INTRODUCTION
Multiple primary tumors (MPT) are rare and have different clinical presentations. Historically, Warren and Gates defined MPT as tumors that are histologically confirmed as malignant, separated by at least 2 cm of normal mucosa, and/or chronologically separated by at least 5 years, excluding metastatic tumors. When tumors develop simultaneously or within 6 months after discovery of the primary tumor, they are considered to be synchronous tumors. If this period exceeds 6 months, they are defined as metachronous tumors(1). The most common findings are related to the presence of 2 tumors, and the gastrointestinal tract, breast, and skin are the most commonly involved primary sites. In the scientific literature, there are few descriptions of lymphoma as one of the primary types of MPT, and an association with the mantle cell lymphoma subtype is even more infrequent and results in a worse prognosis(1,2).
The term mantle cell lymphoma was first used in 1993 to describe the specific subtype of non-Hodgkin B-cell lymphoma with specific clinical and histopathological characteristics(3). It accounts for 3%-7% of all non-Hodgkin lymphomas and 1%-9% of all lymphomas in the periocular region(3-5). This disease primarily affects men aged over 60 years and is usually a widespread and aggressive tumor(3,4). Because of its rarity, most of the descriptions in the literature are case reports, with some cases described in a large case series of lymphoma(4,6).
Here we present an atypical case of metachronous MPT associated with basal cell carcinoma of the skin, intestinal adenocarcinoma with regional lymph node metastasis, and non-Hodgkin B-cell mantle cell lymphoma of the bilateral orbits with systemic findings.
CASE REPORT
A 73-year-old man who was retired and born and raised in São Bernardo do Campo, São Paulo, presented with a complaint of bilateral eyelid edema with low visual acuity since 1 year and 6 months. The symptoms had first appeared on the left and progressed to the right. His family history included a brother who died of an abdominal tumor (exact type unknown). His ophthalmological history included bilateral cataract surgery performed 5 years back. His past medical history included non-Hodgkin B-cell small cell lymphoma