INTRODUCTION
Keratoconus is a corneal ectatic disease where the cornea assumes a conical shape because of thinning, inducing irregular astigmatism and leading to marked impairment of vision. Keratoconus typically initiates at puberty and may progress, depending on individual characteristics, until the third or fourth decade of life; alternatively, it may commence later and arrest at any age. The disease is associated with several conditions, particularly those that encourage eye rubbing. This theory is supported by the fact that patients with keratoconus frequently have itchy eyes and ocular irritation. An autosomal dominant inheritance is reported in approximately 10% patients(1).
Keratoconus occurs in virtually every ethnic group. There is no gender predominance, and it almost always presents bilaterally, although the clinical features are frequently asymmetrical. The rate of progression varies between individuals and also between the two eyes. The severity at the stop of progression is also highly variable and can range from mild irregular astigmatism to severe thinning, scarring, and protrusion(1,2).
Several possible alternatives to manage keratoconic corneas have been reported in the literature, including gas-permeable contact lenses, intracorneal ring segment implantation, and corneal transplantation. However, these options have been limited to the treatment of the consequences of progressive corneal weakening, without any effect on the cause of the disease(2).
Corneal collagen cross-linking (CXL) has been established as an effective surgical treatment for increasing the biomechanical stability of the cornea to prevent the progression of corneal ectasia that occurs in keratoconus(3-5) or after laser refractive surgery(6,7). This technique uses a combination of riboflavin (vitamin B2) and ultraviolet A (UVA) light to induce cross-linking in the stromal collagen. There are two roles of riboflavin in this method. It works as a photosensitizer for the induction of cross-links and protects the underlying tissues from the deleterious influence of UVA irradiation(3-5). It is the only therapeutic approach designed to arrest the progression of disease(3,4).
The cornea is one of the most sensitive tissues of the body because it is densely innervated with sensory nerve fibers via the ophthalmic division of the trigeminal nerve through 70-80 long and short ciliary nerves. Apart from the important sensory functions, corneal nerves help in maintaining the functional integrity of the ocular surface by releasing trophic substances to promote epithelial homeostasis through activation of brain circuits that stimulate tear production and the blinking reflex(8). Given the crucial role of the corneal nerve in maintaining normal corneal structure and function, impaired corneal innervation may challenge the ability of the cornea to withstand surgical challenges, thus leading to a significantly increased risk of complications(9).
Evaluation of corneal sensitivity after corneal CXL with UVA irradiation is important to assess the efficacy and long-term effects of this treatment. In this prospective study, we evaluated the changes in corneal sensitivity after corneal CXL in patients with progressive early-stage keratoconus.
METHODS
Thirty-eight eyes of 19 patients (11 men and 8 women) with progressive early-stage keratoconus, transparent corneas, and a corneal thickness of ≥440 µm in the thinnest area were enrolled in a prospective, nonrandomized clinical study. According to the Amsler-Krumeich classification(10) of keratoconus, all eyes were considered to be in the early stages of keratoconus: 32 eyes (84.2%) were in stage I and 6 eyes (15.8%) were in stage II. An increase of 1.00 diopter (D) in maximum topographic K-value (Kmax) and a decrease in corneal thickness with or without changes in uncorrected visual acuity (UCVA) and best spectacle-corrected visual acuity (BSCVA) within the last year were considered as indications of progression. The mean patient age was 22 ± 2.7 years (range, 18-26 years). All procedures were performed by a single surgeon (BAN) at the Goiania Eye Institute, Goiania, GO, Brazil from January to December 2011.
Patients who fulfilled one of the following criteria after preoperative examination were excluded: age <16 or >35 years; presence of corneal scars or opacities, pregnancy or lactation, active anterior segment pathologic features, systemic connective tissue disease, ocular or systemic disease that can affect epithelial healing, and/or dry eye syndrome; and a history of corneal or anterior segment surgery. Patients using contact lenses were asked to discontinue lens use for at least 3 weeks before each examination.
Preoperative and postoperative examinations included the following: UCVA, BSCVA, slit-lamp biomicroscopy, Goldmann tonometry (Haag Streit, Bern, Swiss), fundus examination (Sigma 150K, Heine, Germany), specular microscopy (Konan, Hyogo, Japan), ultrasound pachymetry (CompuScanTM P, Storz, St. Louis, MO, USA), corneal sensitivity testing (Cochet-Bonnet® esthesiometer, Luneau, Paris, France), and corneal topography (Orbscan IIz, Technolas Perfect Vision GmbH).
