INTRODUCTION
Retinoschisis is the term used to describe an abnormal separation of the retinal layers. It can be congenital, acquired (also known as degenerative or senile), or secondary (associated with myopia, trauma, sickle cell anemia, and other diseases)( 1 ).
Senile retinoschisis (SR) was first described in 1933 by Bartels( 2 ). In most cases, it is an asymptomatic bilateral disease with a prevalence between 1.65% and 7.00% among individuals aged >40 years, and it usually affects the peripheral retina( 3 ). Retinal detachment usually occurs between the external plexiform layer and the inner nuclear layer. The associated complications are rare and include enlargement of the retinoschisis area, retinal tears, retinal detachment (RD) in the area of retinoschisis, and progressive and symptomatic RD. Patient management is controversial. In general, the management of the disease and its complications is conservative because macular involvement is rare, spontaneous progression is not frequent in the natural history of the disease, and prophylactic treatment can pose risks( 4 ).
Approximately 25% of the patients develop retinal holes. Tears in several retinal layers that are close to each other increase the associated risk of RD, which is observed in up to 40% of cases when both leaflets are ruptured( 1 ).
Progressive and symptomatic RD associated with SR is rare, occurring in approximately 0.05% of the cases( 5 ), and it is the only complication in which immediate treatment is indicated. Scleral buckle, laser demarcation photocoagulation, and posterior vitrectomy are treatments described in the literature. Air injection associated with drainage of the subretinal liquid by equatorial sclerotomy was described by Sulonen et al.( 6 ) in a case of RD associated with SR. Moreover, Ambler et al.( 7 ) reported a series of six cases in which intraocular gas injection was associated with external drainage of the sub retinal fluid in the management of SR-associated RD and one re-detachment was observed after this procedure. Pneumatic retinopexy (PR) using air as the buffer associated with cryotherapy was previously described in a case report on this condition( 8 ). However, to the best of our knowledge, the present case report is the first description in the literature on the use of PR using C3F8, without external drainage of subretinal liquid, that allowed the successful management of SR associated with progressive RD.
CASE REPORT