diagnosed in the first semester of 2010 through pleural biopsy and cervical lymph node involvement (Figure 1A and 1B); basal cell carcinoma diagnosed in the second semester of 2010 through biopsy of the skin over the right and left scapular area, left forehead, and chin (Figure 1C and 1D); and intestinal adenocarcinoma diagnosed in January 2011 through histopathological analysis of a piece of intestine removed during emergency surgery (right hemicolectomy and bowel resection for perforated acute abdomen), with regional lymph node metastases (Figure 1 e and 1F).
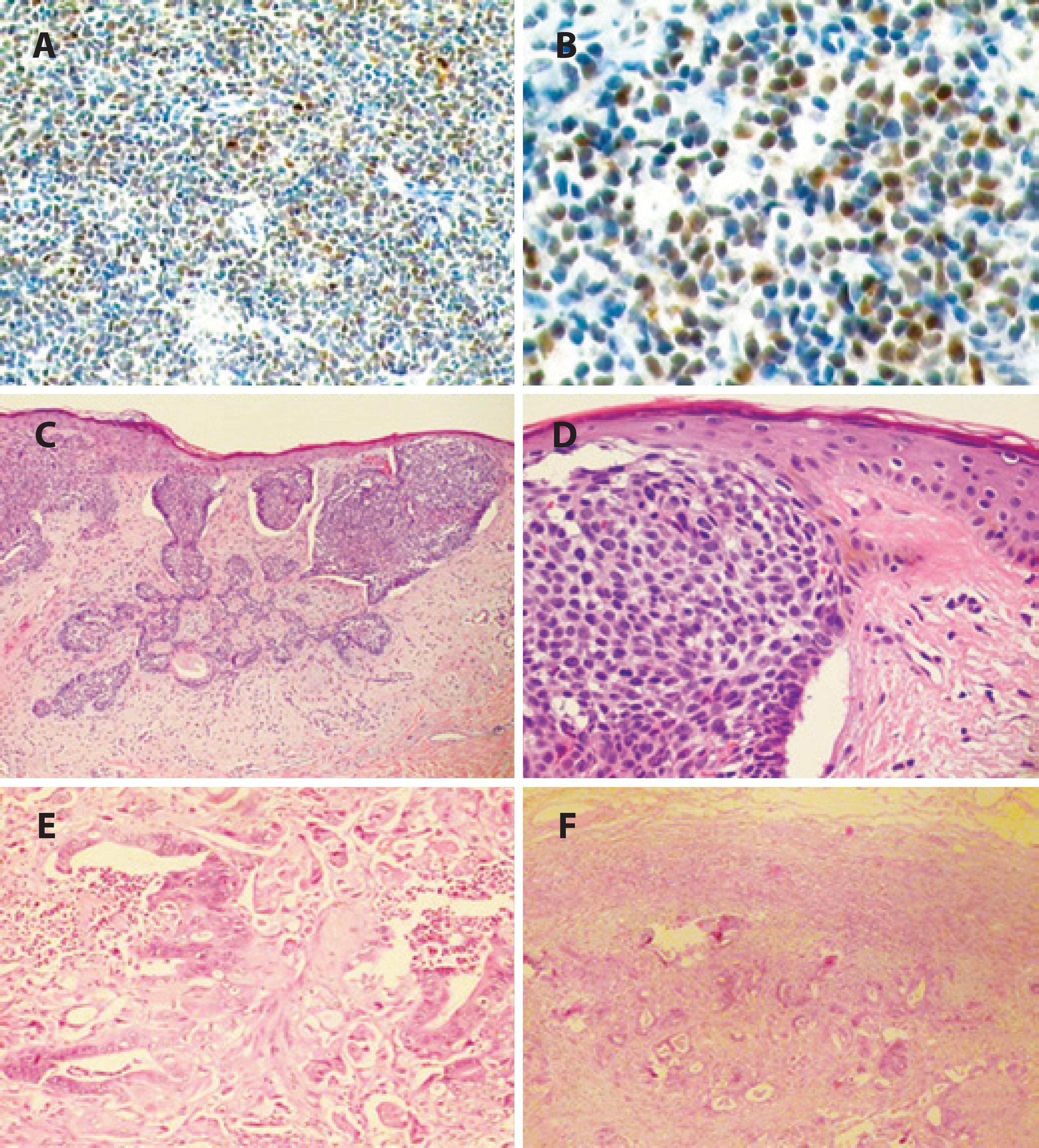
Figure 1 A and B) Biopsy of the involved thoracic lymph node reveals positivity for cyclin D1 with nuclear immunostaining. C and D) Biopsy of the skin over the scapular region reveals basal cell carcinoma with infiltration of the basal membrane. E) Biopsy of the bowel shows intestinal adenocarcinoma, moderately differentiated, with mitosis and increased cell nuclei. F) Biopsy of the abdominal lymph node capsule shows metastasis of the intestinal adenocarcinoma, with intestinal glands
Ectoscopy revealed bilateral proptosis, bilateral bulging in the upper and lower eyelid regions, which was more prominent on the left, and the presence of a solid lesion that was adherent to the deep planes and painless after significant reduction of the palpebral fissure (Figure 2). Uncorrected visual acuity was 20/50 in the right eye and 20/25 in the left eye. Anterior biomicroscopy revealed mucoid secretion with entropion of the lower eyelid on both sides. Intraocular pressure, fundoscopy, and ocular motility examinations were not performed because of technical difficulties.

Figure 2 Ectoscopy findings. There is bilateral bulging in the upper and lower eyelid region, more prominently on the left, with mucoid secretion.
The patient underwent computed tomography and magnetic resonance imaging of the orbit (Figure 3). Incisional bilateral eyelid biopsy was performed in February 2013 (Figure 4). Hematoxylin-eosin staining revealed relatively homogeneous small cells with slight nuclear irregularity. Immunohistochemistry was positive for CD5, CD20, and cyclin D1. On the basis of these findings, a diagnosis of non-Hodgkin B-cell mantle cell lymphoma was made.
