INTRODUCTION
The outcome of cataract surgery is based on the technical quality of the procedure and the presence of other ophthalmic diseases or complications before, during, and after surgery.
To identify the potential visual acuity (VA) to be achieved following surgery, and to identify other diseases that can affect the final result, various tests can be performed depending on the clinical situation at hand, such as the measurement of potential VA and the use of binocular indirect ophthalmoscopy (BIO), etc. Among other currently available ancillary exams for retinal evaluation, optical coherence tomography (OCT) is the least invasive exam offering the most information on the macula(1).
OCT technology allows for observation of the retinal structures (ganglion cells, nerve fiber layer, photoreceptors), including the optic disc and fovea, and thus provides important diagnostic information for accurate evaluation of the macular area(2).
The current study evaluates the ability of spectral domain optical coherence tomography (SD-OCT) to detect pre- and postoperative macular alterations, as well as the variation in the central foveal thickness (CFT) in patients undergoing cataract surgery, and correlates these findings with age, sex, and the presence or absence of concomitant ophthalmic pathologies.
METHODS
This study was approved by the Federal University of Paraná Research Ethics Committee, and only included patients with a diagnosis of senile cataract who had not previously undergone eye surgery and who attended all follow-up exams. All patients signed an informed consent form. This prospective, analytical, observational, longitudinal study included patients of the Unified Health System scheduled for phacoemulsification and intraocular lens (IOL) implantation.
Preoperative evaluation included VA (logMAR), refraction, biomicroscopy, applanation tonometry, and BIO. The same evaluation was repeated postoperatively at 1, 30, and 180 days. The OCT exam was performed on all patients using a Spectralis OCT (Heidelberg Engineering GmbH, Heidelberg, Germany) within 5 h preoperatively and postoperatively at 7, 30, 60, 90, and 180 days.
All patients were preoperatively administered tropicamide 1%, moxifloxacin 5 mg/ml, and diclofenac sodium 0.1%, with postoperative administration of moxifloxacin hydrochloride 5.45 mg/ml combined with disodium phosphate dexamethasone 1.10 mg/ml and ketorolac tromethamine 0.4%. All surgeries were performed by experienced surgeons.
The results were evaluated in their totality and further analyzed in groups according to age, sex, and with reference to any concomitant pathologies.
To compare the groups with respect to the CFT variable, profile analysis was employed. The repeated measures model (ANOVA) was used to compare patients with no other ophthalmic-related pathologies (NOO). The nonparametric Mann-Whitney test was used to compare the groups defined by atrophic and exudative AMD, and assessment of the homogeneity of variance was performed using Levene’s test. P values of <0.05 were considered statistically significant. Data were analyzed using the computer program SPSS v.20.0 (IBM Corporation, Armonk, NY, USA).
RESULTS
We evaluated 98 eyes of 98 patients (63 females). There were no intraoperative complications, and all IOLs were implanted in the capsular sac. The patients’ ages ranged from 43 to 90 years, with a mean of 71.4 years. The initial and final mean logMAR VA were 0.6 and 0.1, respectively.
Sixty of the 98 eyes evaluated (61.2%) presented with NOO, 21 (21.4%) were patients with diabetes mellitus (DM), 10 (10.2%) presented age-related macular degeneration (AMD), three (3.1%) presented epiretinal membrane (ERM), and four (4.1%) presented glaucoma associated with cataract.
In the 60 NOO eyes, the mean pre- and postoperative logMAR VA were 0.6 and 0.1, respectively, which were statistically significantly different (p<0.001). As shown by OCT, the mean pre-op CFT of 222 µm progressively increased up to 60 days postoperatively, when it reached a mean of 227.2 µm (p<0.001). Thereafter, the CFT decreased through to the final OCT examination, when it reached a mean of 224.9 µm (Figure 1). Neither cystoid macular edema (CME) nor Irvine-Gass Syndrome were observed. Similar CFT values were observed in the four eyes with glaucoma associated with cataracts.
