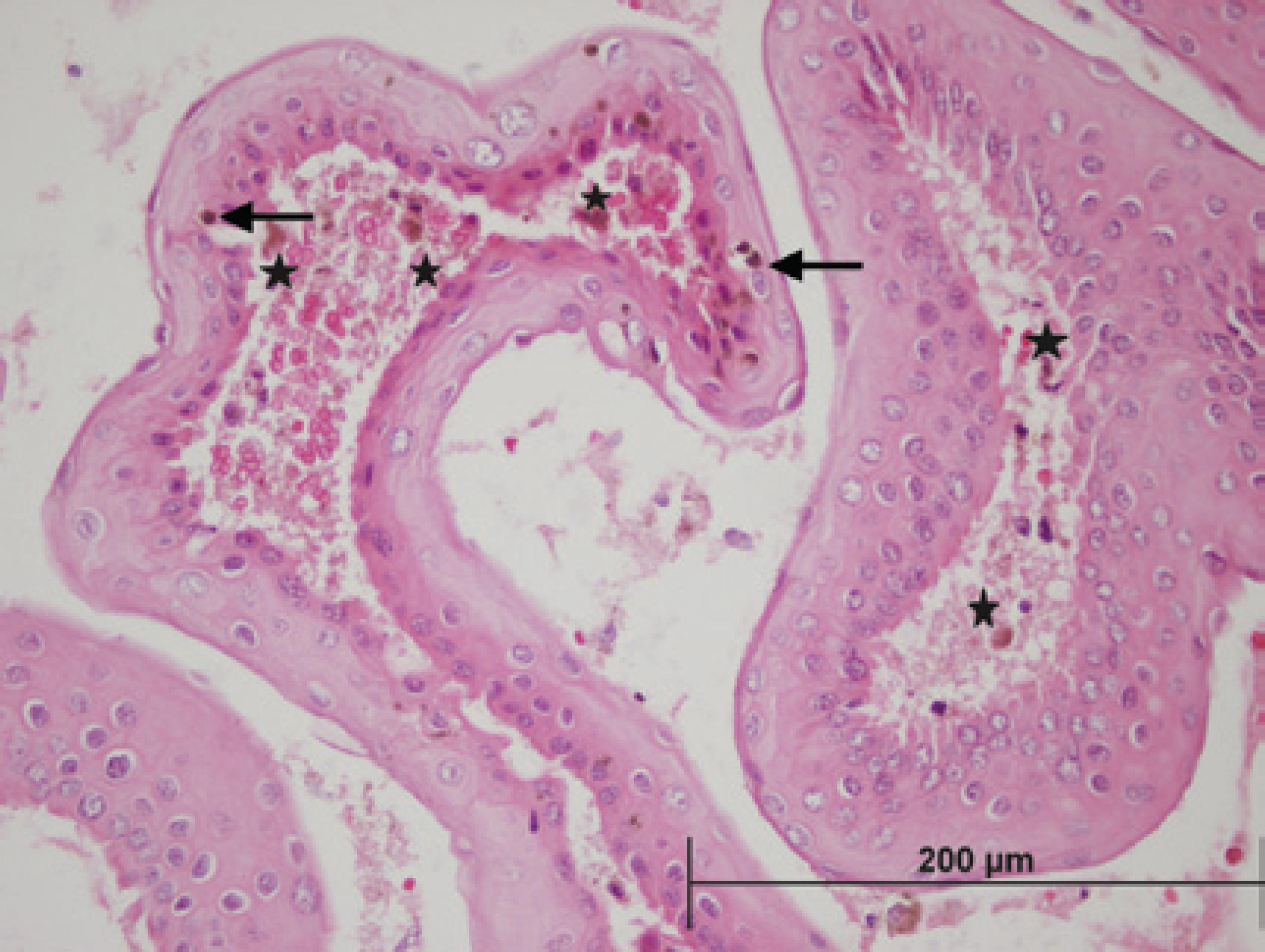
A 75-year-old woman presented with blurred vision, excessive tearing, and photophobia in the right eye. The patient had undergone a nasal conjunctival malignant melanoma excision, without adjuvant cryotherapy or chemotherapy, performed by an outside surgeon, 18 months earlier. Upon examination, her visual acuity was 1/10 in the right eye. Slit-lamp examination showed a patchy melanotic pigmentation covering the upper-nasal limbal quadrant, periphery, and mid-periphery of the cornea, without corneal vascularization and corneal epithelial defect. In addition, a central corneal haze was observed in the same eye (Figure 1). The initial treatment included topical mitomycin-C (MMC), fluorometholone acetate, and artificial tears. Topical 0.04% MMC was applied four times daily for 1 week. Then, MMC was discontinued for 1 week. Her symptoms resolved, visual acuity improved, and the corneal haze disappeared after the application of this regimen four times (Figure 2). However, the pigmented lesions persisted. Therefore, we excised the corneal epithelium and underlying pigmented layer using alcohol corneal epitheliectomy. Histopathological examination demonstrated PAM without atypia (Figure 3). The lesions were successfully removed, and there were no recurrences during the follow-up period of 36 months (Figure 4). At her last visit (at 36 months), the visual acuity was 10/10 in the right eye.
DISCUSSION
The most important lesions arising from the melanocytes of the conjunctiva and episclera are nevus, racial melanosis, PAM, and malignant melanoma. PAM is classified as with or without atypia. The clinical appearance of conjunctival PAM is unilateral and conjunctival, and it is rarely associated with corneal melanotic macule developing in the elderly. The pigmentation tends to be irregular and waxy and gradually becomes more extensive and multifocal. Histologically, diffuse, intraepithelial melanocytic proliferation can be observed, with increased numbers of melanocytes confined to the basal layer of the conjunctival epithelium. These melanocytes are either normal or hypertrophic, possibly with an increased number of dendrites, showing no cytological features of atypia or malignancy(3).
Small lesions of PAM are often managed initially by observation. Lesions with changes or extensive lesions should be biopsied. At least 35% of PAM lesions progress clinically, and at least 11% develop into melanomas within 10 years(1,4). PAM without atypia is not considered a premalignant lesion and does not require treatment. PAM with atypia carries a risk of malignant transformation. The extent of PAM, measured in clock hours, best correlates with the risk of transformation into melanoma(1,4). Small lesions (<1 clock hour) can be followed up by clinical observation. Larger lesions are generally treated by surgical excision and cryotherapy. Oral mucosal or amniotic membrane grafting may be required to fill defects after larger excisions. Unresectable or recurrent diffuse PAM with atypia is managed by mapping biopsies and cryotherapy or MMC and close clinical follow-up(1,4).
Two notable features of this case should be emphasized. First, the association of conjunctival and corneal melanosis, a rare condition, was observed. Moreover, Shields et al. have reported a case of conjunctival melanosis with atypia involving the cornea that was completely healed with topical application of MMC(5). Another case of melanokeratosis due to chronic trauma showed recurrence during follow-up of alcohol corneal epitheliectomy(6). Second, the co-existence of central corneal haze and melanosis, which may have decreased the best-corrected visual acuity, was observed. The haze completely disappeared, and visual acuity improved because of the MMC treatment within 1 month. However, the melanosis persisted; therefore, we performed alcohol corneal epitheliectomy. We observed no recurrence in the 3-year follow-up period after epitheliectomy.
In conclusion, we present this case to illustrate that PAM without atypia can occur in the cornea and cause complaints. Topical MMC and alcohol corneal epitheliectomy can be useful treatments in this condition.






 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

