INTRODUCTION
Syphilis is a sexually transmitted disease. Ocular infection can manifest in secondary or tertiary syphilis, and is considered the great "mimicker" of infectious and noninfectious forms of uveitis(1). Uveitis is the most common ocular manifestation, occurring in 2.5% to 5.0% of cases of secondary or tertiary syphilis. The most common clinical form is acute bilateral multifocal chorioretinitis, with whitish-yellow subretinal plaque. In addition, it can present with panuveitis and vitreitis(2). In the posterior segment, several signs were described in both HIV infected and noninfected patients, including vitreitis, focal retinitis, papillitis, serous retinal detachment, and neuroretinitis, among others. In HIV-infected patients, yellowish-white placoid lesions can be observed in the macula or juxtapapilar, and these are usually flat and with an atrophic center. A dense vitreitis can be the only sign of syphilitic uveitis in HIV-infected patients(3).
The treatment of choice is IV crystalline penicillin(4). Allergic patients can be treated with doxycycline or erythromycin; however, nonpenicillin treatment generally is less effective(5). Although, desensitization is also a choice, it would usually take very long to take effect, given the need for urgent therapy in potentially sight-threatening syphilitic uveitis.
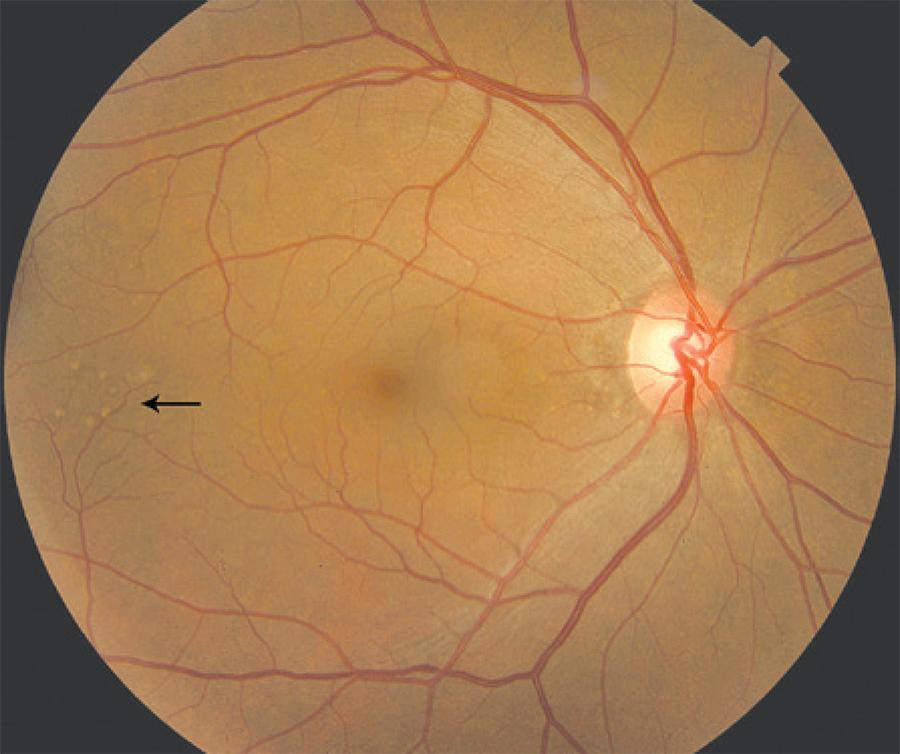
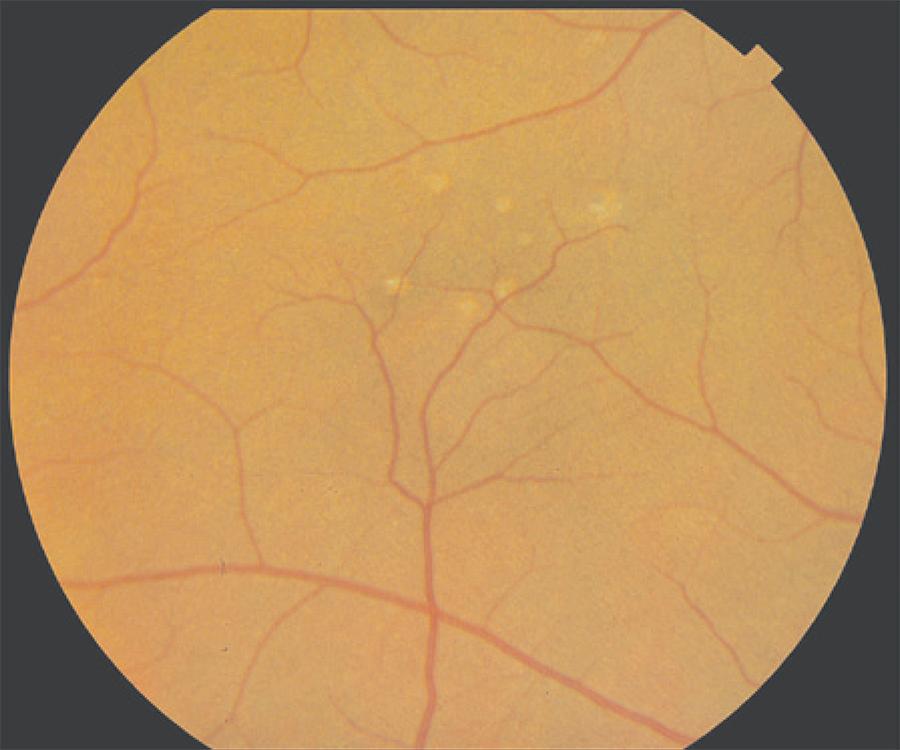
In this case series, we present preretinal pale yellowish dots (Figures 1 and 2) as a manifestation of syphilitic uveitis, and we consider this finding a typical and specific manifestation of ocular syphilis.