A 49-year-old male patient experienced floaters and flashes followed by low progressive vision in the right eye (RE). The patient experienced visual acuity (VA) of count fingers at a 50 cm distance in the RE and 1.0 in the left eye (LE). Fundoscopy examination indicated retinal detachment involving the macula with two tears in the inner and outer retinal layers in the SR area in the superior temporal quadrant of the RE, between the 10 o'clock and 12 o'clock positions (Figure 1 A). The patient had SR in the superior temporal quadrant of the LE. (Figure 1 B). Vitreous detachment was not observed in either eye.
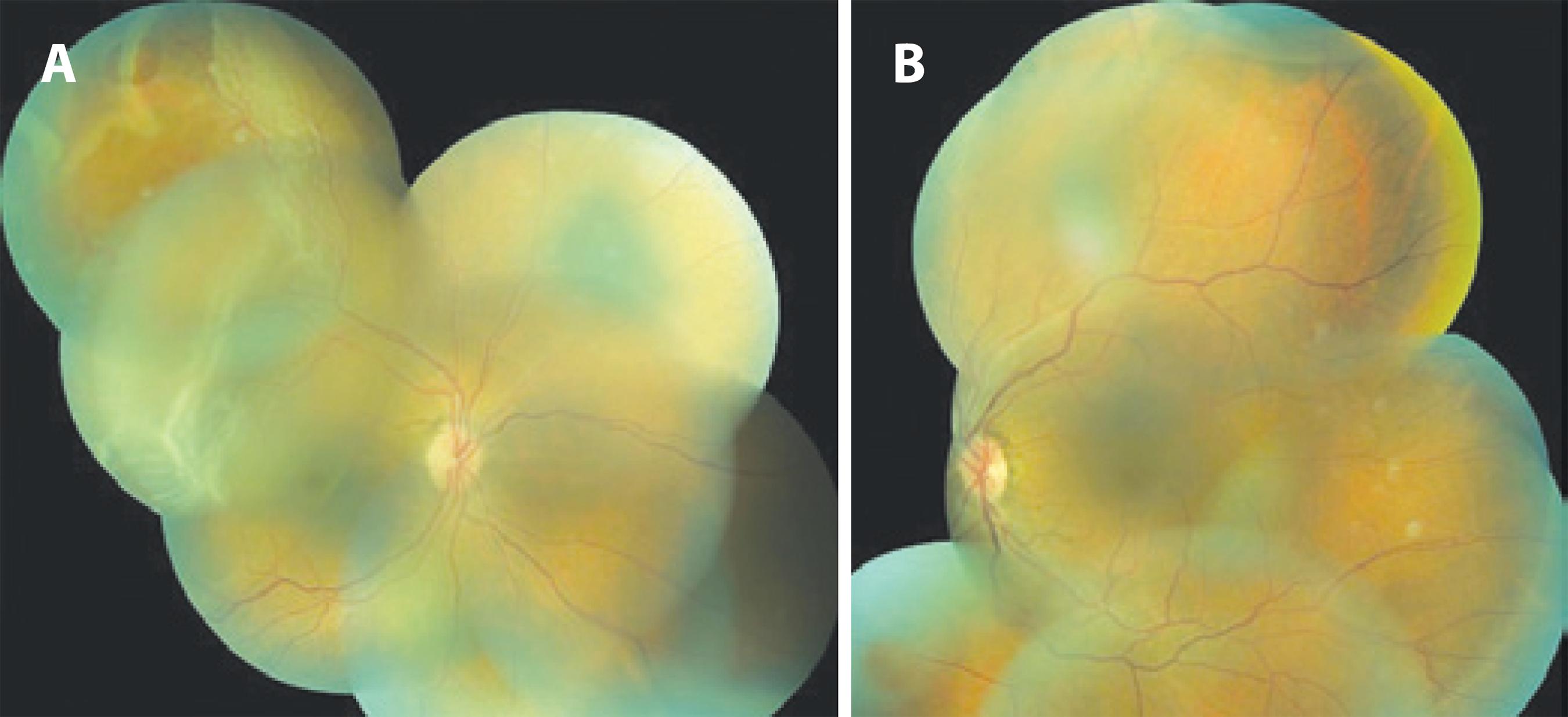
Figure 1 A) Retinal detachment with tears due to senile retinoschisis in the superior temporal quadrant of the right eye; B) Senile retinoschisis in the superior temporal quadrant of the left eye.
PR with injection of 0.3 mL of perfluoropropane (C3F8) was the intervention chosen and the patient's head was inclined upwards slightly over the left shoulder in the sitting or supine positions, so that the intraocular gas bubble would position itself between the 10 o'clock and 12 o'clock positions, enabling closure of the tears.
The procedure was performed in an outpatient setting under local anesthesia and aseptic technique. After prophylactic anterior chamber paracentesis, pure C3F8 was injected into the lower temporal region, 4 mm from the limbus, with a 27-gauge needle. Five min after this procedure, fundoscopy showed no signs of occlusion of the central retinal artery. In addition, the intraocular pressure was within normal limits, similar to the values obtained in the follow-up consultations during outpatient return visits. Closure of the two tears was performed using argon laser two days after gas injection. On the 14th day post-PR, the patient's VA was 0.3 in the RE with retinal attachment (Figure 2). However, on the 23rdday post-PR, the patient progressed to sudden low vision and RD in the superior and inferior temporal quadrants. Due to the failure of first treatment and because a new tear was not clearly identified during fundoscopy in this instance, we chose to perform posterior pars plana vitrectomy and tear closure with C3F8. During vitrectomy, linear tear was observed in the inner retinal layer close to the 11 o'clock position, which had not been previously identified and blocked with laser, and this tear was probably responsible for the failure of the PR.