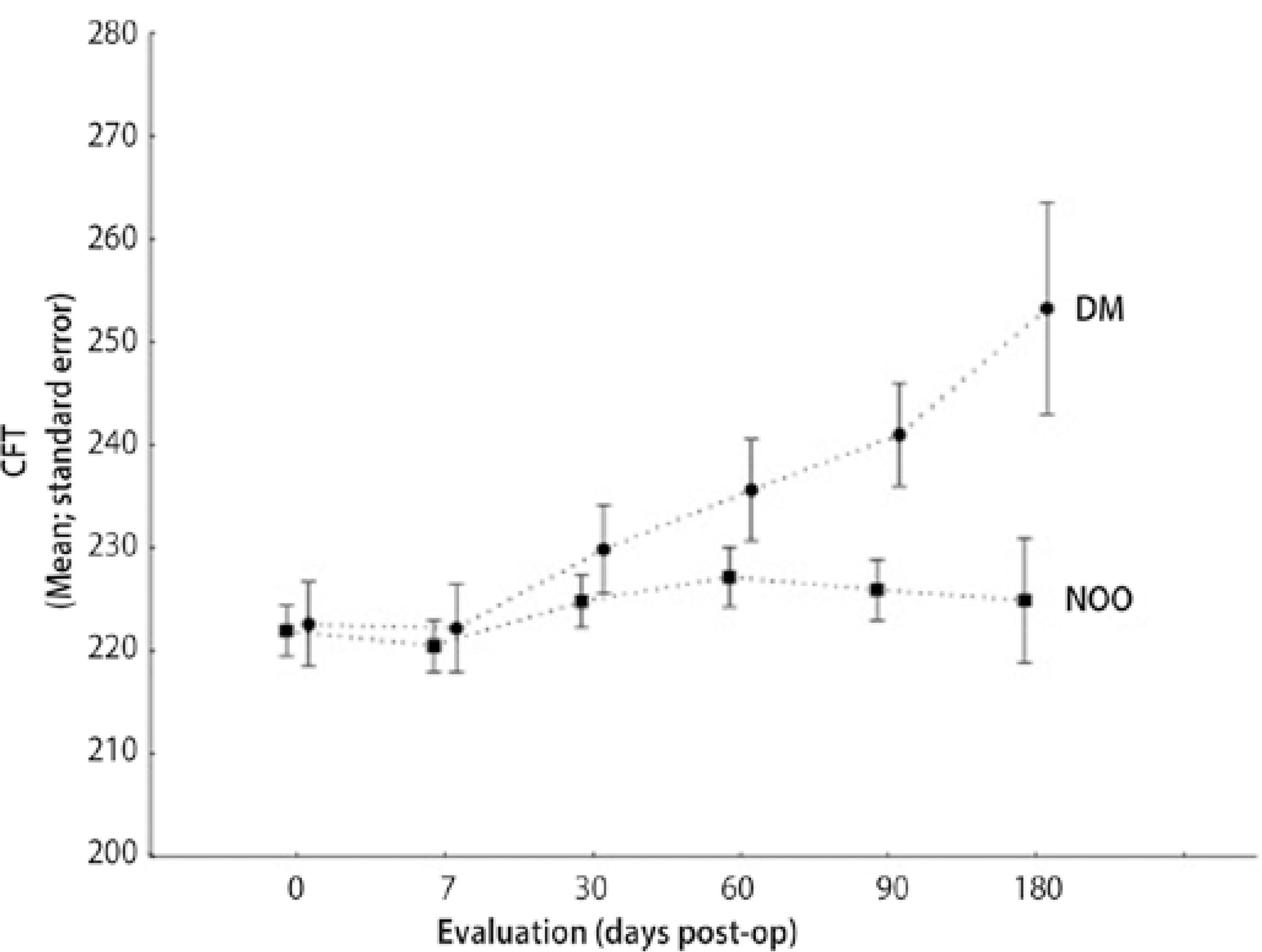
Figure 1 Distribution of central foveal thickness (CFT) in microns, by postoperative days, in the diabetes mellitus (DM) and no other ophthalmic-related pathologies (NOO) groups.
The 21 eyes of the DM patients presented mean pre- and postoperative VA of 0.5 and 0.1, respectively. Starting from the 30th day post-operatively, the mean CFT was statistically significantly different between the NOO and diabetic patients (p<0.001) (Figure 1), suggesting a difference in the progression of the DM and NOO cases in terms of the CFT. Unlike in the patients with NOO pathologies, there was a progressive increase in the mean CFT from the preoperative OCT examination (222.6 µm) to the final exam (253.3 µm).
