INTRODUCTION
Ocular biometry, the refractive status of developing human eyes and how they change with age, is essential for understanding the ocular growth and development of other ocular pathologies.
Many published studies have examined ocular biometry in older populations and have provided significant data. However, there are few population-based age norms for ocular biometry in children due to the technical difficulties in measuring biometric parameters, particularly in small children(1). When we searched for pediatric ocular biometric studies in the ophthalmology literature, we noted some restrictions in the design of previous studies, particularly those with school-age children. There was a paucity of data regarding biometry and central corneal thickness in preschool children. We decided to search for both preschool and school age children to investigate the normal distribution of axial length and central corneal thickness among children in different age groups.
Ocular biometric status varies in different ethnicities. Therefore, data from different areas and ethnicities should be studied. In this article, we present data for ocular biometry and central corneal thickness in a pediatric population. This data contributes to the literature by studying the Caucasian population in the eastern region of Turkey.
METHODS
This study was carried out in Yuzuncu Yil University, Faculty of Medicine, Ophthalmology Department. It was approved by the Human Ethics Committee at Yuzuncu Yil University. The research adhered to the tenets of the Declaration of Helsinki.
The study was performed prospectively. Subjects were children between the ages of 1 and 12 years. The subjects were divided according to age into six groups: 1-2 years, 3-4 years, 5-6 years, 7-8 years, 9-10 years, and 11-12 years. The exclusion criteria were an ocular trauma, ocular surgery, uveitis, glaucoma, cataract, corneal pathologies, vitreous pathologies, retinal pathologies, or premature retinopathy. We did not include children younger than 12 months.
We measured axial length (AL), anterior chamber depth (ACD), lens thickness (LT), vitreous chamber depth (VCD), and central corneal thickness (CCT). AL and CCT measurements were performed with the US-1800 Echoscan (Nidek, Japan) using of A-scan biometry and pachymetry probes via the contact method. The measurements were taken after instilling anesthetic drops (proparacaine) on the cornea. On average, 5 measurements were taken with the pachymetry probe and 10 measurements were taken with the biometry probe to obtain better results. All measurements were taken between 08:30 and 11:30 a.m.
In this study, 364 eyes in 182 individuals were examined. Bilateral evaluation was performed for all patients. The measurements were taken under general anesthesia for 67 patients who had an intervention (probing) for naso-lacrimal dacryostenosis. The measurements were taken during the pre-intervention period in patients who had probing. All measurements were taken by the same ophthalmologist.
Statistical analyses were completed with independently paired t-tests, ANOVAs, and correlation tests.
RESULTS
The mean age was 6.54 ± 3.42 years. For girls, the mean age was 6.61 ± 3.50 years in girls and 6.41 ± 3.30 years in boys. There was no significant age difference between boys and girls. Among all subjects, 63% were boys and 37% were girls; the ratio was 1.70 (n: boys/girls: 115/67).
The mean CCT was 556 ± 34 µm. There was a significant difference between the age groups in terms of CCT. The mean AL, ACD, LT, and VCD were 22.02 ± 1.19, 3.22 ± 0.36, 3.58 ± 0.23, and 15.17 ± 1.11 mm, respectively. Details for the age groups are given in table 1. Significant differences in the age groups were observed in the AL, ACD, LT, and VCD results.
Table 1 Results by age group
| 1-2 years | 3-4 years | 5-6 years | 7-8 years | 9-10 years | 11-12 years | |
|---|---|---|---|---|---|---|
| n | 30 | 29 | 30 | 33 | 32 | 28 |
| CCT | 556 | 547 | 565 | 563 | 550 | 555 |
| AL | 20.49 | 21.81 | 21.97 | 22.25 | 22.66 | 22.95 |
| ACD | 3.06 | 3.20 | 3.02 | 3.30 | 3.31 | 3.44 |
| LT | 3.67 | 3.63 | 3.59 | 3.56 | 3.54 | 3.51 |
| VCD | 13.75 | 14.94 | 15.30 | 15.34 | 15.76 | 15.99 |
n= number; CCT= central corneal thickness (μm); AL= axial length (mm); ACD= anterior chamber depth (mm); LT= lens thickness (mm); VCD= vitreous chamber depth (mm).