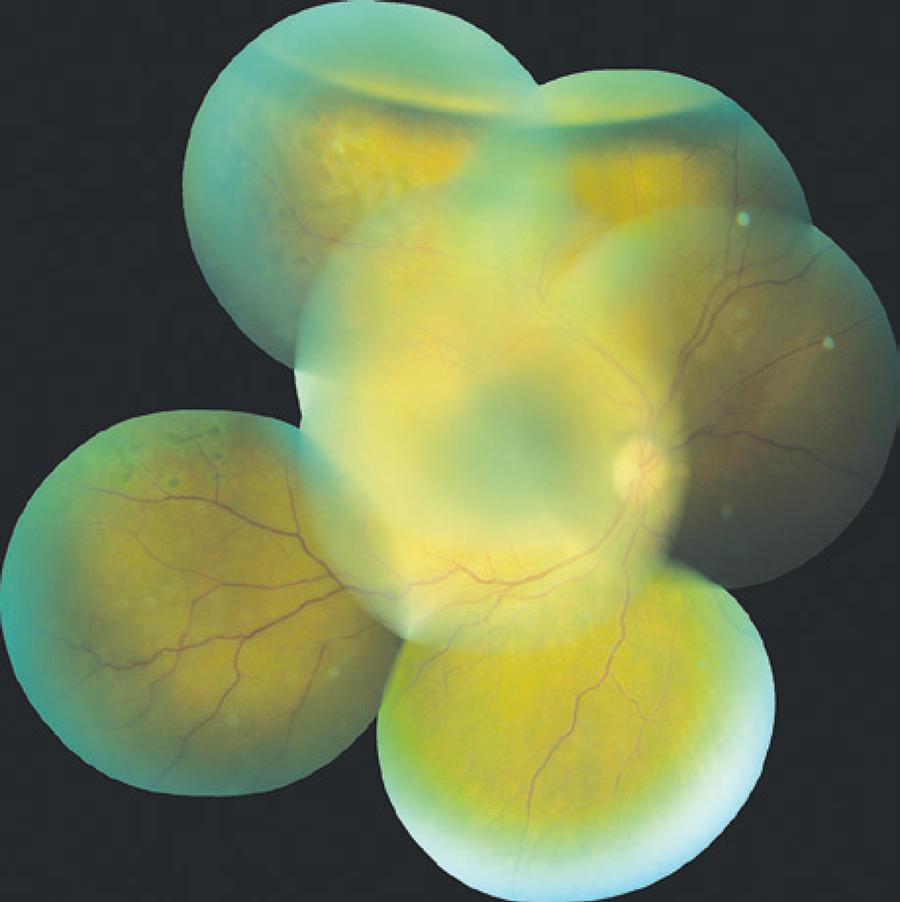
Figure 2 Retinal attachment in the right eye after treatment with the injection of 0.3 mL of perfluoropropane.
During outpatient follow-up at 6 months post surgery, the asymptomatic patient presented a VA of 0.3 in the RE and 1.0 in the LE with better correction. On fundoscopy, the patient had RD at the site of the senile retinoschisis in the superior temporal quadrant of the LE. Posterior involvement was observed after 4 months of progression, confirmed by retinography and optical coherence tomography (OCT), which clearly demonstrated that this complication involved retinal detachment and not simply progression of retinoschisis, although the tears were not evident. Considering the superior position and involvement of the contralateral eye, an interventional procedure (PR) was chosen (Figure 3).
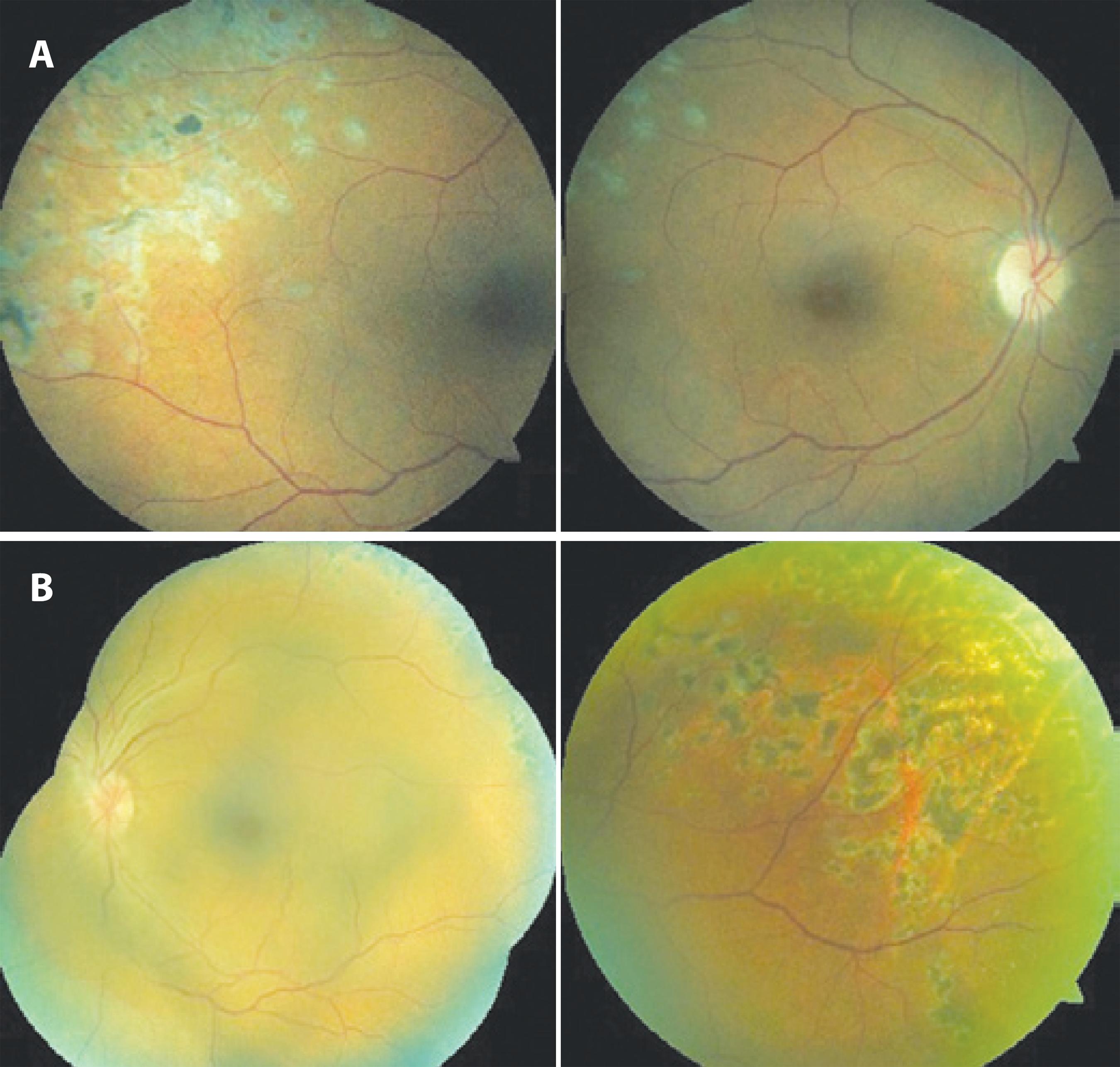
PR was performed according to a technique previously described for the LE, with argon laser photocoagulation in the area of retinoschisis. In this instance, the patient's head was inclined upwards slightly over the right shoulder. The patient progressed with retinal attachment in both eyes (Figure 4), showed no relapses associated with retinal detachment after 24 months of follow-up, and remains in periodic outpatient follow-up at our institution.
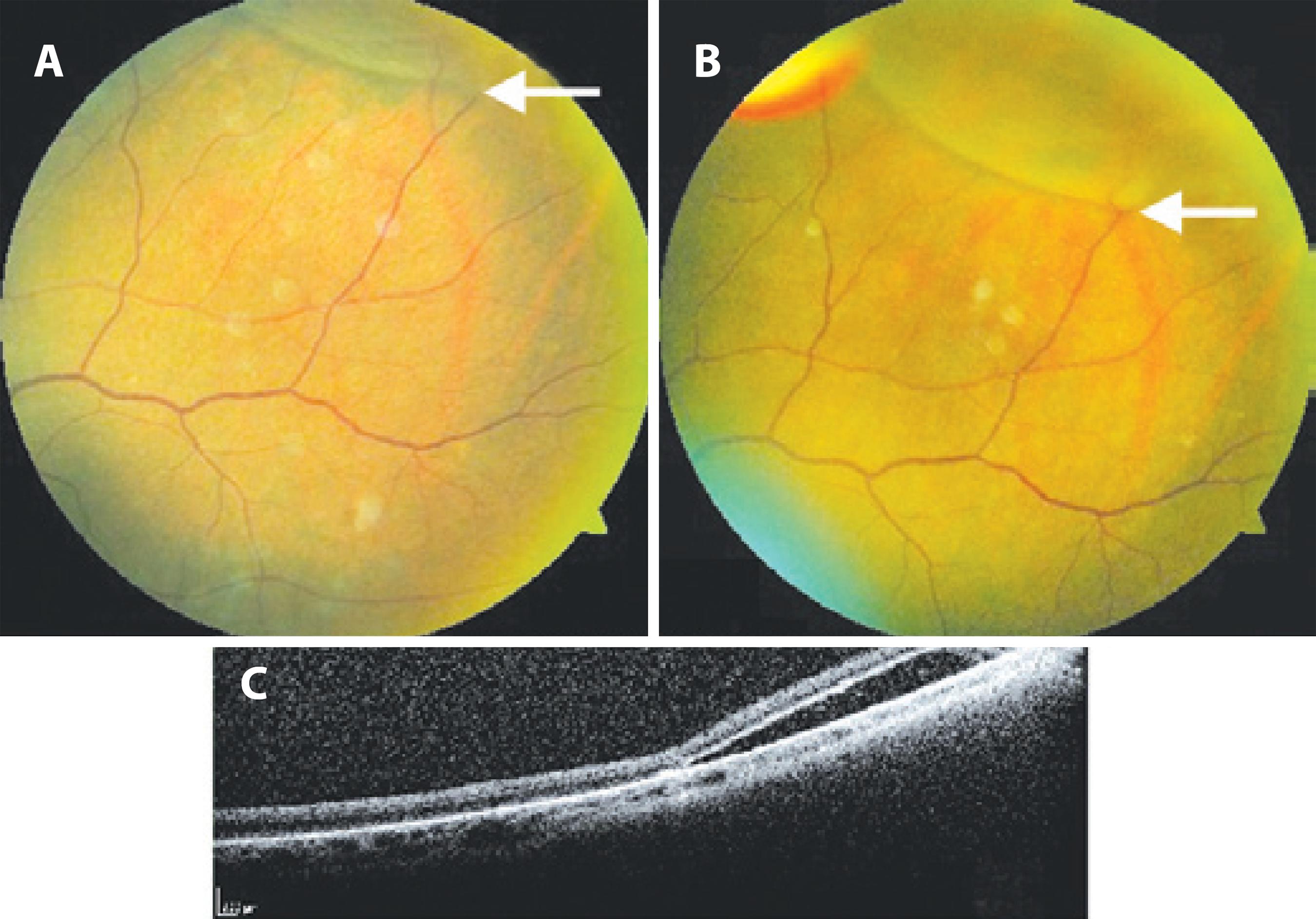
Figure 3 A and B) Retinal detachment in the area of retinoschisis in the superior temporal quadrant of the left eye with evidence of progression (note the retinal detachment approaching the vascular bifurcation indicated by the arrow in B); C) Optical coherence tomography with evidence of subretinal fluid.
DISCUSSION
