INTRODUCTION
Bilateral acute iris transillumination (BAIT) is a very rare condition characterized by the bilateral acute loss of iris pigment epithelium, iris transillumination, pigment showering, persistent mydriasis, and occasional increased intraocular pressure (IOP)(1,2). Patients with BAIT generally present with acute ocular pain, photophobia, and red eyes(1), which are also observed in patients with iridocyclitis. Furthermore, the circulating pigment particles in the anterior chamber may be confused with the inflammatory cells seen in patients with iridocyclitis. Therefore, the presenting symptoms and findings of BAIT may result in a misdiagnosis of acute iridocyclitis. We report a case of BAIT in a patient who was initially misdiagnosed with iridocyclitis and treated with corticosteroid therapy.
CASE REPORT
A 30-year-old male was referred to our clinic to seek another opinion for his diagnosed iridocyclitis, which was unresponsive to treatment. Two months previously, he had been admitted to another clinic with acute bilateral ocular pain, severe photophobia, and red eyes. He was diagnosed with iridocyclitis and treated with topical and systemic corticosteroids. However, his signs and symptoms did not improve. The patient also had a history of upper respiratory tract infection and use of the systemic cefazolin 3 months previously. On admission, his best-corrected visual acuity was 20/20 in both eyes. Slit-lamp examination revealed bilateral conjunctival hyperemia, 1+ circulating pigment in the anterior chamber, diffuse iris transillumination, pigment dusting on the anterior lens capsule, and mydriatic and distorted pupils (Figures 1 A, B and 2 A, B). There were no inflammatory keratic precipitates on the corneal endothelium or inflammatory cells in the anterior vitreous of either eye. Corneal sensation was intact in both eyes. Gonioscopy showed heavy pigment deposition in the trabecular meshwork bilaterally (Figure 2 C, D). There was no evidence of posterior iris bowing or peripheral anterior synechiae on the gonioscopy. IOP was 20 mmHg in the right eye and 18 mmHg in the right eye. The fundus examination was normal in both eyes. The patient had undergone a complete laboratory evaluation for uveitis in the other clinic. The results of those tests, including erythrocyte sedimentation rate, complete blood cell count, biochemistry, urinalysis, venereal disease research laboratory test, intradermal purified protein derivative test, and computed tomography of the chest, were normal. Human leukocyte antigen-B51 (HLA-B51) and HLA-B27 were negative.
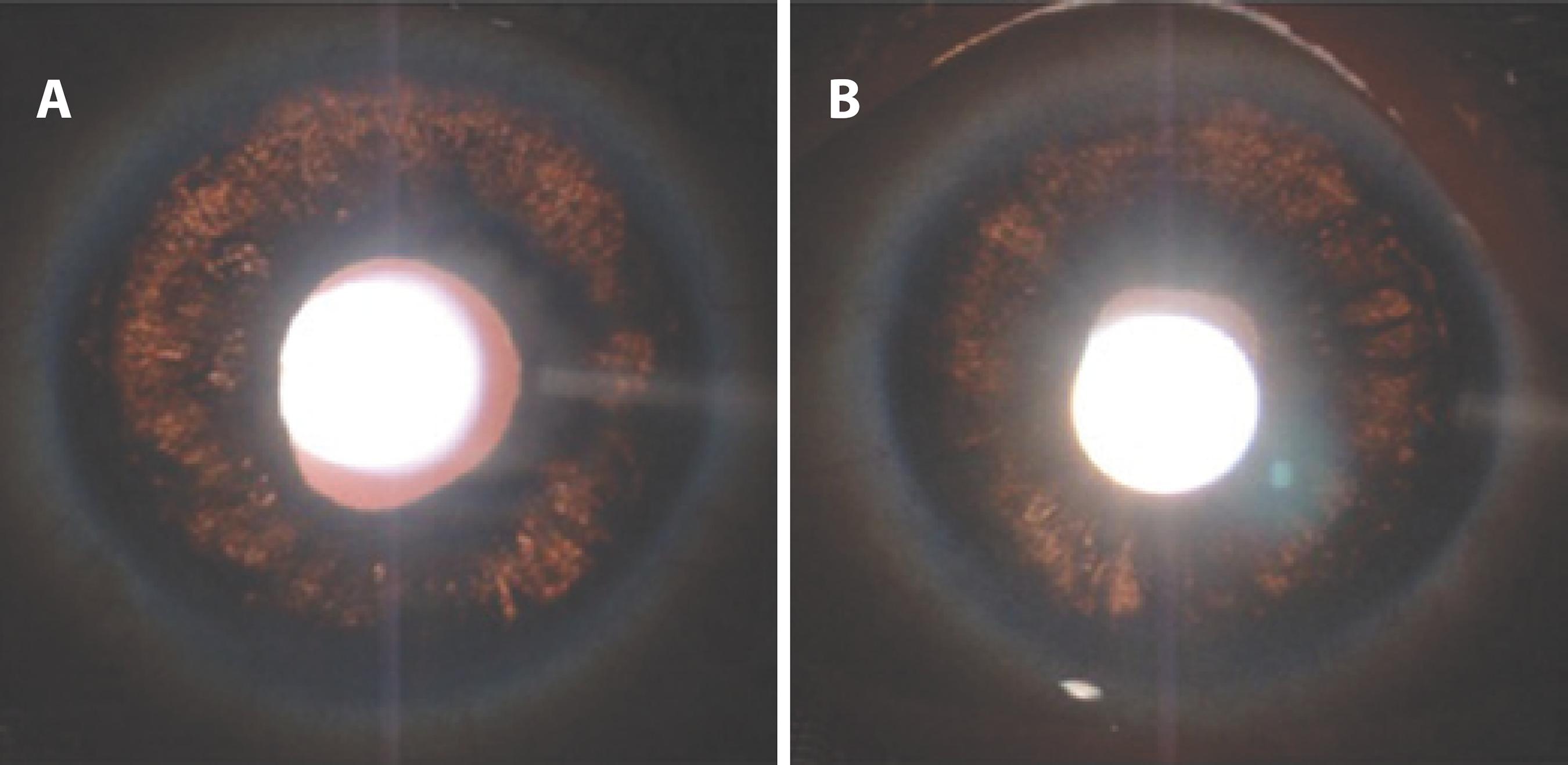
Figure 1 Slit-lamp photographs of right (A) and left (B) eyes showing diffuse iris transillumination defects using the retroillumination technique. The photographs were taken without pharmacologic dilation of the pupils.