CASE REPORT
This case series was performed between March and October 2012 at the Uveitis Sector of Universidade Federal de São Paulo (UNIFESP) on 12 patients who presented with pale yellowish preretinal dots.
Confirmation of ocular syphilis was based on clinical manifestations, and all patients were submitted to both Venereal Disease Research Laboratory (VDRL) and FTA-Abs for syphilis. In addition, lumbar puncture was performed. After diagnostic confirmation of syphilis, fundus photographs and optical coherence of tomography (OCT) (Figure 3) were performed to identify the localization of dots. All cases were treated with IV crystalline penicillin (20 million units/day) for 14 days, which was very effective in controlling the disease.
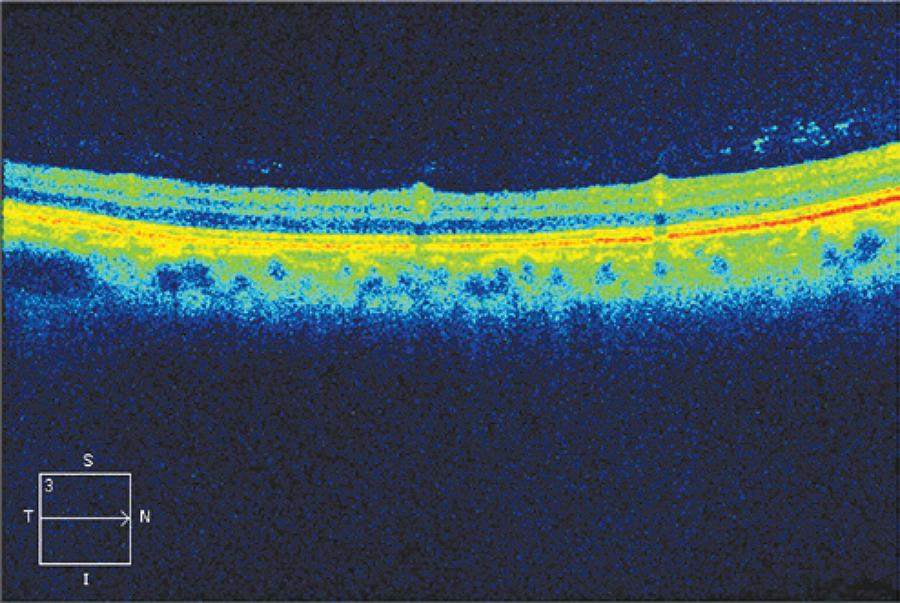
Figure 3 Optical coherence tomography (OCT) of the region, showing perivascular inflammation, with local vitreitis.
Pale yellowish dots were mainly overlying vasculature and also in periphery. OCT was performed and indicated location in the vi-treous-retina transition.
In our 12 cases, 19 eyes were affected, 11 patients were men (91.6%), the median presentation age was 38.1 years, and panuveitis was the main clinical manifestation. Four patients presented bilateral panuveitis (33.3%), three presented unilateral panuveitis (25.0%), two presented bilateral posterior uveitis (16.7%), one presented unilateral retinitis (8.3%), one presented bilateral optic neuritis (8.3%), and one presented anterior uveitis (8.3%). Ten patients were taking oral prednisone (83.3%). Serum VDRL was positive in eight patients (66.7%), cerebrospinal fluid (CSF) VDRL was negative in seven of nine collected (77.8%), serum FTA-Abs was positive in 100% of patients, and eight patients (66.7%) had HIV infection. The best corrected visual acuity (BCVA) after treatment improved in 10 eyes (55.6%), did not change in seven (38.9%), and worsened in one (5.6%). Table 1 shows demographic, clinical, and laboratory findings of all patients.