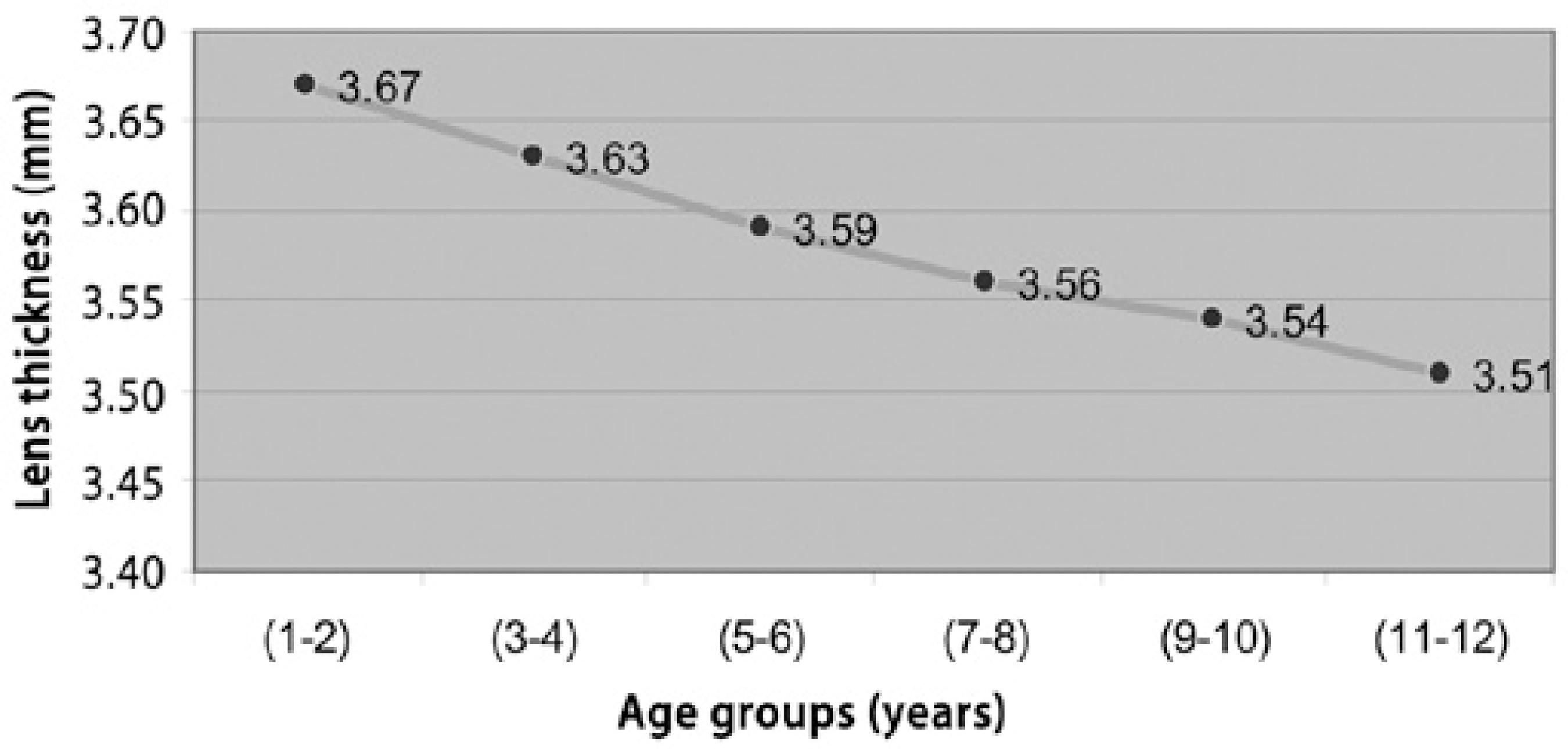
Increasing age was significantly correlated with increasing AL, ACD, and VCD (p=0.000, p=0.000, p=0.000, respectively). Although there was a significant positive correlation between AL, ACD, and VCD, there was also a significant negative association between all of the above measurements and the LT (p=0.054, p=0.000, p=0.000, respectively). An important finding was that LT decreased as the age increased (p=0.000).
