INTRODUCTION
The tilted optic disc is a congenital, nonhereditary condition in which the optic nerve enters the eye at an oblique angle. Its prevalence has been reported to be 1%-2% in the general population(1). In clinical practice, the diagnosis of tilted disc is based on ophthalmoscopic appearance. Clinically, tilted discs appear as an exaggerated oval or D-shaped optic nerve head with one hemisphere of the disc more elevated than the contralateral half(2). The elevated margin of the disc is usually adjacent to an intact neurosensory retina, pigment epithelium, and choroid and the depressed portion of the disc is commonly associated with a thinned choroid and thinned retinal pigment epithelium (RPE) that may be visible as fundus depigmentation on ophthalmoscopic evaluation(3-5).
The most common form of optic disc tilt consists of superotemporal rim elevation, often with inferonasal depression(5). Subretinal neovascularization and chorioretinal degenerative changes in the tilted disc syndrome have been reported(6-8).
In most of the cases, RNFL thickness was found to be thinned on the sectors close to the elevated disc rim. Many studies have discussed altered RNFL patterns in cases of tilted disc, but the results did not reflect the same results. Law et al.(9) found significant lower RNFL in eyes with tilted optic disc, whereas Rauscher et al.(10) found no association between optic disc tilt and RNFL. Controversially, the study by Hwang et al.(11) using a Cirrus HD OCT found a significantly thicker RNFL in eyes with tilted disc.
The characteristics of tilted optic disc make the diagnosis and monitoring of glaucoma difficult due to the similarities with glaucomatous discs. Moreover, tilted disc is associated with visual field defects, which also leads to diagnostic difficulties.
With the advent of OCT, all retinal layers can now be measured objectively, and the technique is widely used to assess the status of the RNFL in patients with glaucoma and other optic neuropathies(12). Spaide et al. recently described a technique (enhanced depth imaging) in which SD-OCT was used to measure choroidal thickness(13).
Our aim was to study RNFL and peripapillary choroidal thickness in individuals with tilted disc and compare the values obtained from the control group in order to identify characteristic RNFL and choroidal thickness patterns.
METHODS
This prospective study included 35 eyes of 35 patients with tilted disc syndrome (14 men and 21 women). Records from the Ophthalmology Department at Konya Training and Research Hospital were scanned. Patients who were diagnosed with tilted optic disc were invited to participate in the study from December 2013 to February 2014. The control group included 29 eyes of 29 age- and sex-matched control subjects. All patients underwent a complete ophthalmic examination including slit-lamp biomicroscopy, Goldman applanation tonometry, color vision test (Ishihara test), fundoscopy, optic disc photograph imaging and computerized perimetry. Subjects were evaluated by a 24.2 program with SITA standard algorithm of the Humprey Visual Field analyser II model 750i (Humphrey Instruments, San Leandro, CA, USA). Only the reliable visual field parameters (fixation loss, <20%; false positive rate, <33%; and false negative rate, <33%) were included in the study. Global indices (mean deviation [MD] and pattern standard deviation [PSD]) were evaluated. Tilted disc cases underwent two reliable visual fields, with a minimum time interval of 1 month, and control cases received only one reliable visual field test after the perimetric learning effect.
Best-corrected visual acuity (BCVA) was measured by means of the standard Snellen chart. The values of visual acuity were converted to the logMAR scale for statistical analysis. Exclusion criteria included history of glaucoma and intraocular trauma, optic neuropathy, axial length measurement other than 22-26 mm and a spherical equivalent higher than -6.00 D. Subjects with unstable and uncontrolled cardiovascular, renal or pulmonary diseases, diabetes and pregnancy were also excluded. A tilted disc was defined as anteroposterior rotation (tilt) and sagittal plane rotation (torsion) based on a review of tilted disc syndrome by Witmer et al.(2). These characteristics were easily evaluated by fundoscopy or optic disc photographs.
Choroidal thickness measurements were performed using an SD-OCT device (λ=870 nm, 40000A-scans/s and 3.9 μm axial resolution) with software version 5.3 (Spectralis; Heidelberg Engineering, Heidelberg, Germany). RNFL imaging was performed using circular scans of a diameter of 3.4 mm around the optic disc. The scans were well centered at the optic nerve head. Spectralis OCT included RNFL thickness in six sectors: nasal (N), superonasal (NS), superotemporal (TS), temporal (T), inferotemporal (TI) and inferonasal (NI), as well as global RNFL thickness (G) (Figure 1).