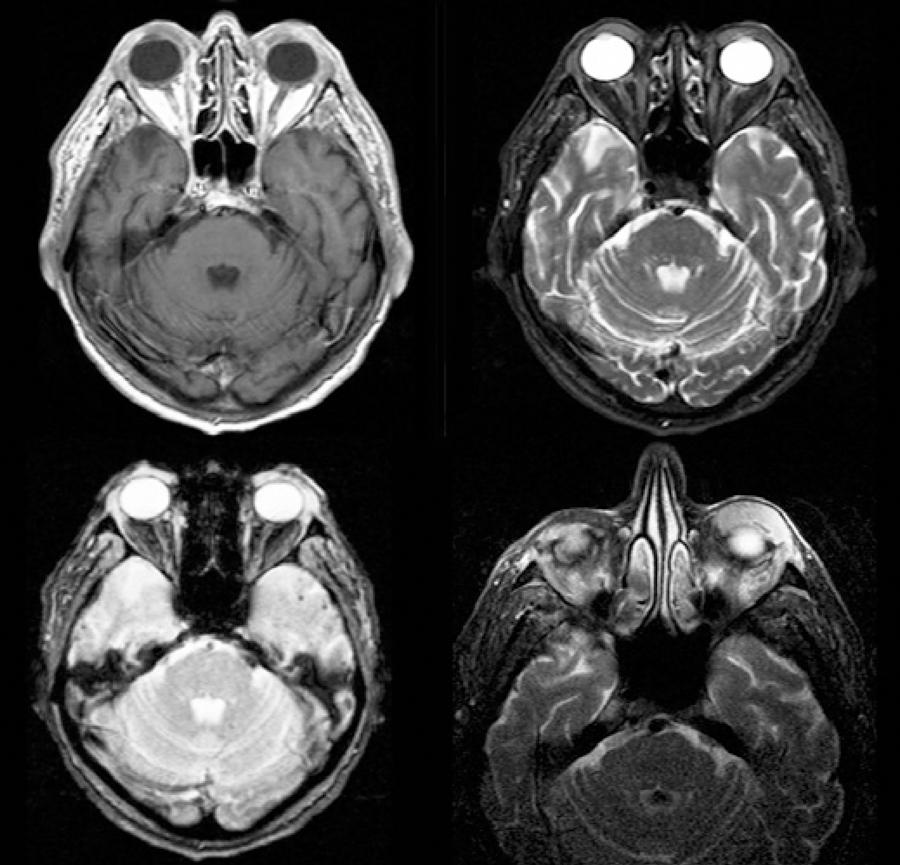
Figure 3 Magnetic resonance imaging of the orbit: The image shows bilateral eyelid thickening, which is more pronounced on the left, and a lesion involving the eyeball, which is hypointense relative to fat on a T1 image and hyperintense on a T2 image, with contrast enhancement (gadolinium).
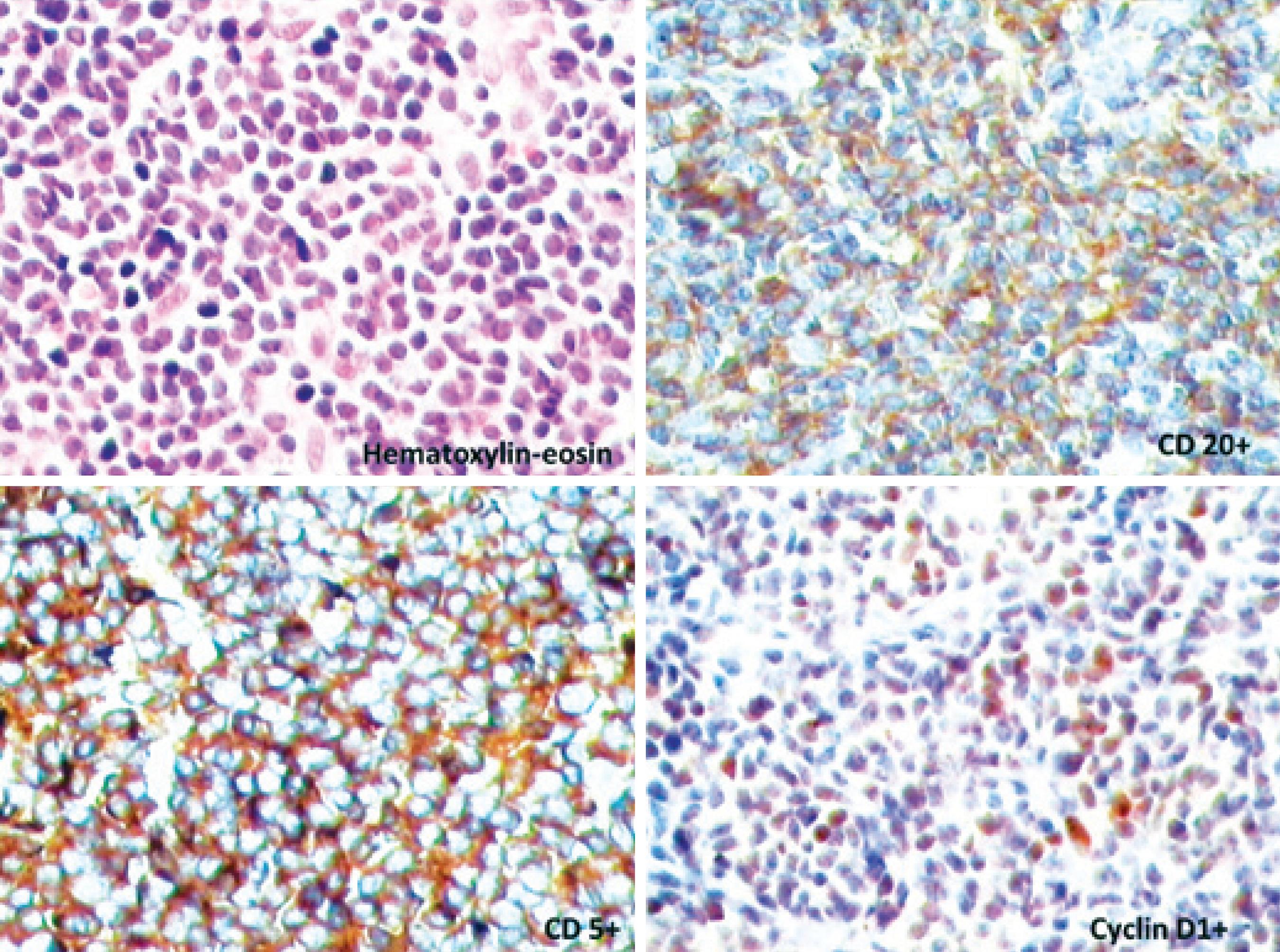
Figure 4 Incisional eyelid biopsy: Hematoxylin-eosin staining shows a relatively homogeneous population of small cells with slight nuclear irregularity. Immunohistochemistry is positive for CD5, CD20, and cyclin D1.
The patient was referred to the Oncology Sector at UNIFESP, where he began his treatment with 3 cycles of CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone), 6 cycles of FCR (fludarabine, cyclophosphamide, and rituximab), and radiotherapy The patient is being followed-up by a multidisciplinary team.
DISCUSSION
MPT affects approximately 1.3%-2.5% patients diagnosed with malignancy, and patients with ≥3 MPTs account for 0.16%-0.26% of this total(1,7). Although the lesions described in the literature primarily involved the gastrointestinal tract, breast, and skin (non-melanoma), other sites can also be affected. Pandurengan et al.(8) described a case of gastrointestinal stromal tumor associated with gastric lymphoma, while Troyanova et al.(9) described an increased risk of MPT in Bulgarian patients diagnosed with malignant non-melanoma of the skin, primarily affecting the head and neck, thyroid, lung, larynx, bladder, colon, melanoma, and non-Hodgkin lymphoma. Dasanu et al.(2) reported a case of pancreatic adenocarcinoma associated with mantle cell lymphoma; this was the only case we found in PubMed and Bireme describing MPT involving the specific subtype of mantle cell lymphoma, similar to the present case. Our first tentative diagnosis was based on the patient's personal history and was orbital metastasis. In our patient, any of the malignancies could be the origin of metastasis, indicating the importance of biopsy for histological confirmation.