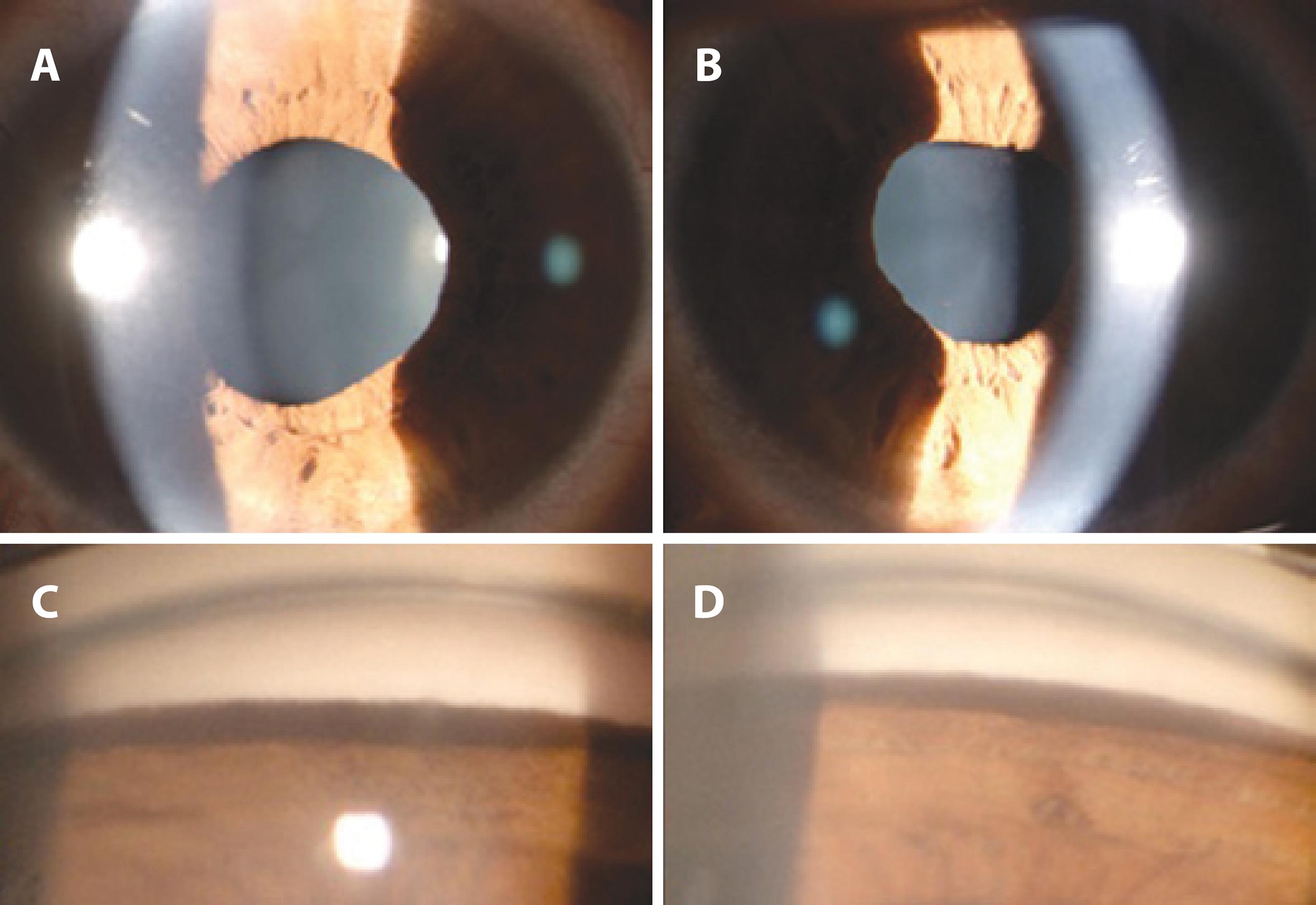
Figure 2 Slit-lamp photographs of right (A) and left (B) eyes showing mydriatic, distorted pupils with poor response to light, and a small amount of pigment dusting on the anterior lens capsule. Gonioscopy of right (C) and left (D) inferior angles showing heavy inferior trabecular meshwork pigmentation.