PR is a well-established surgical technique for the treatment of some cases of RD. The procedure involves the induction of the closure of the retinal tear using cryotherapy or argon laser photocoagulation, in addition to intraocular gas injection, associated with the maintenance of an appropriate head position for closure of the retinal tear and resolution of the subretinal liquid. Small rhegmatogenous RDs caused by primary tears extending up to 1 h arc located between the 10 o'clock and 2 o'clock positions are the cases with classical indication for this type of treatment, when prognosis is more favorable. Previous studies have indicated that the success rate of PR is 53%100% for the cases with a single treatment. Phakic eyes appear to have better results compared with aphakic or pseudophakic eyes( 9 , 10 ).
Vrabec (2000)( 8 ) described a case where PR was used successfully as the sole treatment of SR-associated RD. The 52-year-old patient had retinoschisis extending from the 7 o'clock to 11 o'clock positions associated with RD dividing the foveal region and presented with symptoms since three weeks. Two tears were identified in the outer leaflet and three in the inner leaflet of the retinoschisis. After closure of the internal tears using cryotherapy, injection of 0.6 mL of air was performed followed by argon laser phococoagulation in the external tears after resolution of the subretinal liquid. The patient presented a final VA of 20/30 and retinal re-attachment with a 10-month follow-up. In the report, the author emphasizes the importance of the inner leaflet tears for the progression of RD in these cases, although, commonly, external tears are considered the most important in the development of SR-associated RD. This is the only case described in the