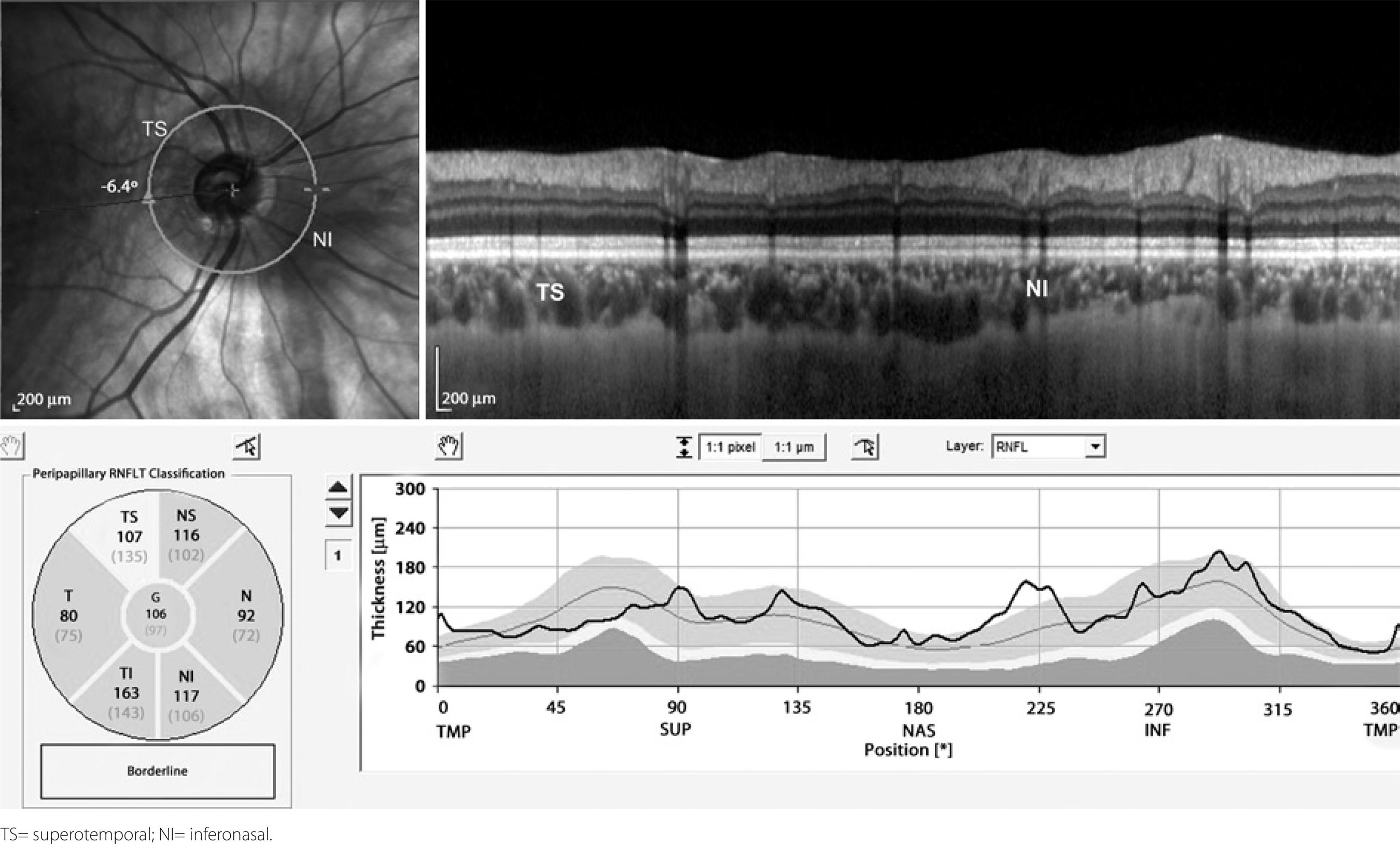
Figure 1 Inferior nasal crescent and superotemporal disc rim elevation with loss of superior retinal nevre fiber layer thickness verified in OCT.
For measurements of peripapillary choroidal thickness, a 360-degree 3.4 mm diameter peripapillary circle scan was performed using the standard protocol for RNFL assessment. Choroidal thickness was measured manually from the outer portion of the hyperreflective line corresponding to the RPE to the inner surface of the sclera (Figure 2). Peripapillary choroidal thicknesses adjacent to the elevated disc rim and the depressed sector directly opposite to the elevated disc rim were evaluated. In the control group, measurements were taken of the superotemporal and inferonasal peripapillary choroidal thickness in which the superotemporal choroid region corresponded to the choroid adjacent to elevated disc rim in the tilted disc group and the inferonasal choroid corresponded to the choroid adjacent to the depressed disc rim, which is directly opposite the elevated disc rim location, in the tilted disc group (Figure 1). The choroid was measured by two independent graders (MO, SI) using the tools found on the Spectralis OCT analysis software. The intraclass correlation coefficients for overall peripapillary choroidal thickness were used to assess agreement between both graders.