Systemic lymphomas (nodal and extranodal) can spread to the ocular adnexa. When there is ocular involvement secondary to a systemic lymphoma, the uvea is almost exclusively the affected site (choroid, ciliary body, and iris)(5). However, ocular adnexal lymphomas have not been associated with intraocular lymphomas. They are generally indolent, painless, and well tolerated and mold to the adjacent structures without bone destruction in imaging studies(5). Rasmussen et al.(4) related the most common symptoms of mantle cell lymphoma in the orbital and adnexal region: irritation, pain, and epiphora. They also referred to eyelid masses, conjunctival swelling, and proptosis as the most frequent signs. Our patient complained of bilateral eyelid swelling, low visual acuity, and an orbital mass. Because this was a specific subtype of lymphoma, we believed that the orbital tumor in our patient was a metastasis of non-Hodgkin B-cell small cell lymphoma of the cervical lymph nodes. A factor in favor of this hypothesis is the rarity of the presence of two primary malignant tumors in the orbit; however, we have to remember that the primary sites for orbital metastasis are the breasts, lungs, and prostate. Our patient also presented with intestinal adenocarcinoma, which can metastasize to the orbit; however, this type of involvement is very rare. In such cases, imaging findings have been related to osseous changes such as hypo- or hyperostosis primarily located intra- or extraconally and occasionally involving the extraocular muscles. These characteristics were not found in the case presented(10).
Mantle cell lymphoma is a distinct subtype of non-Hodgkin B-cell tumors that primarily affect elderly men, unlike the majority of periocular lymphomas, which are more common in older women(4,6). As observed in our case, approximately one- to two-thirds of patients report a previous diagnosis of systemic lymphoma at diagnosis; for the remaining third, the diagnosis is made when the disease is already widespread. This characteristic also differentiates it from other orbital lymphomas(4). Approximately 32%-71% of these tumors are bilateral, and the eyelid, orbit, and conjunctiva are the most involved regions(3-5). The bone marrow is involved in 50%-70% cases at diagnosis(4). In most cases, there is involvement of more than one site in the orbital region or the ocular adnexa(4). The most frequent signs and symptoms are irritation, ptosis, eyelid edema or mass, proptosis, pain, and diplopia; other less common findings include a mass in the region of the lacrimal gland, chemosis, conjunctival hyperemia, ocular motility alteration, tearing, and malalignment of the eyeball(3,4). Only 50% patients have a survival rate of >5 years(3,4).
There are some characteristic immunohistochemical markers (CD5+, CD20+, bcl-2+, CD21+ dendritic form, CD43+, CD23-, CD10, CD11c-, and CD25-) and genetic patterns characterized by the translocation t(11;14)(q13,q32), which causes overexpression of the CCND1 gene and the protein cyclin D1(3-5). However, some authors have described atypical cases that were immunohistochemically negative for CD5(3). Coupland et al. showed p16 expression in 2 patients.6 Histologically, this lymphoma is characterized by small cells with irregular and hyperchromatic nuclei and scant cytoplasm(6).
The European Task Force on Lymphoma has defined 3 types of mantle cell lymphoma growth patterns: diffuse (most common), nodular, and marginal zone(3,4). Some studies have shown that the marginal zone pattern is related to better prognosis, while others have demonstrated that all patterns have a similar prognosis(3). In fact, the prognosis is usually poor, with poor response to treatment, bone marrow involvement, and short survival duration. The poor prognosis is associated with increased mitotic activity (>20 mitoses/10x field), blastic morphology, peripheral involvement (atypical cells in the peripheral blood), and increased p53 expression(3,5). A few years ago, it was considered an untreatable disease with only palliative care options available, but nowadays, several types of treatments are being studied. Recently, some studies showed a response to combined therapy with multiple chemotherapy regimens and rituximab (anti-CD20) in patients with an early diagnosis; other researchers have seen good results with bone marrow transplantation(3,4).
In conclusion, mantle cell lymphoma is a rare disease, usually widespread, and carries a poor prognosis. Physicians should consider this malignancy as a differential diagnosis for neoplasms of the orbit. Rapid and accurate diagnosis by clinical and immunohistochemical tests is essential before referral of the patient for systemic evaluation and treatment. This case report described an extremely rare occurrence, and in our knowledge, it represents the first case described in the scientific literature on metachronous MPT with bilateral non-Hodgkin B-cell mantle cell lymphoma of the orbit in a Brazilian patient.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

