INTRODUCTION
Corneal laser surgery is currently the most widely used surgical method for correcting refractive errors. Measurement of the corneal curvature, thickness, and elevation are important for the preoperative assessment of patients requiring refractive surgery and for the diagnosis of corneal ectasias like keratoconus and pellucid marginal degeneration. Historically, a simple Placido-based corneal topography was considered the norm for screening the cornea for topographic anomalies. Currently, Scheimpflug and Placido systems are being used to provide information on the anterior and posterior corneal surfaces. Currently, 2 such systems are widely used: the Galilei Dual Scheimpflug Analyzer (Ziemer, SIS, Port, Switzerland) and the Pentacam (OCULUS Optikgeräte GmbH, Germany) single Scheimpflug analyzer.
The present study aims to evaluate the agreement in measurements obtained by these 2 systems. Previous studies have evaluated the agreement between Scheimpflug devices; however, different best-fit sphere (BFS) diameters were used in both devices(1) or only elevation data were compared between the Dual Scheimpflug Analyzer and a Scanning Slit-beam imaging system(2). Comparisons using different BFS would alter the elevation data obtained by the single Scheimpflug system (compared with the dual Scheimpflug system) because the reference is flatter. Now that the pre-set BFS diameter in the single Scheimpflug system is universally set to 8.0 mm, we attempted a comparison with equal BFS diameters in both systems. Our aim was not to demonstrate the superiority of one system over the other, but to discuss the similarities between both systems.
METHODS
This prospective, noninterventional, diagnostic study comprised 60 eyes of normal candidates for refractive surgery. Patients who had undergone previous ocular surgeries, those with any systemic disease (including diabetes mellitus, connective tissue disease, hypertension, and collagen vascular diseases), and/or those who had worn rigid contact lenses in the past 6 months were excluded. Soft contact lens wearers were asked to discontinue wearing their contact lenses for at least 14 days prior to measurements(3). The study received the approval of the Institutional Review Board of the American University of Beirut and complied with the Health Insurance Portability and Accountability Act (HIPAA) recommendations. Informed consent was obtained from all patients. All subjects underwent corneal topography using the Galilei (dual Scheimpflug system) followed by corneal topography using the Pentacam (single Scheimpflug system) by the same trained ophthalmic technician who was blinded to the study protocol.
Pentacam (single Scheimpflug system)
The Pentacam system uses a single rotating Scheimpflug camera (180º) and a monochromatic slit-light source [blue light-emitting diode (LED) at 475 nm] that rotate together around the optical axis of the eye to calculate a 3-dimensional (3D) model of the anterior segment. The 3D, high-resolution, cornea-scanning mode obtains 50 images of the eye in 1 second. Overall, 138,000 true elevation points were recorded.
Galilei (dual Scheimpflug system)
The Galilei Dual Scheimpflug Analyzer uses two rotating Scheimpflug cameras integrated with a Placido topographer. The light source is also monochromatic (blue LED at 475 nm). The 122,000 data points are analyzed per scan. The system used Scheimpflug images of all anterior segment structures (cornea, iris, pupil, anterior chamber, and lens) to evaluate and analyze the corneal shape and thickness, pupil size, and anterior chamber parameters (size, volume, and angle). The presence of two Scheimpflug camera devices that obtain images of the same part of the eye simultaneously decreases movement artifacts and increases image accuracy by superimposing the two images. The presence of the Placido improves the accuracy of calculation of the anterior corneal curvature.
Measurement technique
Measurements were obtained in a semi-lit room. To standardize the tear film meniscus and account for tear film abnormalities that may influence Placido measurements, a drop of carboxymethyl cellulose artificial tears was instilled in the fornix of each eye, and measurements were obtained 3 min later to ensure that the tear film meniscus was back to its normal thickness(4). Both eyes were measured. Measurements were obtained using an 8.0-mm diameter BFS, which was fitted in float. Central elevations and maximum/minimum elevations in the central 8 mm of the cornea were recorded with both the dual and single Scheimpflug systems. Pachymetry measurements were internally calculated by the individual machines by subtracting the anterior and posterior corneal elevations. In patients with a normal topography, only one eye was considered for analysis (60 eyes of 60 patients). Data from the right eyes of the first, third, and fifth 10 patients and data from the left eyes of the second, fourth, and sixth 10 patients were used for further analysis.