Table 1 Demographic, clinical, and laboratory data of the patients
| Patient | Sex | Age | Uveitis | Oral prednisone | Liquor VDRL | Serum VDRL | Serum FTA-Abs | Inicial BCVA | Final BCVA | HIV |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 30 | Bilateral panuveitis | Yes | Positive | + | + | HM | HM | Yes |
| 20/60 | 20/40 | |||||||||
| 2 | M | 43 | Unilateral retinitis | Yes | Not collected | + | + | 20/40 | 20/20 | Yes |
| 3 | M | 49 | Bilateral panuveitis | Yes | Negative | + | + | LP | HM | Yes |
| HM | 20/l50 | |||||||||
| 4 | M | 4 | Bilateral panuveitis | Yes | Negative | - | + | CF1 m | 20/60 | No |
| 20/60 | 20/25 | |||||||||
| 5 | M | 40 | Unilateral panuveitis | Yes | Negative | + | + | CF1 m | CF1 m | Yes |
| 6 | M | 37 | Unilateral panuveitis | No | Negative | + | + | HM | CF 50 cm | Yes |
| 7 | M | 32 | Bilateral panuveitis | Yes | Not collected | - | + | CF 2 m | LP | No |
| 20/l00 | 20/20 | |||||||||
| 8 | M | 36 | Unilateral panuveitis | Yes | Negative | - | + | CF 2 m | 20/25 | Yes |
| 9 | M | 28 | Anterior uveitis | Yes | Not collected | + | + | 20/25 | 20/25 | Yes |
| 10 | M | 28 | Bilateral optic neuritis | Yes | Positive | + | + | 20/20 | 20/20 | Yes |
| 20/40 | 20/20 | |||||||||
| 11 | F | 55 | Bilateral | No | Negative | + | + | 20/20 | 20/20 | No |
| Posterior uveitis | ||||||||||
| 12 | M | 40 | Bilateral | Yes | Negative | - | + | CF 1 m | CF 1 m | No |
| Posterior uveitis | 20/60 | 20/60 |
DISCUSSION
Ocular syphilis is a common manifestation of secondary or tertiary syphilis and constitutes an important factor in diagnosis and treatment of different stages of syphilitic infection. Although very common in clinical practice, syphilis infection is under reported in Brazil. According to the Brazilian notification system (DATASUS), prevalence of syphilis during pregnancy was 1.6% in 2004, with an estimate of 48,425 cases. From 2005 to 2012, 57,700 cases of syphilis during pregnancy were notified, with an incidence rate of 0.6 in 1,000 births in 2005, reaching 5 in 1,000 births in 2012. Most were detected in women between 20 and 29 years, and of those diagnosed in 2011, only 11.5% had their partners treated. These data show increases in both notification and incidence of the disease in the past few years in Brazil(6).
Fu et al.(7) described a series of nine eyes from eight patients with syphilitic retinitis, who presented creamy yellowish superficial, multifocal, retinal precipitates, overlying an area of retinitis. Most eyes (66.7%) presented a single group of precipitates, while others (33.7%) presented a multiple group of precipitates associated with distinct areas of retinitis. All manifestations resolved between 2 and 3 weeks after initiation of the treatment(7).
Yang et al.(8) described a Chinese patient who presented mutton fat precipitates in the posterior vitreous membrane with retinal vasculitis in both eyes. In addition, Yang and colleagues described three other eyes in two patients, which presented multiple perimacular whitish dots termed as "multiple punctiform retinian precipitates",(8)very similar to those found in our cases. Our study, as suggested by these authors, indicates that these precipitates or pale yellowish dots are highly suggestive of ocular syphilis. Yang et al.(8) presumed that they were provenient from treponema collections and inflammatory cells, both pre- and intraretinal.
Reddy described a HIV patient with "multiple preretinal aggregates" resting on a sectorial area of detached retina that had a diffuse yellowish-white ground glass full-thickness opacification(9). Furthermore, clinical and OCT presentation were similar to our findings and resolved after initiating treatment for syphilitic retinitis.
Fundus photographs showed that these dots were overlying vasculature and also located at the periphery. OCT revealed that they were located in the vitreous-retina transition (Figure 3), probably due to local perivasculitis, which is typical in treponema infection, as the local vitreitis also suggests. After treatment, ocular findings disappeared in all patients but one, a 55-year-old, female without HIV infection; even with resolution of ocular symptoms, the findings remained present 4 months after treatment with crystalline penicillin.
Although not yet acknowledged in the literature as a typical sign, these are very common findings in ocular syphilis. Other authors suggest that they can be granulomas, but more studies, particularly pathologic studies, are required. It is important to acknowledge these findings because syphilis can present in several forms. In conclusion, ophthalmologists should always consider syphilis in the differential diagnosis of uveitis, particularly in the presence of preretinal dots, which appear to be very suggestive of ocular syphilis.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