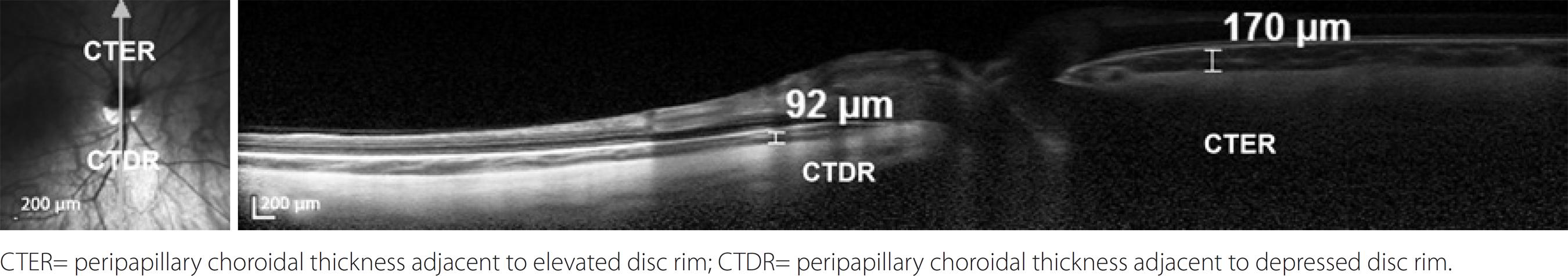
Figure 2 Peripapillary choroidal thickness image showing thinner choroid in the inferior sector of the optic disc.CTER= peripapillary choroidal thickness adjacent to elevated disc rim; CTDR= peripapillary choroidal thickness adjacent to depressed disc rim.
The study was conducted under a protocol approved by the Konya Selcuk University Medical Faculty Ethics Committee and was in accordance with the ethical standards stated in the 1964 Declaration of Helsinki. Informed consent was obtained from all the patients after explanation of the procedures.
All statistical analysis of the data were performed using commercial software (Statistical Package for Social Science, version 15.0; SPSS Inc., Chicago, IL, USA). Statistical analysis was performed by using the Independent t-test (parametric). Pearson correlation coefficient was used to evaluate the correlation between the RNFL thickness and the global indices of visual field. Results were considered statistically significant when p<0.05. Results are represented as mean ± SD.
RESULTS
The recordings of 35 patients were assessed and six were excluded from the study. Four cases were excluded because the sclera was invisible in OCT, and two cases were excluded due to unreliability for visual field analysis. A total of 58 subjects were included in the study. The tilted disc group included 29 eyes of 29 individuals, aged between 19 and 67 years (mean age, 45.3 ± 13.2). The control group included 29 eyes of 29 individuals aged between 21 and 64 years (mean age, 48.3 ± 12.1).
Fundus examination in all eyes showed the existence of tilted optic disc with mainly inferior nasal crescent (Figure 1). The most common form of tilted disc we found was superotemporal rim elevation (n=17, 58.6%), followed by temporal rim elevation (n=7, 24.1%). None of our cases had evident posterior staphylomas on fundoscopic examination.
Mean best-corrected visual acuity was 0.15 ± 0.13 logMAR for the tilted disc group and 0.08 ± 0.06 logMAR for the control group. The axial length value for the tilted disc group was 25.1 ± 2.3 mm and 24.8 ± 3.4 mm for the control group. There were no differences between the tilted disc and control groups in regard to mean BCVA and axial lenght (p=0.09 and p=0.087, respectively). The mean spherical equivalent for the tilted disc group was -1.94 ± 2.56 D, whereas the control group mean was -0.86 ± 1.96 D (p=0.076). All patients had normal color vision.
The RNFL thickness analysis showed that the superotemporal and superonasal sectors were significantly thinner in the tilted disc group than those of the control group (p<0.001 and p=0.001, respectively; Table 1). The RNFL thickness of the nasal sector was significantly higher in the tilted disc group (p=0.013); however, the global RNFL was significantly lower in the tilted disc group (p=0.005).