The preoperative BIO exam showed that among the 21 eyes of patients with DM, 14 had no ophthalmoscopic signs of diabetic retinopathy (DR), and seven were categorized as eyes with mild non-proliferative diabetic retinopathy (NPDR).
However, in the preoperative OCT examination, one of the 14 eyes that was clinically defined as not having DR was actually found to have mild DR. Of the seven eyes with clinical signs of DR, the preoperative OCT exam showed that three had mild NPDR and four had moderate NPDR. Still, none had macular edema (ME) as assessed by OCT. After 180 days of follow-up, three eyes without DR progressed into mild NPDR without ME, and two eyes with moderate NPDR without ME progressed into moderate DR with ME (Table 1).
Table 1 Distribution of eyes in patients with diabetes mellitus by DR classification * and time (days) of follow-up
| Without DR | Mild NPDR w/o ME | Moderate NPDR w/o ME | Moderate NPDR w/ ME | Total | ||
|---|---|---|---|---|---|---|
| Preoperative | 13 | 4 | 4 | 0 | 21 | |
| Postoperative (180 days) | 10 | 7 | 2 | 2 | 21 | |
DR= diabetic retinopathy; NPDR= nonproliferative diabetic retinopathy; w/o= without, w/= with; ME= macular edema.
*= International clinical diabetic retinopathy and diabetic macular edema disease severity scales.
Four eyes presented with a clinical diagnosis of AMD using BIO (one atrophic, three exudative). The preoperative OCT exam identified four additional patients with atrophic AMD and two with exudative AMD. Table 2 shows the distribution of patients with AMD according to pre- and postoperative VA scores. The CFT scores of both types of AMD were also evaluated. The subset of eyes with atrophic AMD showed low variation in CFT, reaching maximum values on the 7th day post-op (mean = 181.25 µm), while the subset with exudative AMD reached the maximum CFT on the 30th day post-op (mean = 386.25 µm) (Figure 2).
Table 2 Distribution of eyes of patients by VA (logMAR) and type of age-related macular degeneration
| Group | Pre-operative VA | Post-operative VA | Difference |
|---|---|---|---|
| Dry (n=5) | 0.76 ± 0.40 | 0.70 ± 0.30 | -0.58 ± 0.37 |