The institutional ethics committee approved the study. All patients provided written informed consent in accordance with the Declaration of Helsinki after receiving a detailed description of the nature and risks of the procedure.
Treatment
Corneal CXL was conducted under sterile conditions in an operating room. All patients received a mild oral sedative (diazepam, 5 mg) 30 min before surgery and two drops of topical 0.5% proximetacaine 2 to 5 min before surgery. A wire eyelid speculum was placed for exposure. Corneal epithelium was removed by mechanical scraping over the central cornea (9.0 mm) with a blunt Paton spatula (Storz Ophthalmic Instruments, St Louis, USA).
The lid speculum was removed. Iso-osmolar 0.1% riboflavin solution (402.7 mOsmol/L), which was prepared by diluting 0.5% vitamin B2-riboflavin-5-phosphate with 20% dextran T500, was instilled into the cornea every 3 min for 30 min. Slit-lamp examination using a blue filter ensured the presence of riboflavin in the anterior chamber.
The lid speculum was replaced before irradiation. Fixation during irradiation was achieved by instructing the patient to focus on the light-emitting diode on the UVA emitter. The surgeon's thorough control ensured the patient's centration. UVA irradiation was performed for 30 min using a commercially available UVA system (UV-X, Peschke Meditrade) at a working distance of 5 cm, with an irradiance of 3 mW/cm2 corresponding to a surface dose of 5.4 J/cm2. During irradiation, iso-osmolar 0.1% riboflavin drops were applied every 5 min to ensure saturation of the cornea with riboflavin. A topical anesthetic agent (0.5% proximetacaine) was applied as required.
After this treatment, the patients were medicated with 0.3% topical moxifloxacin drops 4 times a day for 5 days and ketorolac tromethamine 3 times a day for 3 days. A soft therapeutic lens was applied until complete re-epithelialization of the cornea was achieved. Unpreserved artificial tears were recommended for mild irritation. Paracetamol-codeine pain medication was also prescribed as needed for the first 2 to 3 days. Fluorometholone eye drops were then applied 3 times a day for 2 weeks.
Using the Cochet-Bonnet® esthesiometer, central corneal sensitivity was measured before surgery, 7 days after surgery, and once a month after surgery until recovery of the baseline (preoperative) sensitivity level. A central corneal sensitivity of >40 mm was considered normal(11). Full recovery was considered as the recovery of the preoperative level of corneal sensitivity. The Cochet-Bonnet® esthesiometer comprises a nylon filament measuring 60.0 mm in length and 0.12 mm in diameter. The force exerted by the filament when it touches the cornea is inversely proportional to its length. All measurements were obtained by the same experienced observer. Patients lay in the supine position looking straight ahead, and they were asked to indicate when the stimulus was felt. The filament was moved toward the cornea smoothly at a perpendicular angle, guided by its corneal reflection. Contact was detected by a slight bending in the filament. If there was no patient response to the first contact, the length of the filament was decreased by 5.0 mm to increase its rigidity, and the procedure was repeated until the patient reported the feeling of corneal contact. The mean filament length from a minimum of 3 stimulus applications that elicited a positive response from the patient was considered to be the corneal touch threshold(11,12).
Statistical analysis was performed using SPSS 17.0 (SPSS, Inc.) software. The paired t-test was used to check the significance of the difference between two dependent groups in every continuous variable. A p-value of <0.05 was considered statistically significant.
RESULTS
After treatment, complete re-epithelialization was observed within 4 days in all patients.