literature with therapeutic success after PR using air as buffering agent, without associated drainage of the subretinal fluid, although an unsuccessful attempt of treatment has been reported( 11 ). In our case, intrasurgical C3F8 was used, and it is of note that treatment with PR was suggested because the tears in retinoschisis were elevated and close to each other. In the first treated eye, the gas was effective in resolving the subretinal fluid and attaching the retina, which indicates that PR is a valid option in cases of retinoschisis with RD. However, late treatment failure was observed, considering that a linear tear was not identified and properly blocked with laser, causing fluid leakage after partial absorption of the gas. Preoperative fundoscopy did not clearly identify the tear responsible for the re-detachment, and for this reason, scleral buckle surgery was rejected; during posterior vitrectomy, a linear tear in the superior quadrant was detected in the inner layer without laser blockage. In contrast, in the LE, after documentation of the RD progression, PR was performed with blockage of retinoschisis using argon laser photocoagulation. The subretinal fluid moved to the temporal region and was slowly absorbed without recurrence after a 12-month follow-up.
This case suggests that PR may be considered a treatment option in selected cases of SR-associated RD. The advantages include a less invasive procedure, possibility of performing the procedure in an outpatient setting, decreased costs, and lower complication rates( 9 , 12 ). The identification of all the tears and rigorous pexia are crucial in the treatment proposed to decrease the risk of failure.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