| Wet (n=5) | 0.94 ± 0.38 | 0.64 ± 0.50 | -0.30 ± 0.27 |
| P value* | 0.548 | 0.095 | 0.309 |
VA= visual acuity
*= nonparametric Mann-Whitney test, p <0.05.
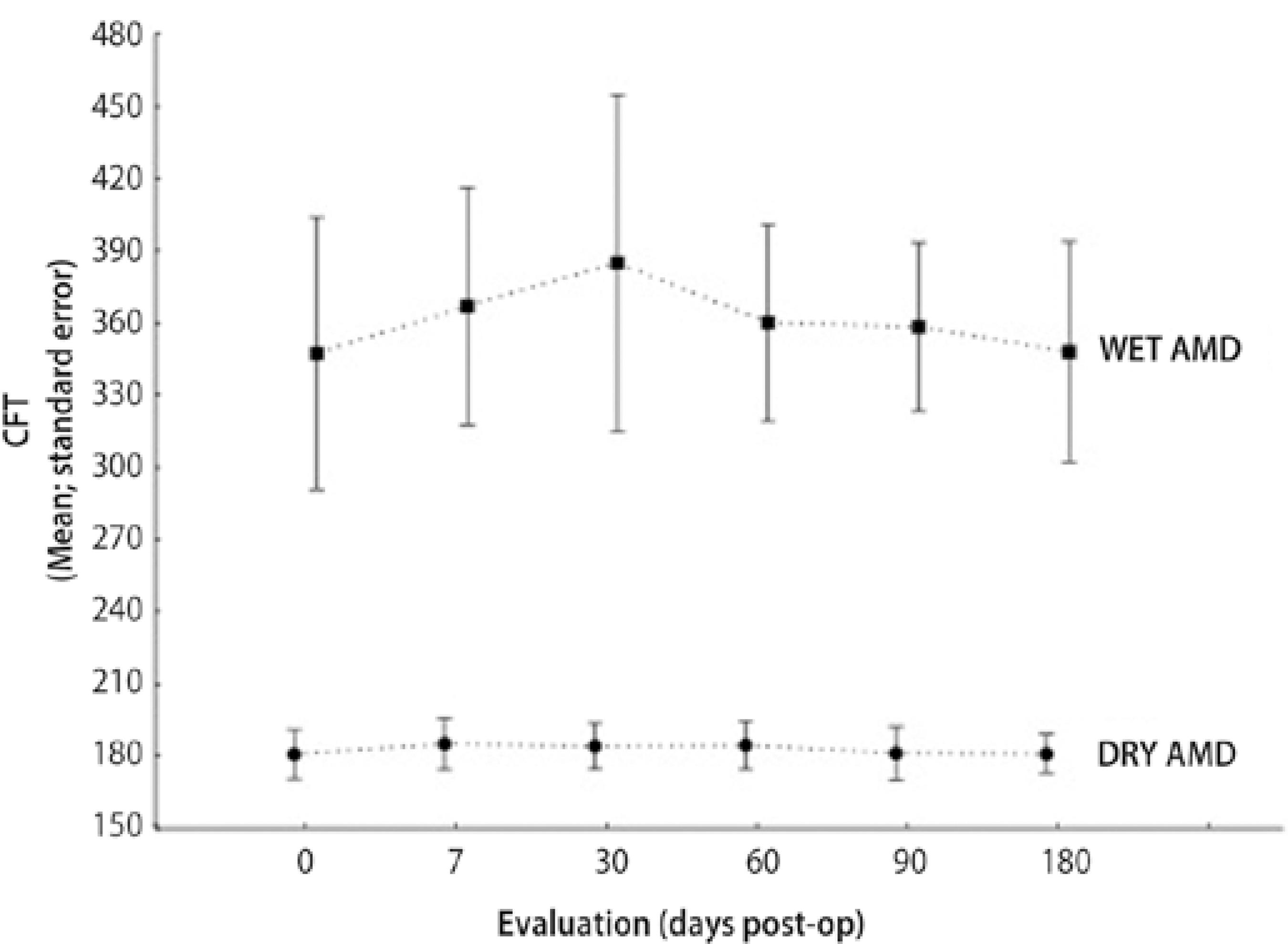
Figure 2 Distribution of central foveal thickness (CFT) in micrometers, by postoperative days and type of age-related macular degeneration (AMD).
We also compared the VA and CFT scores between male and female NOO patients; no significant difference was found between the sexes. Table 3 shows that male patients had a higher mean CFT than female patients at all time points, with statistical significance.
Table 3 Distribution of mean CFT (µm) in patients with no other ophthalmopathies by follow-up length (days) and sex
| Group | CFT 0 | CFT 7 | CFT 30 | CFT 60 | CFT 90 | CFT 180 |
|---|---|---|---|---|---|---|
| Female (n=41) | 219.8 ± 14.9 | 217.5 ± 14.9 | 221.5 ± 15.2 | 224.2 ± 17.7 | 221.7 ± 16.2 | 220.6 ± 15.8 |
| Male (n=19) | 226.7 ± 24.9 | 227.2 ± 25.1 | 232.1 ± 26.5 | 233.7 ± 27.3 | 235.2 ± 26 | 234.2 ± 26.4 |
| P value * | 0.017 | 0.012 | 0.009 | 0.037 | 0.020 | 0.022 |
CFT= central foveal thickness
*= Levene's test.
The VA and CFT scores were also compared between patients 70 years and younger and patients over 70 years. The mean pre- and postoperative VA scores differed very little between the two groups, while the mean CFT in the group aged 70 years or younger was lower than in the group over 70 years in all follow-up tests. In terms of the CFT variable, the progression of cases in patients 70 years and younger was statistically significantly different than in patients over 70 years (p=0.016).
Three eyes had preoperative ERM that was only detected after the OCT exam. The first case showed no improvement of VA with cataract surgery, with a preoperative CFT of 196 µm and a 180-day post-operatively CFT of 179 µm. The second case had a pre- and postoperative VA of 0.1 and 0.3, respectively. The preoperative CFT was 614 µm, and the final CFT was 606 µm. Unlike the two previous cases, the third patient had a preoperative VA of 0.3 and CFT of 424 µm, and postoperative VA of 1.0 and CFT of 449 µm.