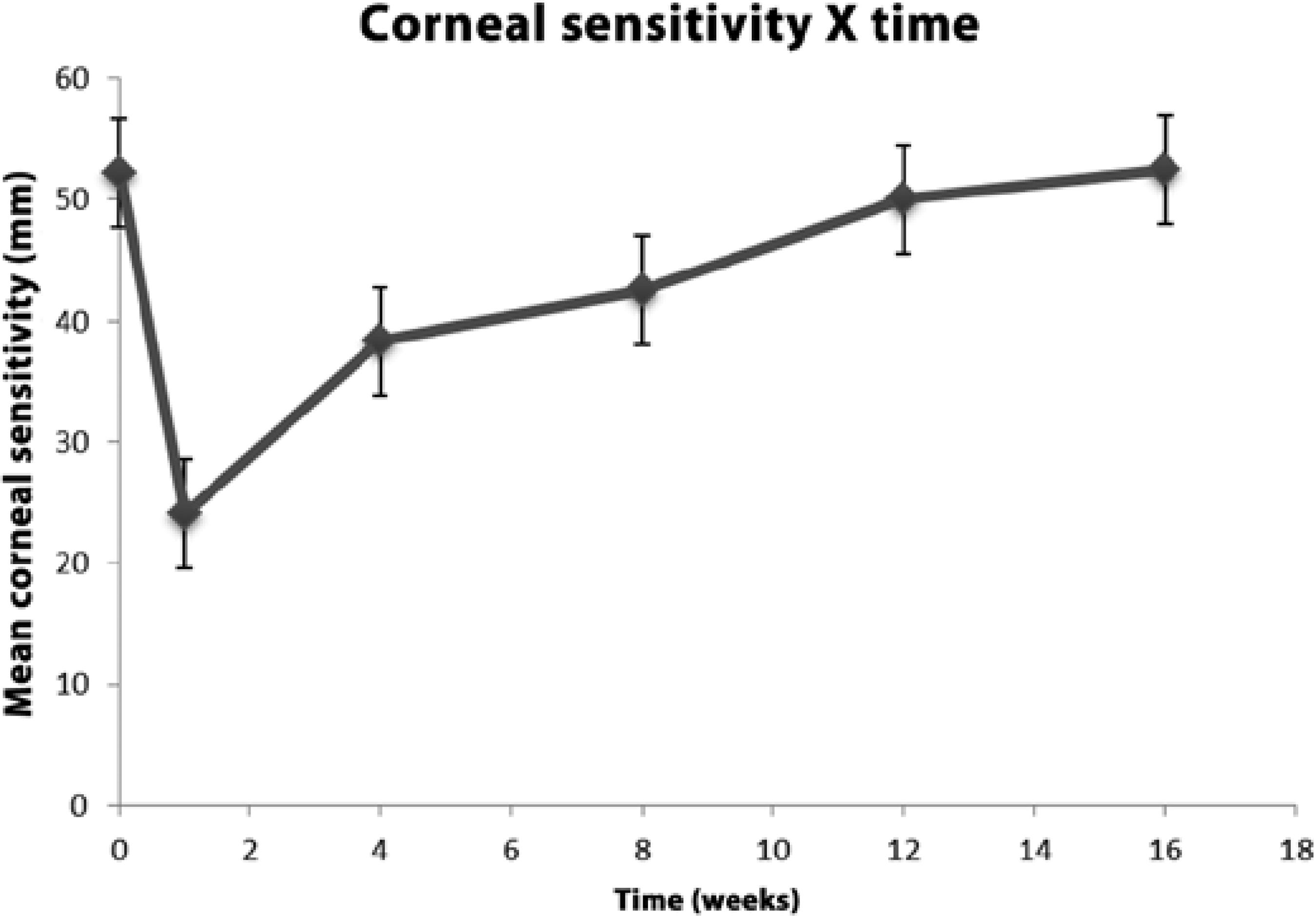
Corneal sensitivity gradually returned to preoperative levels in all treated eyes. The mean central corneal sensitivity was 52.24 (±6.44) mm before surgery, 24.08 (±7.78) mm 7 days after surgery, and 38.29 (±4.23), 42.50 (±3.02), 50.00 (±3.07), and 52.50 (±2.78) mm 1, 2, 3, and 4 months after CXL, respectively. Normal levels of corneal sensation, but not a return to baseline (preoperative) levels, were noted 2 months after surgery (p=0.000). Statistical analysis showed a significant decrease in corneal sensitivity for up to 3 months after surgery. Preoperative levels were observed at 3 (p=0.081) and 4 months after surgery (p=0.817; Figure 1).
Four months after corneal CXL, 3 eyes (7.9%) experienced 1-line improvement in postoperative BSCVA. It did not change in 33 eyes (86.84%) and decreased by 1 line in 2 eyes (5.2%). No statistically significant difference was noted between preoperative and postoperative BSCVA values (p=0.571).
Sixteen eyes (42.2%) experienced a 1-line improvement in postoperative UCVA. One eye lost 1 line and another lost 2 lines in UCVA. No statistically significant improvement was observed between preoperative and 4-month postoperative results (p=0.092).