Table 1 RNFL thickness: tilted disc and control group
| SD-OCT RNFL (μm) | Tilted disc group (n=29) | Control group (n=29) | Significance |
|---|---|---|---|
| Superotemporal | 109.24 ± 9.98 | 126.44 ± 9.45 | p<0.001 |
| Superonasal | 85.37 ± 13.34 | 106.68 ± 9.99 | P=0.001 |
| Inferonasal | 113.72 ± 8.87 | 118.24 ± 12.27 | p=0.114 |
| Inferotemporal | 129.27 ± 15.36 | 133.72 ± 13.25 | p=0.243 |
| Temporal | 67.10 ± 9.67 | 71.58 ± 10.19 | p=0.091 |
| Nasal | 81.44 ± 9.48 | 74.82 ± 10.20 | p=0.013 |
| Global | 87.62 ± 10.37 | 96.06 ± 11.44 | p=0.005 |
Peripapillary choroidal thicknesses are presented in table 2. The analysis showed that the mean choroidal thickness next to the elevated disc rim was 193.75 ± 37.87 µm and the mean choroidal thickness opposite this location was 125.48 ± 24.68 µm; the difference was statistically significant between these topographical regions in the same eye (p<0.001). The control group had a mean superotemporal peripapillary choroidal thickness of 209.37 ± 27.98 µm and an inferonasal choroidal thickness of 198.34 ± 17.08 µm; the difference was not significant between these topographical regions in the same eye (p=0.075). There was no significant difference in superotemporal choroidal thickness between the tilted disc and control groups (p=0.079); however, inferonasal choroidal thickness was significantly lower in the tilted disc group (p<0.001).
Table 2 Average peripapillary choroidal thickness (μm)
| Sectors | Tilted disc group | Control group | p-value |
|---|---|---|---|
| Superotemporal (CTER) | 193.75 ± 37.87 | 209.37 ± 27.98 | p=0.079 |
| Inferonasal (CTDR) | 125.48 ± 24.68 | 198.34 ± 17.08 | p<0.001 |
| p-value | p<0.001 | p=0.075 |
CTER= peripapillary choroidal thickness adjacent to elevated disc rim; CTDR= peripapillary choroidal thickness adjacent to depressed disc rim.
Eighteen eyes (62%) presented visual field defects, most frequently found on the superotemporal quadrant (n=10), whereas 11 eyes had normal visual fields. There was generalized reduction in retinal sensitivity in all quadrants. Visual field analysis revealed a pattern standard deviation (PSD) of 4.20 ± 1.47 for the tilted disc group, which was significantly higher (p<0.001) than the control group (1.65 ± 0.60). Mean deviation (MD) was significantly lower (p<0.001) in the tilted disc group than the control group, with a mean value of -7.09 ± 3.45, whereas the control group had a MD of -2.63 ± 1.29. There was no significant correlation (correlation coefficient, p value) for MD and the RNFL thicknesses at all quadrants except TI (0.373, p=0.046) and for PSD and the RNFL thicknesses at all quadrants except TI (0.458, p=0.013). There was a significant correlation for PSD the global RNFL thickness (0.428, p=0.020).
Regarding the manual measurement of peripapillary choroidal thickness, the intraclass correlation coefficients showed agreement between the two observers (p<0.001) and ranged from moderate (0.67, next to the elevated disc rim) to very high (0.96, superotemporal).
DISCUSSION
This study used SD-OCT to demonstrate that tilted optic disc is associated with abnormal patterns of both peripapillary RNFL and choroidal thickness. The most common form of tilted disc in our study was inferonasal disc rotation with superotemporal rim elevation, which is similar to previous reports(1,5,14). We found that a significant difference exists in the choroidal thickness between the elevated and depressed sectors of the optic disc, in which there is a thinner choroid next to the depressed part of the disc. Furthermore, we found that eyes with inferior tilted disc show superior RNFL defects when analyzed by OCT imaging. We also confirmed that global RNFL was significantly lower in the tilted disc group. These findings show that OCT technology may be more sensitive for the detection of RNFL defects in abnormal optic disc morphologies.
The choroid inferior to the optic disc and the choroid nasal to the macula were reported to be thinner than all other sectors, and those variations were attributed to the natural anatomical architecture of normal eyes(15). This regional difference observed in choroidal thickness may be imputable to the development of the eye. Evidence from embryology indicates that the optic fissure is located in the inferior aspect of the optic cup, which is the last part of the globe to close during eye formation. A thinner choroid may be important because it may make this area more susceptible to retinal and choroidal diseases(15). This idea is favored by eyes with glaucoma wherein the choroid was reported to be thinner and the observation of more severe field defects in the thinner hemifield in glaucomatous eyes(16). Reported disorders such as subretinal neovascularization and chorioretinal degenerative changes in the tilted disc syndrome(3) may be associated with thinner choroid next to the depressed part of the optic disc. It is unclear why the choroid is thinner in the discoloration area than in the other quadrants. However, it may correspond to the absence of retinal pigment epithelium and photoreceptors and attenuation of the choroid(17).