On admission to our clinic, the patient was using topical prednisolone acetate 1% 8 times a day, topical cyclopentolate 1% twice a day, and a fixed carbonic anhydrase inhibitor/beta blocker combination. The cyclopentolate was discontinued, and the prednisolone was tapered and discontinued after a month. The patient remained stable for the rest of his 3-month follow-up, without the need for steroid treatment. During follow-up examinations, IOP did not increase, the pigment dispersion in the anterior chamber decreased, and the iris transillumination defects remained stable.
DISCUSSION
Iris atrophy with and without transillumination may be caused by several diseases, such as viral iridocyclitis, pigment dispersion syndrome (PDS), pseudoexfoliation syndrome, Fuchs uveitis syndrome (FUS), Vogt-Koyanagi-Harada disease, acute angle-closure glaucoma, ocular trauma, bilateral acute depigmentation of the iris (BADI), and BAIT(1-5).
The most common differential diagnosis in pigment dispersion and iris transillumination is PDS, which typically occurs in young myopic adults. It is usually asymptomatic and characterized by posterior bowing of the iris, Krukenberg’s spindle, and slit-like, radial, midperipheral transillumination defects(6), none of which were detected in our patient.
Herpes simplex and cytomegalovirus may cause unilateral iridocyclitis with sectorial/diffuse iris atrophy and transillumination. Although an aqueous tap for polymerase chain reaction (PCR) analysis is required for a definite diagnosis, negative results do not exclude a viral etiology(7).We were unable to obtain aqueous humor for viral analysis, because the patient did not consent to the procedure. However, symmetrical and bilateral involvement, lack of keratic precipitates, and atonic pupils with compromised reaction to light helped us to differentiate BAIT from viral uveitis.
FUS is a chronic, asymptomatic, low-grade unilateral uveitis characterized by diffuse, stellate, and medium-sized keratic precipitates and iris stromal atrophy, with or without heterochromia, and without posterior synechiae(8), which were also not detected in the present case.
Our patient displayed the clinical findings of BAIT, including acute onset of severe photophobia and red eyes, bilateral severe transillumination of the iris, pigment showering in the anterior chamber, a mydriatic and distorted pupils, and increased IOP. This condition should also be differentiated from BADI, which has a more benign course and shorter duration of pigment discharge, a lower incidence of elevated IOP, which is transient, and reversibility of iris changes in some patients(5). Both conditions have a common etiology but the pigment discharge seems to be only from the iris pigment epithelium in BAIT and from the iris stroma in BADI. The features that differentiate BADI from BAIT are depigmentation of the iris without transillumination defect and unaffected pupils(1).
BAIT may also masquerade as iridocyclitis, as in the case of our patient, who was referred for evaluation of bilateral acute iridocyclitis. On our initial examination, he had no inflammatory keratic precipitates on the corneal endothelium but had all of the clinical findings of BAIT. Therefore, we ruled out acute iridocyclitis.
Although the exact etiopathogenesis of BAIT remains unclear, several publications have reported a relationship between BAIT and systemic use of moxifloxacin(2) and clarithromycin(9), upper respiratory tract infections(1), and a toxic effect following fumigation(10). Our patient had a history of upper respiratory tract infection and use of systemic cefazolin 3 weeks before the onset of his symptoms. It is difficult to establish which of those factors was the cause of BAIT. Tugal-Tutkun et al.(1) reported 26 patients with BAIT, 19 of whom had a history of upper respiratory tract infection and use of systemic antibiotics, including moxifloxacin, ampicillin/sulbactam, amoxicillin/clavulanate, trimethoprim/sulfamethoxazole, cefixime, and penicillin V. However, they concluded that the relationship between BAIT and systemic antibiotic use was coincidental, because there are no reported ocular adverse effects related to the topical use of these antibiotics, in particular moxifloxacin, which has efficient ocular penetration. We use moxifloxacin in the anterior chamber for prophylaxis of endophthalmitis after cataract surgery, and we have not encountered any cases of BAIT associated with its use. Therefore, it appears that BAIT in the present case was triggered by the virus that caused the upper respiratory tract infection.
In conclusion, BAIT should be differentiated from other diseases causing pigment dispersion into the anterior chamber and from iridocyclitis. It is important to make a correct differential diagnosis of BAIT from anterior uveitis to avoid the unnecessary use of corticosteroids and detailed investigation for uveitis. Early diagnosis of this condition is also important because of the risk of marked increases in IOP.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