Four months after surgery, comparison of preoperative and postoperative results showed a statistically significant difference between some of them. The mean thickness as assessed by central corneal pachymetry decreased from 478 ± 24.8 µm to 454 ± 29.06 µm (p=0.00). The mean spherical equivalent decreased from -2.08 ± 0.85 D to -1.92 ± 0.84 D (p=0.00), and the mean maximum topographic K-readings (Kmax) dropped from 51.45 ± 1.77 D to 50.18 ± 1.64 D (p=0.00). No other data showed significant differences before and after surgery. The mean minimum topographic K-readings (Kmin) changed from 45.49 ± 1.79 D to 45.48 ± 1.81 D (p=0.860). The mean intraocular pressure changed from 11.66 ± 1.23 mmHg to 11.50 ± 1.24 mmHg (p=0.279), and the endothelial cell counts changed form 2280.26 ± 258 to 2287 ± 270 cells/mm2 (p=0.549). The mean patient data before and after cross-linking are shown in table 1.
Table 1 Mean corneal pachymetry values, spherical equivalents, topographic K-readings (Kmax and Kmin), intraocular pressure, and endothelial cell counts before andafter corneal cross-linking
| Before corneal CXL | Four months after surgery | p-value | |
|---|---|---|---|
| Pachymetry values | 478 ± 24.8 µm | 454 ± 29.06 µm | 0.00 |
| (440-508 µm) | (420-488 um) | ||
| Spherical equivalents | -2.08 (±0.85) D | -1.92 (±0.84) D | 0.00 |
| Kmax | 51.45 ± 1.77 D | 50.18 ± 1.64 D | 0.00 |
| Kmin | 45.49 ± 1.79 D | 45.48 ± 1,81 D | 0.860 |
| Intraocular pressure | 11.66 ± 1.23 mmHg | 11.50 ± 1.24 mmHg | 0.279 |
| Endothelial cell counts | 2280.26 ± 258 mm2 | 2287 ± 270 mm2 | 0.549 |
No intraoperative, early postoperative, or late postoperative complications were observed in this series of patients. After 4 months, all corneas remained transparent, without any scar in the stroma.
DISCUSSION
Many corneal surgical procedures have been associated with a temporary decrease in corneal sensitivity due to amputation or laser ablation of the corneal nerves. This damage may contribute to the development of dry eye, impaired epithelial wound healing, increased epithelial permeability, and ocular surface changes after the procedure. In such cases, the corneal sensitivity usually returns to normal within 3-12 months after surgery(9,13).
Increased visibility of nerve fibers by slit lamp biomicroscopy has been demonstrated in patients with keratoconus. Corneal nerves pass between the stroma and epithelium at sites of early degradative change. The keratocytes wrap around the nerves as they pass through an otherwise acellular Bowman's layer. Localized nerve thickening develops in the epithelium and stresses the epithelial architecture(14). In vivo laser scanning confocal microscopy has revealed decreased innervation and decreased cell density in all layers of the keratoconic cornea(15). The sub-basal nerve plexus architecture isaltered with fragmentation of the plexus, increased sub-basal nerve tortuosity, decreased central nerve fiber density, and a correlation between the decrease in nerve density decrease and severity of disease(16-18). Another study(19) reported decreased sensitivity in all corneal zones of patients with keratoconus, and the decrease depended on the severity of the condition. Injured nerve fibers may quickly regenerate and may exhibit abnormal responses because of the altered expression of ion channel proteins in the regenerating nerve terminals(20).In the current study group, according to the Amsler-Krumeich classification(10) of keratoconus disease, all eyes were considered to be in early-stage keratoconus: 32 eyes (84.2%) were in stage I and 6 eyes (15.8%) were in stage II. Therefore, faster corneal sensitivity recovery was expected.
Corneal CXL with riboflavin and UVA irradiation is a technique of a minimally invasive nature that is used for the stabilization of different types of corneal ectatic disorders. This technique augments the mechanical rigidity of the cornea by inducing cross-links at the corneal stroma(3-5). Removal of the epithelium has been recommended as an initial step in the CXL procedure because its lipophilic nature decreased the diffusion of riboflavin into the corneal stroma(4,5). Moreover, the epithelium may block the UV rays(3). The photosensitizer riboflavin is applied to the de-epithelialized surface of the cornea and is allowed to penetrate the corneal stroma(3-6). Subsequent exposure of the cornea to UVA light is believed to result in photodynamic cross-linking when riboflavin, excited by UVA, creates free radicals leading to collagen cross-linking(4,5).
