INTRODUCTION
Optic disk melanocytoma (ODM) is a relatively common and well-known benign intraocular tumor(1). It can be defined as a melanocytic nevus variant located at the optic disk and histopathologically presents as uniform, deeply pigmented cells with melanosomes and after bleaching, small uniform nuclei with inconspicuous nucleoli and abundant cytoplasm(2).
ODM is usually diagnosed by ophthalmoscopic examination due to the characteristic appearance of the tumor(1,3,4). Ancillary procedures, such as fundus photography, fluorescein angiography (FA), and optical coherence tomography (OCT), can help the diagnosis and are useful for follow-up evaluations(1).
Fundus autofluorescence (FAF) is a non-invasive examination based on the fluorescent appearance of lipofuscin when illuminated by an external light source(5). Lipofuscin is a mixture of proteins, lipids, and small chromophores that accumulate in retinal pigment epithelium (RPE) as a result of incomplete or deficient photoreceptor outer segment degradation(6). Depending on the intensity of the autofluorescence, a lesion may be described as isoautofluorescent, hypoautofluorescent, or hyperautofluorescent(5).
FAF has been used in the assessment of choroidal melanocytic tumors but not yet in melanocytomas(3). The aim of this paper is to describe the clinical features and FAF and OCT findings of two consecutive patients who presented with ODM.
METHODS
A retrospective study was performed by reviewing medical records of two consecutive patients diagnosed with ODM and referred to an ophthalmic oncology specialist at the Hospital Universitário Professor Edgard Santos, Salvador (BA), Brazil within a three-month period (June-September, 2012). Both patients had undergone ancillary procedures at the Retina and Vitreous service of the Hospital São Rafael (Fundação Monte-Tabor), Salvador (BA), Brazil.The study protocol was approved by the Institutional Ethics Review Board of the Hospital São Rafael-Fundação Monte-Tabor and conducted by the Retina and Vitreous Service at the same institution (CAAE: 14929313.4.0000.0048).
