INTRODUCTION
Macular telangiectasia (MacTel), also known as idiopathic juxtafoveolar telangiectasia, is a rare ocular disease that can lead to legal blindness. This disease is characterized by abnormal retinal vascular dilatation and vessel dysfunction.
The term idiopathic parafoveal telangiectasia (IPT) was introduced by Gass and Oyakawa in 1982(1). Based on clinical findings, high-speed indocyanine green angiography, optical coherence tomography (OCT), and demographics, Yanuzzi et al. proposed a classification into type I - telangiectasia Coats aneurismal type, and type II - perifoveais telangiectasias(2). The type 2 is the most common form, occurring in the fifth or sixth decade of life in both sexes, usually bilateral, with progressively detereorating visual acuity(3).
The epiretinal membrane (ERM) arises from defects in the internal limiting membrane that allows the migration of the retinal glial cells and subsequent proliferation and contraction on the inner retinal surface(4). To date, the association between idiopathic macular telangiectasia and ERM formation has not been reported. This case report aims to describe the case of a patient with ERM secondary to macular telangiectasia.
CASE REPORT
The patient was a 46-year-old female with complaints of blurred and distorted vision in both eyes. She had been reporting these symptoms for 2 years. She had no history of any laser treatment, topical medication, or intraocular surgery. She had a history of hypertension and non-insulin dependent diabetes mellitus of 4 months duration, both of which were controlled medically. She had no history of diabetic or hypertensive retinopathy.
On examination, her vision with correction was 20/200 for the right eye, counting fingers 5 meters left eye, with normal intraocular pressure, normal results of papillary examination, and a slit-lamp biomicroscopy results that revealed significant initial bilateral nuclear cataracts. Ocular motility was normal in both eyes.
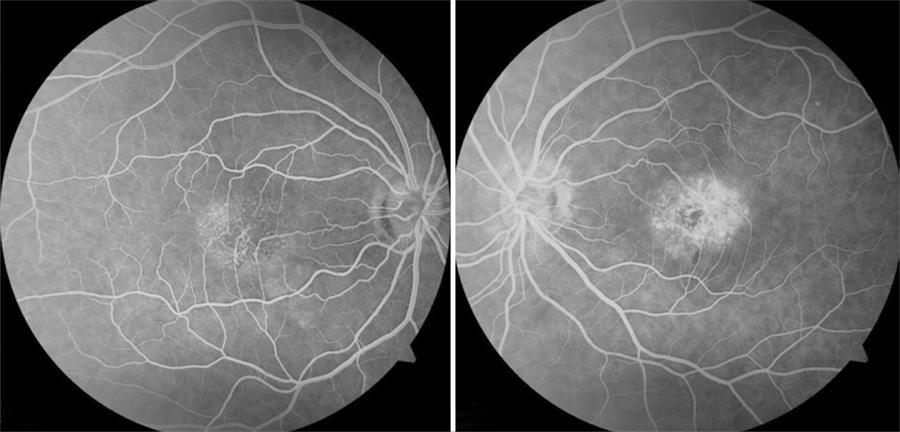
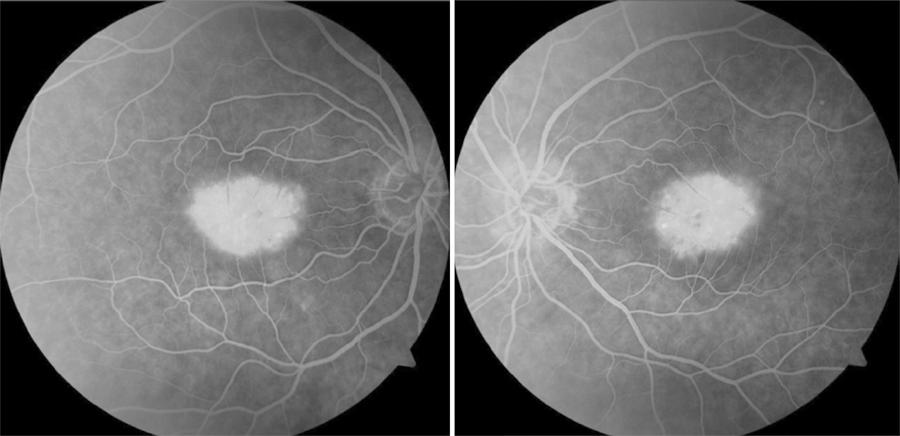
Fundoscopy revealed a clear vitreous, attached retina, optical disc stained, and hard drusen in the posterior pole. Perimacular hemorrhages and aneurismal dilatation of the vessels were evident (Figure 1). A white and elevated lesion, with wrinkling of the retina was found adjacent to vascular changes (Figure 1). Optical coherence tomography (OCT) revealed loss of foveal depression and hyper-reflective areas in the inner layers of the retina, suggesting ERM formation (Figure 2). A cavity between the outer layers of neurosensorial retina, atrophy of the photoreceptor layer, and integrity of retinal pigment epithelium (RPE) were also noted. Fluorescein angiography (FA) revealed a localized area of hyperfluorescence with telangiectasia of capillaries located inferotemporally to the fovea (Figure 3). These features were evident during the late stages of FA due to active leakage of dilated juxtafoveal capillaries (Figure 4). The patient maintains regular annual follow-up.