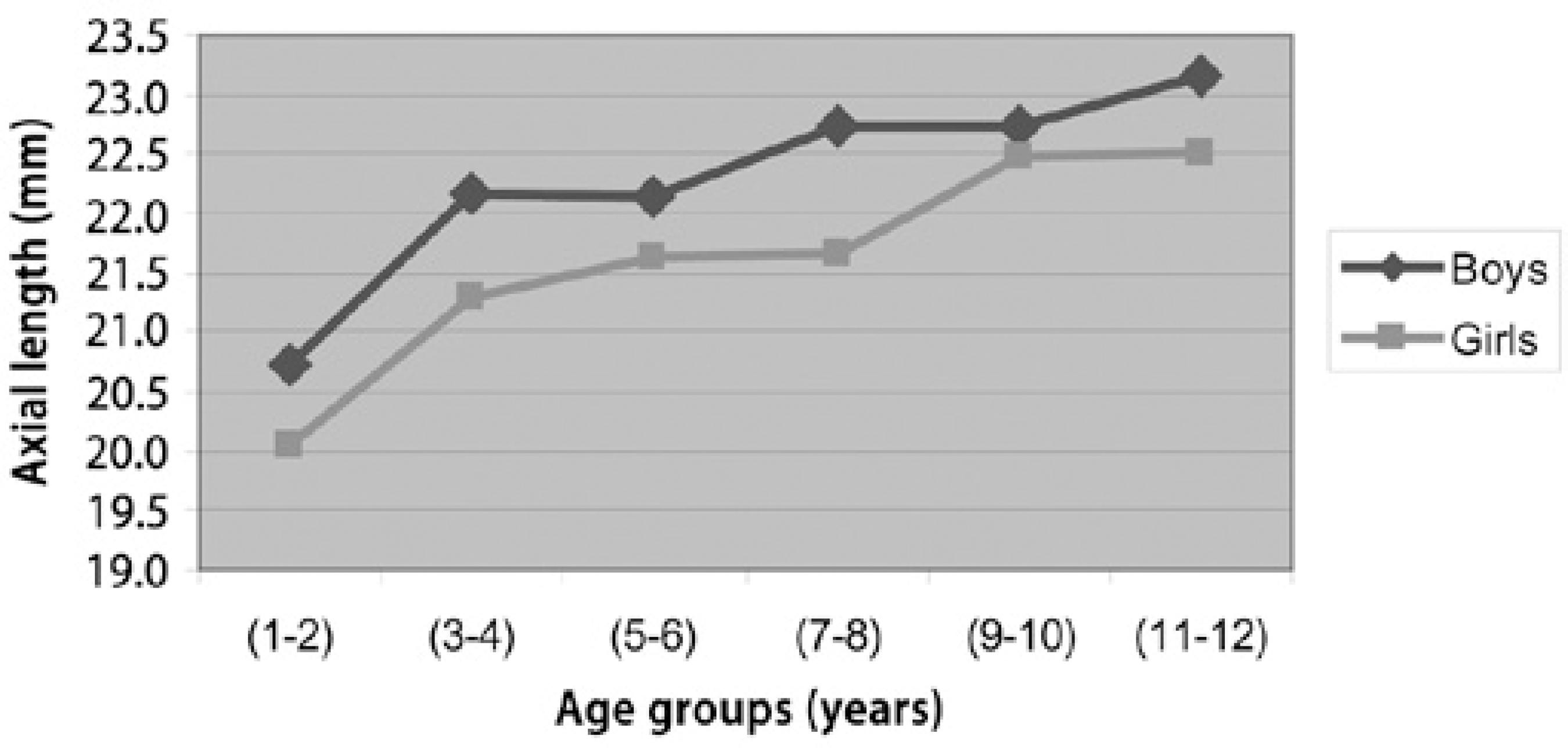
When we compared girls and the boys, there were significant differences in AL, ACD, and VCD (p=0.000, p=0.001, p=0.000, respectively), but there was no correlation in terms of CCT and LT (p=0.128, p=0.147, respectively). The AL was 0.74 mm longer in boys than in girls (Graphic 1).
DISCUSSION
The most striking aspect of our study was that it was not performed with postmortem subjects or with congenital cataract patients, as could be observed in some studies(2,3).