Ancillary procedures performed were color and red free retinography, FAF, FA and spectral-domain OCT. A Topcon TRC-50DX retinal camera and Optovue-RTVue 100 were used.
Demographics, clinical data, and ophthalmic imaging examination findings were described and compared with the actual relevant literature. The ophthalmological examination, ancillary procedures, and data collection were performed by the same ophthalmologist.
RESULTS
Case 1
A 48-year-old female, dark-skinned, without comorbidities, was referred to an ophthalmic oncology specialist due to a pigmented intraocular tumor causing progressive vision loss in the right eye (OD). Best corrected visual acuity was counting fingers (CF) in OD and 20/25 in the left eye (OS). Biomicroscopy and tonometry were normal in both eyes (OU). Ophthalmoscopy presented as a black mass covering the optic disk and adjacent retina, including the fovea, with some vitreous seeding in the OD (Figure 1 A). There were no significant findings in the OS.
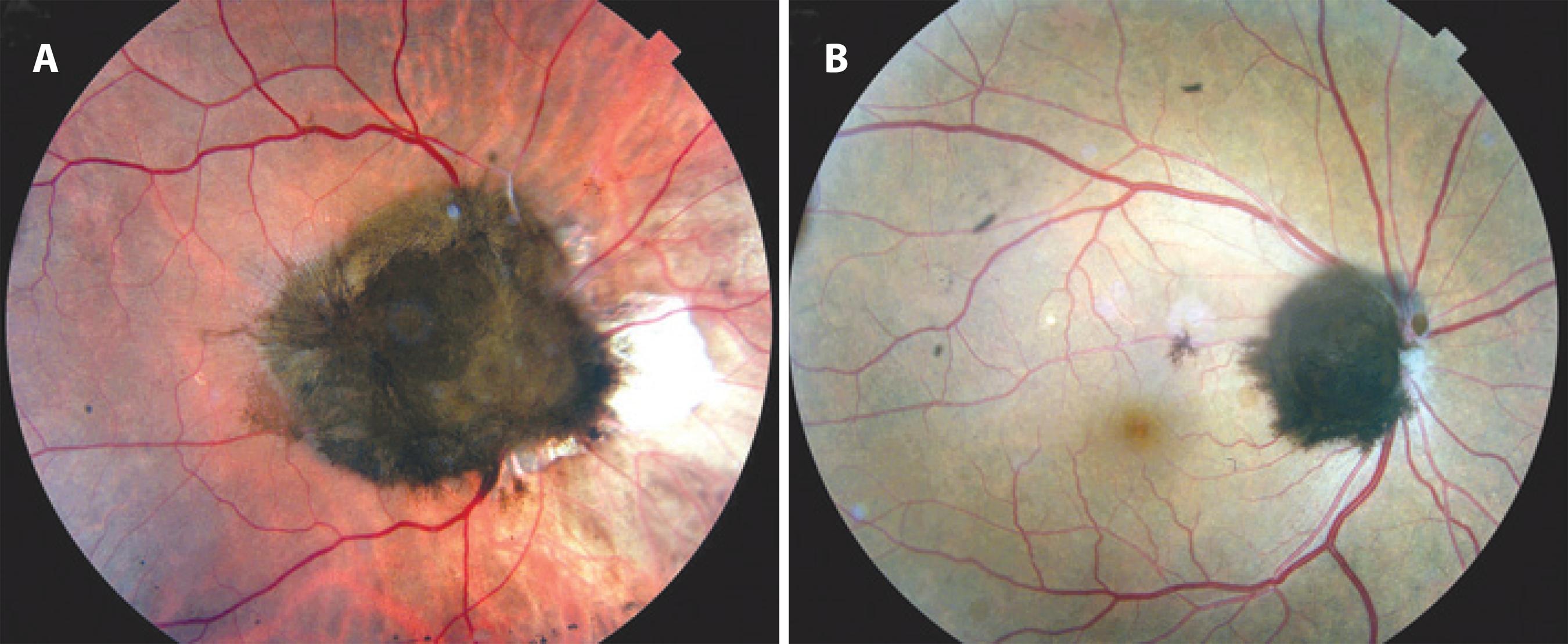
Figure 1 Clinical appearance of optic disk melanocytoma in the described patients. Case 1 (A). Case 2 (B).
FA presented as a hypofluorescent image with regular and well-defined outlines during the whole examination, matching to fluorescence blockage caused by tumor in the OD. There were no significant findings in the OS.
Case 2
A 53-year-old male, dark-skinned, with systemic arterial hypertension was referred to an ophthalmic oncology specialist due to a pigmented intraocular tumor found in a routine examination. Best corrected visual acuity in OU was 20/20, and biomicroscopy and tonometry revealed no changes in OU. Ophthalmoscopy showed a black mass covering the optic disk and some adjacent retina, with massive vitreous seeding, preserving the macula in the OD (Figure 1 B). There were no relevant findings in the OS. FA showed the same pattern as that described in case 1.