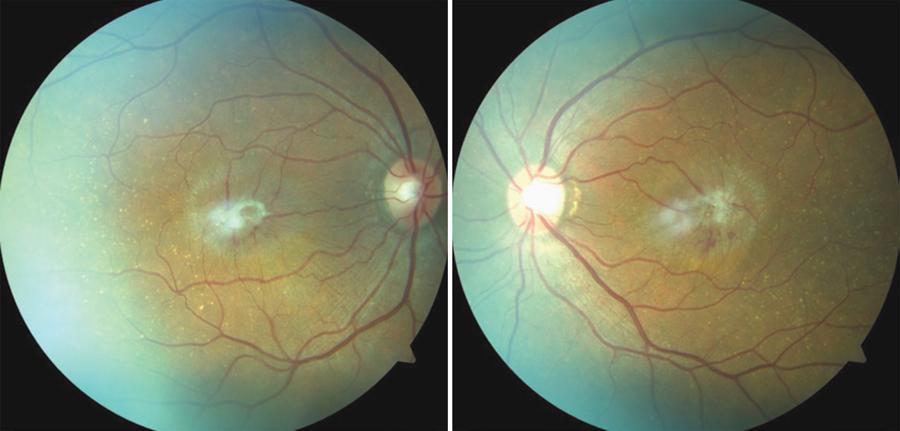
Figure 1 The fundoscopy revealing hard drusen in the posterior pole, aneurismal dilatation of parafoveal vessels and epiretinal membrane.
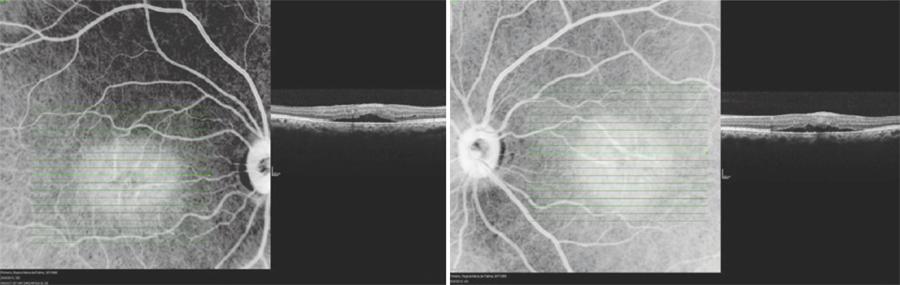
Figure 2 OCT revealing loss of foveal depression, cavity between outer layers of neurosensorial retina and hiperreflective areas suggesting epiretinal membrane.
DISCUSSION
ERM, whose incidence increases with age, occurs in approximately 6% of the patients over the age of 60(5). ERMs can be idiopathic or secondary to an initiating event. It is thought that most idiopathic ERMs originate from fibroglial proliferation on the inner surface of the retina secondary to a break in the inner limiting membrane (ILM) that occur during posterior vitreous detachment. Secondary ERMs result from an already existing ocular pathology such as central or branch retinal vein occlusion, diabetic retinopathy, uveitis, and retinal breaks with or without detachment. Glial cells, RPE cells, and myofibroblasts are shown to be involved in ERM formation.
Yannuzzi et al., classified macular telangiectasias (MacTel) into two types. Type 1 is the aneurismal telangiectasia. This involves predominantly unilateral telangiectasia, mostly in men, with aneurysms of various sizes. Type 2 is the perifoveal telangiectasia. This involves bilateral telangiectasia, which is limited to the perifoveolar area, without visible aneurysms and is associated with subretinal neovascularization (SRN). Nonproliferative perifoveal telangiectasia refers to exudative telangiectasia and foveal atrophy. Proliferative perifoveal telangiectasia refers to proliferative changes with SRN and fibrosis(6).
The cause of MacTel type 2 is not known and no treatment exists to prevent the progressive loss of central vision that often occurs in patients with this disease. MacTel type 2 is also characterized by a loss of macular transparency, superficial white crystals, depletion of macular pigment, and progressive foveal thinning(7). In MacTel type 2, the primary defect is located in the Müller cells or neural cells. The Müller cells regulate capillary endothelial function and metabolism of adjacent cells. Degeneration of Müller cells could cause rupture of the blood-retina barrier in parafoveal capillaries, causing edema.
It has been reported that depletion of the macular pigment (most pronounced alterations occur in the temporal perifoveolar region) is a specific and early clinical feature of MacTel type 2(7). This depletion is associated with a reduction in the number of Muller cells(8).
Muller cell degeneration may explain the ILM drape, cavities within the inner neural retina that commonly are found in MacTel type 2(9), as well as the loss of macular pigment. We hypothesized that dysfunction of Muller cells might lead to ERM formation. It is also possible that MacTel alters the relationship between the hyaloid face and the ILM, thus collaborating in patoghenesis of ERM. It was postulated that chronic exudation caused a change in the vitreous configuration, with secondary vitreomacular traction and ERM formation(10).
In summary, the present case demonstrates that MacTel and ERM may occur concomitantly.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