Of the 98 eyes, OCT preoperatively diagnosed macular disease in 21 eyes (21.4%), while BIO diagnosed maculopathies in just 11 (11.2%).
DISCUSSION
The inclusion of OCT exams as part of the routine preoperative tests for intraocular surgeries is imminent, driven by its noninvasive nature and greater accuracy in the diagnosis of macular diseases. Additionally, as this equipment becomes more popular, it will subsequently become less costly. Compared to other tests used for the diagnosis of macular diseases, such as retinal angiography or electroretinography, OCT is not only safer, it is more precise and practical.
In the present study, the preoperative BIO exam detected macular alterations in 11 eyes (11.2%): seven with DR and four with AMD. In addition to those 11 eyes with BIO-detected macular changes, OCT revealed 10 additional eyes with maculopathies (six AMD, one mild NPRD, and three ERM), with a total of 21 eyes (21.4%). In addition to greater accuracy during preoperative evaluation, OCT also allowed for detailed monitoring of the macula in the postoperative period, thus revealing the reason for the worsening vision in some eyes, especially in diabetic patients.
The difference observed between the BIO examination and OCT may be due to the inaccuracy of the pre-op BIO examination performed by the clinician, who is not a retinal specialist and may not have noticed the subtle macular changes, especially when lens opacification is present. On the other hand, seeing a retina specialist is not routine as part of the preoperative examination for cataract surgery. Therefore, the findings presented here may be very similar to what happens in the real world of ophthalmic practice. Additionally, the near-infrared light in OCT allows for more precise observation of the retina.
Besides the diagnostic capabilities of OCT, the measurements of retinal thickness, especially the CFT, are important in the follow-up of operated eyes. In our study, a progressive increase was observed in the CFT of the NOO group from the 7th to the 60th day after surgery, which then began decreasing up to the 180th day post-op, when the values approximated those obtained in the preoperative examination. However, male patients showed a decreased CFT only 180 days after surgery, whereas female patients showed a decrease in CFT values from the 90th day post-operatively.
Similarly, Corrêa et al.(2)evaluated the CFT of 62 eyes with no other associated pathologies by SD-OCT at pre-op, 1 week, and 1 month following cataract surgery, and observed a continuous increase in the CFT until 30 days post-operatively.
The incidence of clinically significant CME is 0.6-2.6%; however, the incidence of subclinical CME is uncertain(3,4). Using OCT, Bélair et al.(5) showed that the incidence of CME in patients without other eye pathologies was 4% and 0% at 30 and 60 days post-operatively, respectively. However, there was no statistically significant difference between the two evaluated time points.
Other studies showed that the incidence of subclinical CME diagnosed by OCT varies between 0-22%(4,6,7). No cases of subclinical CME or Irvine-Gass syndrome were observed in our study. The discrepancy in the incidence of subclinical CME can be explained by variations in the inclusion and exclusion criteria, and by different medication protocols employed in the postoperative period of different studies(6).
Among the 21 eyes in patients with DM, who underwent phacoemulsification in the present study, seven presented signs of DR via preoperative BIO exams. Preoperative OCT not only found that one eye thought to be without NPDR actually had mild NPDR, but also helped to better classify the remaining seven eyes with DR (three with NPDR and four with mild-to-moderate NPDR without ME). OCT also showed that after 180 days post-op, three eyes without DR developed mild NPDR without ME, and two eyes with moderate NPDR without ME developed moderate DR with ME.
Cataract surgery has the potential to induce inflammatory and mechanical changes in vitreoretinal structures, thus causing macular thickening with changes to VA(8), probably due to damage to the blood-retinal barrier(9,10).
Jun et al.(11) evaluated 637 OCT exams (Stratus) in patients with macular diseases and CFT scores less than 252 µm. They found that 25% of the patients had NPDR. Although 75% of the patients with diabetes had clinical reports of ME, their OCTs were normal on the day of examination. While this finding can be explained by therapeutic factors, only one patient underwent laser photocoagulation in the 3 months preceding the study. Thus, diabetic patients may have ME with no increase in CFT.
The incidence of ME found via OCT testing is 22% in the eyes of diabetic patients undergoing cataract surgery(12). On the other hand, DR is known to progress in 10-30% of patients undergoing phacoemulsification(7,13-16). In these studies, the main factor responsible for the progression of DR was the degree of DR at the time of phacoemulsification(15,17,18).