Ocular biometry
Most of the studies with A-scans were conducted with adolescent and adult subjects. In this study, children were studied and the distributions of ocular biometry and CCT were documented in a hospital-based sample of children between 1 and 12 years of age. When we reviewed the literature on ocular biometry with focusing on children, most data was from older children between 5 and 16 years of age(4-7).
In the literature, AL in newborns ranged from 17 to 17.3 mm, and rapid increase was found in the postnatal period. The AL reached 20.6 mm after the first year of life. This rapid increase continued until the third year of life. After this rapid phase, increases in AL slowed until the seventh year and reached adult size at 10 years old(8-10). Our study found similar results showing that AL reached 20.49 mm after the first year of life and reached adult levels between 9 and 10 years of age.
Gordon et al. performed a study with age groups that reported eye growth increased approximately 1 mm/year during the first 2 years of life, 0.4 mm/year between 2 and 5 years, and 0.1 mm/year between 5 and 15 years(9). In our study, similar findings showed that eye growth increased about 1 mm/year in the first 2 years of life and increased 0.3 to 0.4 mm/year after 2 years. The average annual growth rate in our study was 0.26 mm, and we did not observe a linear increase in AL.
Our study also examined whether there were differences between girls and boys. Girls tended to have shorter eyes compared to boys. The males are typically have a deeper anterior chamber and a larger vitreous chamber. In the present study, the AL was 0.74 mm longer in boys than in girls. This finding is consistent with Zadnik et al., who reported that AL was longer in boys(10). Twelker et al. and Ojaimi et al. studied AL in school-age children and reported the same findings(11,12).
In our study, lens thickness was 3.67 mm in the first 2 years of life and 3.51 mm in 11-12 years (Graphic 2). Zadnik et al. studied 869 children between 6 and 14 years of age and reported that there was a decrease in lens thickness between 6 and 10 years(13). Saw et al. studied myopic children who were between 7 and 9 years of age and reported a decrease of about 0.01 mm in lens thickness over 3 years(14). The same finding was also present in Shih et al.'s study, which showed that a decrease was present in children between the ages of 7 and 11 years(15). Our study found that lens thickness continuously decreased until 12 years of age. Therefore, we can say that there was a decrease in lens thickness during the first 12 years of life.
Central corneal thickness
The literature included different results about CCT in children, ranging from 529 to 564 µm(16-21). The average CCT in our study was 556 µm, and the range was between 448 and 678 µm.
Portellinha et al. reported that CCT is 573 µm in the newborn and decreases after birth(22). However, they did not find differences between boys and girls. In our study, there was only a 6-µm difference between boys and girls, which was not statistically significant.
Prost et al. studied 360 children between 0 and 14 years old(23). In newborns, the average CCT was 537 µm, and at 14 years of age, the average was 567 µm. Parentin et al. hypothesized that this decrease took place during the first and second years of life. They claimed that rearrangements in collagen bundles and remodeling occurred in the early years of life(24).
Hussein et al. studied children between the ages of 7 months and 14 years and reported that CCT was 538 µm in children under 2 years old, 546 µm in children between 2 and 4 years, 565 µm between 5 and 9 years, and 555 µm between 10 and 14 years old. The mean CCT for all age groups was 549 µm(16). Our present results are similar to that study. As table 1 indicates, CCT was 556 µm in the first 2 years, 547 µm between 3 and 4 years, 564 µm between 5 and 8 years, and 553 µm between 9 and 12 years. We did not identify a gradual decrease or increase, unlike that reported in other studies(16,22,23) in terms of CCT during the first 12 years of life. The limitations of our study for CCT are an insufficient number of subjects and the extreme measurement results in age groups that make it difficult to obtain a linear algorithm.
In conclusion, axial length was 20.49 mm in first 2 years. It was increasingly reached adult levels of approximately 22.66 mm during years 9-10. Lens thickness was 3.67 mm in first 2 years and continuously decreased to 3.51 mm up to 11-12 years old. Central corneal thickness was 556 µm in the first 2 years, and 555 µm in years 11-12. There was no linear increase/decrease in central corneal thickness measurements, which may be due to an insufficient subject number and extreme values in age groups.
The results of this study may contribute to the literature, particularly in the aspect of understanding pediatric eye growth and treating the most common surgical entity (congenital cataract) in early childhood period.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