An in vivo confocal laser scanning microscopy study(16) has demonstrated that the anterior subepithelial stroma was recolonized by nerve fibers, with the restoration of corneal sensitivity, 6 months after CXL using the epithelium-off technique. An animal study(17)of corneal sensitivity and innervation after CXL in rabbits has also shown that corneal sensitivity was significantly decreased 3 days after UVA irradiation with de-epithelialization treatment. Corneal sensitivity in the central region of the cornea decreased to the lowest level 7 days after treatment and returned to normal 3 months after the procedure; the corneal nerve fiber density appeared normal after 6 months. A recent prospective, interventional case series(21)evaluated the effects of CXL on corneal innervation, sensitivity, and tear function in patients with progressive early-stage keratoconus. The study detected prominent hypoesthesia 1 month after surgery, which gradually recovered by 9 months after surgery; the time course was similar for both sensitivity restoration and corneal nerve regeneration. Another study(22) evaluated the changes in corneal tactile sensitivity following corneal collagen cross-linking in patients with progressive keratoconus and concluded that corneal CXL performed in keratoconus patients induced a considerable decrease in corneal sensitivity. This decrease was greater in the first week after the procedure, with progressive recovery for up to 6 months of follow-up. Our results demonstrated that normal levels of corneal sensation that were not yet baseline (preoperative) levels were observed two months after surgery, and significant transient hypoesthesia was observed for as long as 3 months after CXL. The difference in the time of corneal sensation recovery between the different studies may be related to other factors such as the degree of ectasia, contact lens use, and systemic disease that can affect epithelial healing or corneal sensitivity.
Contact lens wear decreases corneal sensitivity(23). To minimize any effect on measurements, patients using contact lenses have been asked to discontinue lens use for at least 3 weeks before each examination.
Corneal sensation is also decreased in patients with diabetes and mild to moderate somatic neuropathy, and it progresses with the severity of neuropathy. These findings have important clinical implications with regard to the development of corneal abnormalities in patients with diabetes(24). Therefore, patients with systemic disease that can affect epithelial healing and corneal sensitivity, such as diabetes, were excluded from our study.
An important finding of this study was a significant decrease in corneal thickness after corneal CXL, which may also have contributed to the decrease in corneal sensitivity. Our group(25) recently described transient corneal thinning after corneal CXL with UVA irradiation and a hypo-osmolar riboflavin solution in thin corneas (<400 µm) for progressive keratoconus. In our analysis of changes in corneal thickness over time, pachymetric values decreased until 1 month after surgery and appeared to increase thereafter. Six months after treatment, no statistically significant difference was found between postoperative and baseline values. The physiology of this initial thinning and subsequent rethickening remains unclear. Epithelial removal may increase the rate of water evaporation from the stroma and renders the cornea vulnerable to thinning because the stroma has no dehydration resistance(26). Epithelial remodeling, anatomical and structural changes in corneal collagen fibrils(27), and keratocyte apoptosis(28) may also be implicated. Surgeons must be aware about postoperative thinning of the cornea after CXL, particularly in thinner corneas. Ours results suggest that further studies are necessary to evaluate the relationship between the decrease in corneal thickness and transient corneal hypoesthesia after CXL.
A few potential limitations were apparent in this study, with the small sample of studied eyes and the absence of a control group of patients being the major ones. However, because all patients presented with bilateral progressive keratoconus, it was considered unethical to leave the disease untreated in one eye. Esthesiometry is a reproducibly accurate measure of corneal sensation. The most popular device for this purpose is the Cochet-Bonnet esthesiometer, which comprises a calibrated nylon filament for mechanical stimulation(11). It has limitations in its sensitivity as a test, but it is the most practical method available(12). The conclusions of this study should be interpreted within the limits of this method of evaluation.
Touching the cornea triggers one of the most sensitive protective reflexes of the human body. The threshold of sensitivity, particularly in the center of the cornea, is exceedingly low; therefore, pathological changes can be diagnosed early and precisely and can be used for diagnosis and follow-up and to assess the prognosis of various corneal disorders. The loss of normal corneal sensation may compromise the protective blink reflex, delay epithelial wound healing, decrease tear flow, and show an association with neurotrophic keratitis, sterile corneal melts, and infectious keratitis(11,28).
CONCLUSIONS
The results of this study emphasized the slow and gradual recovery of corneal sensitivity after CXL, as observed in other studies published in the literature. These observations can help to direct studies to better define the risk and management of persistent epitheliopathy and dry eye symptoms after CXL.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