Brito et al.(14) reported that the most common RNFL defect was located on the superotemporal sector of the Spectralis OCT, and the most commonly involved perimetric quadrant was also superotemporal. They speculated that this was the opposite of what would be expected. We likewise found superotemporal visual field defects in cases with superotemporal RNFL defect; however, the results of analysis of correlations between MD and PSD were not completely consistent. We therefore concluded that visual field defects in individuals with tilted optic disc might be multifactorial in origin. Furthermore, it would be beneficial to study visual fields and document the factors influencing the test parameters in subjects with tilted optic disc.
In this study, OCT examination found that RNFL thickness was significantly thinned in the superior quadrant in patients with tilted disc syndrome. This may be attributed to the fact that the density of nerve fibers entering the optic disc in tilted disc syndrome is lower in this sector(18).
The differences may be due to hypoplasia associated with tilted disc. There is little knowledge regarding the underlying etiology of the embryonic aberrations(19). Simon et al.(20) reported that intrauterine injury to the retina, optic nerve, chiasm or posterior visual pathway may cause hypoplasia of the optic nerve. Similarly Apple et al.(5) speculated that localized absence of ganglion cells and their failure to make synaptic connections in the lateral geniculate body might result in hypoplastic development of other supportive tissue. Consequently, the disc becomes tilted because of the imbalance in the number of ganglion cells and supportive tissue within the optic nerve. In addition, when the visual fields of eyes with tilted optic disc were compared to control groups, there was generalized reduction in retinal sensitivity in all quadrants(21). This generalized reduction in sensitivity has lead to the opinion that tilted disc may represent a diffusely hypoplastic optic nerve(22).
It is an uneasy issue whether a patient with tilted disc and ocular hypertension has glaucomatous optic neuropathy and RNFL damage. A commonly observed problem with tilted disc is the detection of early glaucomatous damage. Both are associated with visual field defects, and tilted disc morphology is a finding in optic disc rim evaluation; its presence makes identification of the usual signs of glaucomatous damage, such as pathological cupping, difficult to detect(23,24). We may say that the presence of a small visual field defect in a patient with an inferior tilted disc and superior RNFL loss is most probably related to tilted disc morphology instead of glaucomatous optic neuropathy; however, this argument needs to be proven by large-scale studies comparing visual fields in both glaucoma and tilted disc groups. In addition to clinical examination, realization of OCT in conjunction with perimetry can help in the diagnosis and monitoring of glaucoma in cases of concomitant optic disc tilt. OCT appears to have the ability to distinguish normal from glaucomatous optic nerve heads, but it is not clear that these findings can be generalized to tilted disc and glaucoma(25). Witmer et al.(2) partly supported this notion as they reported that new technologies for imaging the optic nerve head and RNFL currently had a limited role in diagnosing and monitoring tilted disc. There could be OCT error due to the abnormal anatomy of the nerve, as tilted discs can mimic other conditions; however, this diagnostic error is best prevented by clinicians who are familiar with the clinical manifestations of the anomaly. Nevertheless, in a study of patients with glaucoma and tilted discs, OCT was shown to be accurate in measuring the RNFL thickness and corresponded well to Humphrey visual field defects(26).
Eyes with tilted discs were more miopic than controls. However, none of our cases had evident posterior staphylomas on fundoscopic examination. Furthermore, we recruited cases with a spherical equivalent lower than 6.00 D of myopia to reduce the possible effects of myopic chorioretinopathy on peripapillary RNFL. To avoid RNFL changes due to mechanical tissue stretching, we included cases with an axial length measurement within a certain range (22-26 mm).
OCT imaging of the optic nerve head and RNFL rely on validated normative data; however, validated normative datasets for tilted disc do not currently exist. Therefore, considering these data, imaging the optic disc with OCT could be a limitation of our study.
This study demonstrated a clinical characterization of the main tilted disc morphologies that may be helpful in differentiating a tilted disc from other altered disc morphologies. Additionally, the presence of optic disc tilt should be taken into account when interpreting peripapillary RNFL and choroidal thicknesses by SD-OCT. It would be beneficial to explore the comparison between glaucoma and tilted disc groups in additional studies.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