Intraclass correlation coefficients (ICCs)
For each system and for a defined subset of apparently healthy eyes, measurements were obtained 3 times and the data were averaged. One eye of each subject was selected. Ten right eyes were selected from the first 10 subjects and 10 left eyes were chosen from the second 10 subjects. The internal repeatability of each machine was analyzed by calculating the ICC, which was defined as the ratio of the between-subjects variance to the sum of the pooled within-subject variance and between-subjects variance. The ICC, which approached 1.0 when there was no variance between repeated measurements, was automatically calculated using PASW Statistics software (SPSS version 18.0, SPSS Inc. Chicago, IL, USA). The ICCs ranged from 0 to 1 and were commonly classified as follows: ICC <0.75, poor agreement; 0.75-<0.90, moderate agreement; and >0.90, high agreement(5).
Statistical analysis
Statistical analysis was performed using the Statistical Program for Social Sciences v18.0 (SPSS v18.0, SPSS Inc. Chicago, IL, USA). A paired t-test was used to compare the instruments in each elevation parameter. Mean algebraic and mean absolute differences were calculated. Results are expressed as means ± standard deviations. In addition, Pearson's correlation coefficients (PCCs) were calculated to assess the correlation between the anatomical parameters measured by each imaging technique. All tests were 2-tailed. A p-value of <0.05 was considered statistically significant. Bland-Altman plots were used to assess the interchangeability (agreement) of the 2 imaging systems for measuring elevation parameters. These plots show the differences between the methods plotted against the mean of the methods. They provided a graphical method to assess the presence of an agreement between the 2 clinical techniques.
RESULTS
Patient characteristics
Sixty eyes of 60 subjects (25 males, 35 females) were included in the study. The mean age of the participants was 27.0 ± 4.1 years. All eyes had a normal topography, with no evidence of curvature abnormalities.