Spectral-Domain OCT and FAF
Both cases presented similar OCT and FAF findings. Spectral-domain OCT showed an elevated hi-reflective line corresponding to the tumor surface, followed by a dense shadow pictured as an optically empty mass (Figures 2 A and B). Hi-reflective spots in the vitreous cavity anterior to the tumor and corresponding to vitreous seeding were found in case 2 (Figure 2 C).
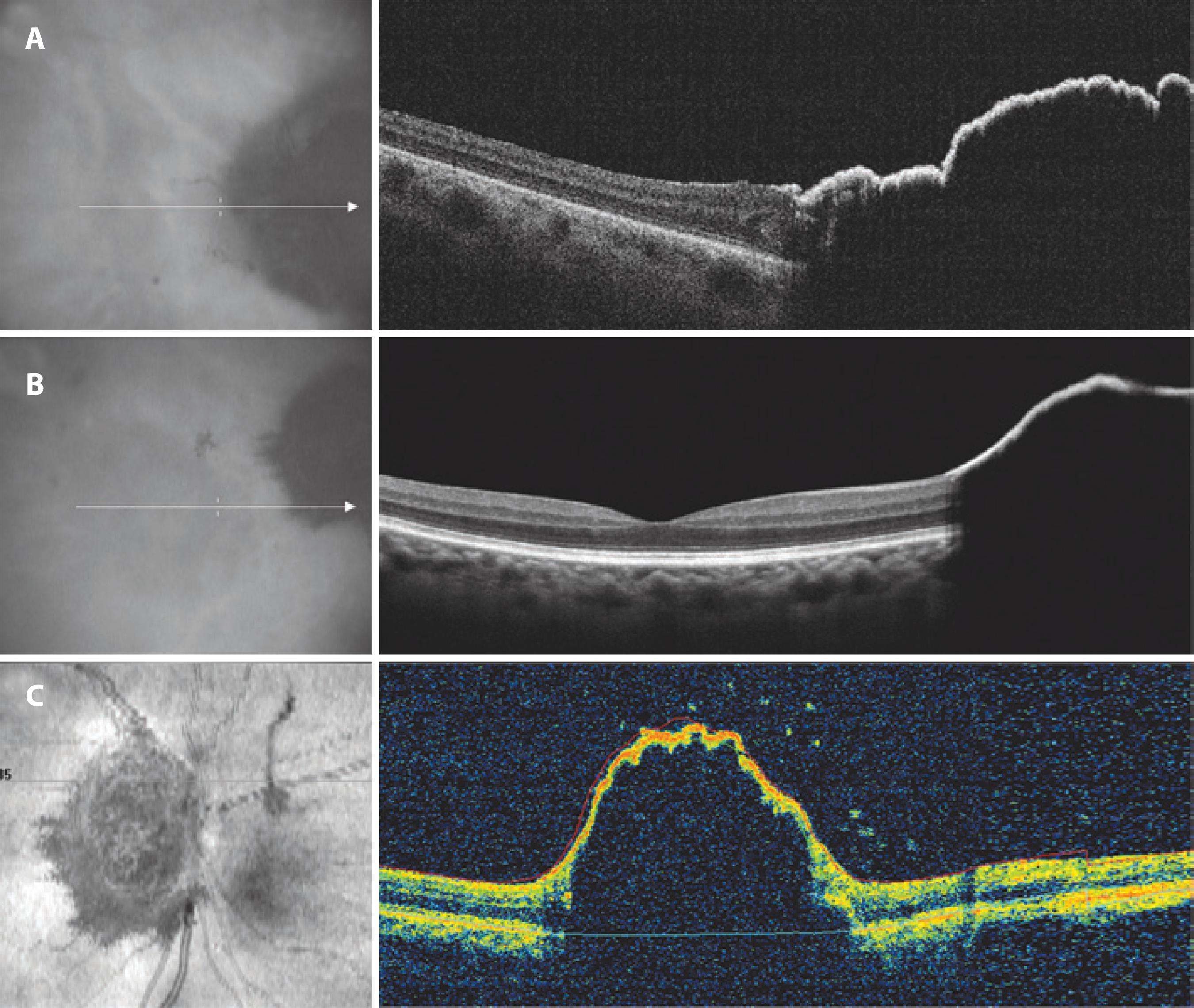
Figure 2 Spectral-domain OCT showing an elevated hi-reflective line corresponding to the tumor surface, followed by a dense shadow pictured as an optically empty mass (A and B). Hi-reflective spots in the vitreos cavity, antherior to the tumor, corresponding to vitreos seeding were found in case 2 (C).
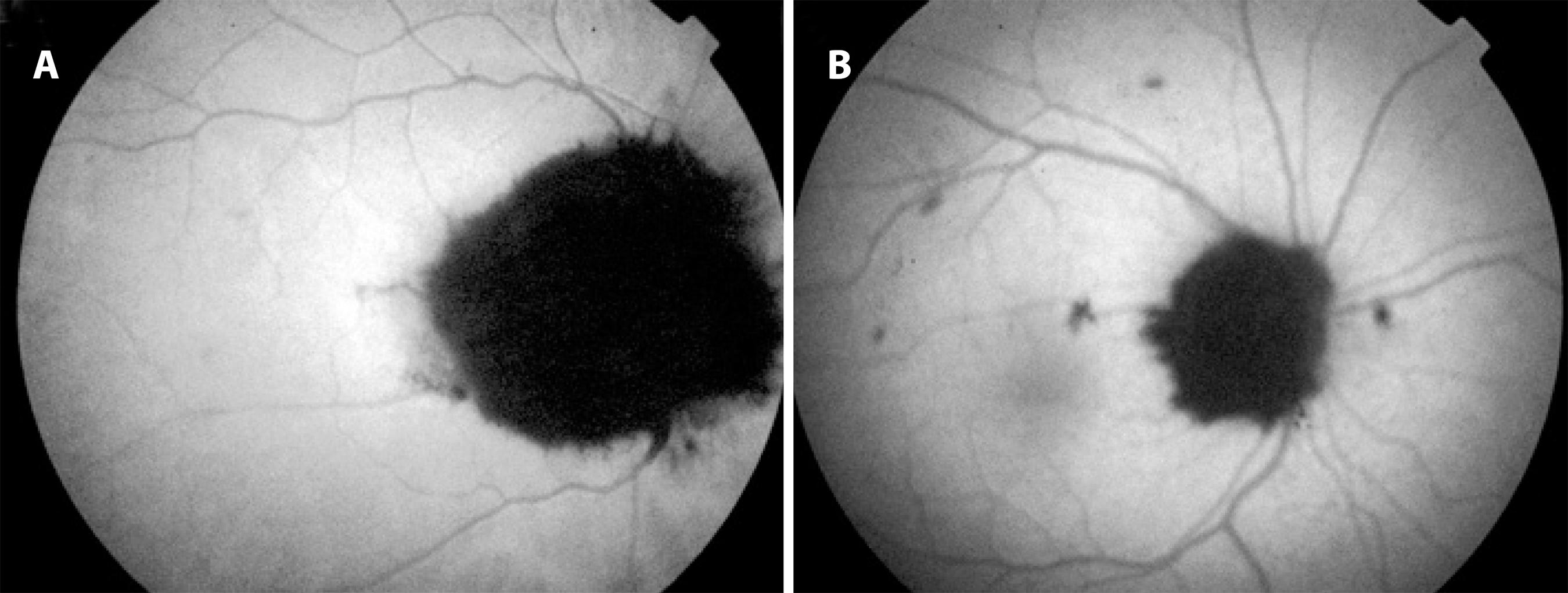
FAF revealed an outstanding hypoautofluorescence. The remaining retina demonstrated isoautofluorescence (Figures 3 A and B).
DISCUSSION
Despite the characteristic clinical appearance of melanocytoma, conditions such as primary or metastatic choroidal melanoma and combined hamartoma of the retina and RPE must first be ruled out(1,3,4). Other differential diagnoses include choroidal nevus, RPE hyperplasia, and RPE adenoma(1,4). Transformation of melanocytoma into malignant melanoma is extremely rare(6).
OCT is a valuable tool for examining the retina and inner choroid architecture(7). OCT patterns and applications are well described in several choroidal and retinal tumors(4,7). OCT findings in ODM include sloped and brightly reflective anterior tumor surface, adjacent retinal disorganization, and abrupt posterior optical shadowing(3). Vitreous seeds can be found(4). Both of the presented cases showed the characteristic features. Vitreous seeds were evident in one patient.
A leading cause of decreased visual acuity in ODM is related to retinal exudation(8). Rarely, excessive tumor growth, involving the fovea, is the cause of vision loss(1). OCT is useful in providing information about the adjacent retinal tissue in ODMs(4). In case 1, OCT was valuable in delimitating the tumor extention and excluding other treatable conditions.