Previous studies have shown that diabetic ME progresses in 2040% of eyes undergoing cataract surgery, although swelling disappears spontaneously in most of these eyes(19-21).
In 2009, Hayashi et al.(22)performed OCT (Stratus) in diabetic patients who underwent cataract surgery with IOL implantation. The final sample was 34 eyes without DR and 34 eyes with DR. The OCT was performed to obtain the CFT 1 day before surgery and 3, 6, and 12 months postoperatively. They noted an increase in the CFT in both groups after performing phacoemulsification, although this increase was much more significant in the group with DR, as was also shown in our study.
In another study, Biró et al.(23) compared the CFT of 18 eyes of diabetic patients with 36 eyes of nondiabetic patients using SD-OCT preoperatively and at 1, 7, 30, and 60 days post-op, with the contra-lateral eye acting as the control. Patients with any other ophthalmic pathologies were excluded, as well as those with severe NPDR or with proliferative DR. A significant increase was noted in the CFT in both the groups with DM and without DM as compared with their respective controls. Additionally, there was a significant increase in the CFT in both groups when compared with the preoperative examination, and in the exams on days 7, 30, and 60 post-op. Similar findings were observed in our diabetic patients, who showed a gradual increase in CFT up to the last day of assessment, while the patients with no concomitant eye pathologies had a peak in their CFT 60 days post-op, which was followed by a decline.
In our study, only one patient presented with atrophic AMD and three with exudative AMD, which had all already been clinically diagnosed prior to surgery. In the pre-op OCT exams, four more cases of atrophic AMD and two more cases of exudative AMD were diagnosed, thus showing the importance of the OCT exam as part of the preoperative assessment for cataract surgery. The CFT for the exudative AMD group increased up to the 30th day post-operatively, reaching 386.25 µm, and subsequently regressed back to their approximate pre-op values. The subset with atrophic AMD had virtually no changes in their CFT, which peaked on day 7 after surgery (121.25 µm).
With regard to AMD, the importance of a preoperative OCT exam is even more evident for patients undergoing cataract surgery, since of the 10 patients in our sample, six were diagnosed only after the preoperative OCT. An increase was observed in the CFT for both types of AMD, which peaked on the seventh day after surgery, although this returned to similar values to the preoperative period by the final examination for both types. Clearly, there is a large difference between the CFT values of patients with atrophic and exudative AMD, since they have different clinical courses.
In 2012, Monestam et al.(24) showed that patients with clinical signs of AMD at the time of cataract surgery have a lower gain in vision than patients without AMD symptoms. That said, for patients with AMD, cataract surgery is still beneficial, since the visual result 10 years after surgery is better than preoperative vision. In our study, we observed no statistically significant difference relative to the VA in patients with atrophic or exudative AMD, pre- or postoperatively.
As for CFT in regards to sex, male patients with no other eye pathologies in the present study had higher CFT than females at all evaluation time points (p<0.05). Schuman et al.(25) and Gupta et al.(26) also showed that males present higher CFT values than females.
In this study, patients over the age of 70 years had higher CFT than those 70 years and younger. Both age groups presented an increase in CFT up to 60 days post-op, and thereafter, there was a subsequent decrease up to the final day of follow-up. Therefore, it was statistically shown that the development of cases in patients up to the age of 70 years is different to those over the age of 70 years. In 2013, Gharbiya et al.(6) reported that there was no significant relationship between age and CFT, with p=0.56. However, Gupta et al.(26) obtained different results, with older patients presenting a lower CFT, which decreased by 0.38 µm per year.
Finally, is important to point out that although OCT examination may offer a better evaluation of fundus changes, showing additional details, it is not a substitute for adequate clinical evaluation made with BIO.
CONCLUSION
OCT examination was able to diagnose macular diseases during preoperative assessment for phacoemulsification and was more effective than BIO examination. Moreover, OCT evaluated CFT scores in patients with DR, showing a progressive increase up to 180 days postoperatively. It also showed that CFT is higher in males than in females, and in patients aged over 70 years than in those 70 years and younger.
Our results demonstrated that OCT is a reliable and useful preoperative examination for patients undergoing cataract surgery.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