FAF has been previously used in the assessment of choroidal melanocytic tumors but not yet in melanocytomas(3). In both described cases, FAF showed the same pattern: the tumor appears as an outstanding hypoautofluorescent lesion and the remaining retina was isoautofluorescent.
In an OCT-pathologic correlation, Finger et al. showed a very similar OCT image(9). Histopathologically, they found a thin layer of gliotic and disorganized retina covering the tumor surface(9). We suppose that the absence of RPE over the tumor, and therefore lipofuscin, is associated with the highly pigmented mass blocking the posterior RPE, which can explain the outstanding hypoautofluorescence. Further studies are necessary to confirm these assumptions due to the great variability of the ODM presentations despite the small sample in this study.
FAF findings in ODM differential diagnoses, such as choroidal melanoma and choroidal nevus, have been previously described(5,10,11). FAF is useful in documenting the presence of lipofuscin, a finding that represents an important criterion in differentiating small choroidal melanoma from benign choroidal nevus(5). Choroidal melanomas have mild autofluorescent properties (granular appearance in 92% of cases and nongranular appearance in 8%)(5). Lately, a quantification method of digital autofluorescence was suggested for distinguishing nevi from melanomas with a sensitivity of 0.89 and specificity of 0.93(12). The FAF patterns found in the presented cases can be helpful for diagnosing suspicious melanocytic lesions.
The authors were not able to find any descriptions of ODM FAF in the reviewed literature. Therefore, we assume that this is the first report of these findings and believe that when its pattern has been clearly defined, FAF will be a useful tool to avoid misdiagnosis in suspicious cases and for follow-up.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