Machine characteristics
Each measurement was obtained 3 times, and only the findings with the highest quality (as determined by the machine) were included for analysis. The ICC was calculated for each machine on the basis of 3 measurements. The ICC for the dual Scheimpflug system was as follows: 0.999 for pachymetry (CCT), 0.998 for SimK, 0.998 for anterior BFS, and 0.993 for posterior BFS. The ICC for the single Scheimpflug system was as follows: 0.994 for CCT, 0.986 for SimK, 0.996 for anterior BFS, and 0.991 for posterior BFS.
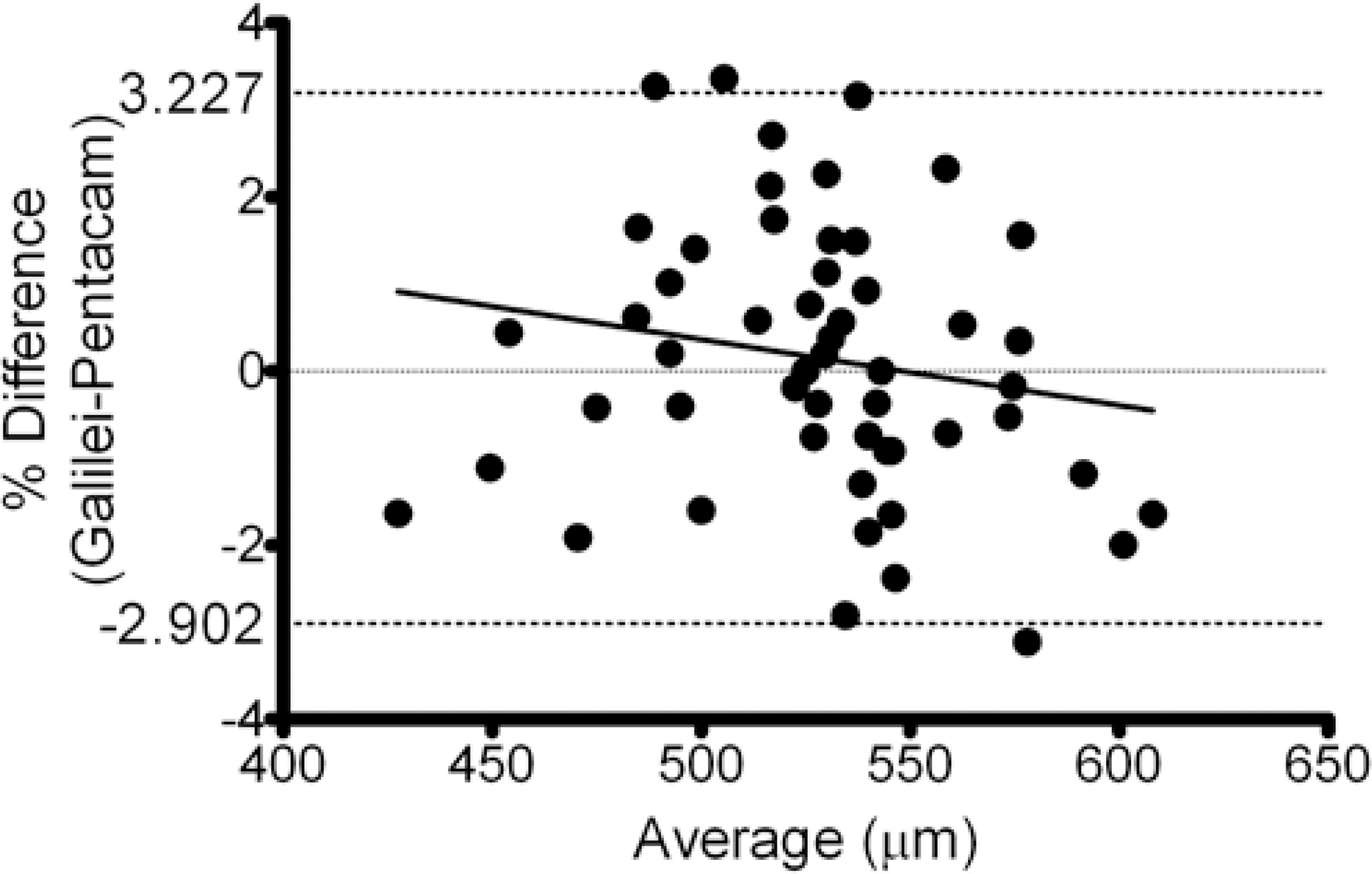
Pachymetry
Pachymetry measurements are summarized in table 1. The mean difference between the dual Scheimpflug and single Scheimpflug systems in central pachymetry measurements was 0.7 ± 8.2 µm. The mean absolute difference between the two machines in central pachymetry measurements was 6.7 ± 4.6 µm. Figure 1 shows a Bland-Altman plot of central pachymetry. The dual Scheimpflug system exhibited a trend for displaying values larger than those displayed by the single Scheimpflug system for corneal thicknesses below 550 µm. It also exhibited a tendency to display smaller measurements at higher mean central pachymetry measurements. The PCC for central corneal thickness was 0.977.
Table 1 Correlation of pachymetry measurements between the dual Scheimpflug system (Galilei) and the single Scheimpflug system (Pentacam)
| (µm) | Galilei (µm) | Pentacam (µm) | Pearson's correlation coefficient |
|---|---|---|---|
| Central pachymetry | 535 ± 35 | 534 ± 37 | 0.977 |
| Thinnest point | 531 ± 37 | 528 ± 43 | 0.982 |
| Superior 2 mm | 574 ± 33 | 590 ± 33 | 0.864 |
| Inferior 2 mm | 568 ± 38 | 559 ± 43 | 0.949 |
| Nasal 2 mm | 578 ± 32 | 579 ± 34 | 0.897 |
| Temporal 2 mm | 549 ± 33 | 553 ± 34 | 0.904 |
| Superior 3 mm | 612 ± 35 | 649 ± 37 | 0.889 |
| Inferior 3 mm | 613 ± 35 | 613 ± 39 | 0.865 |
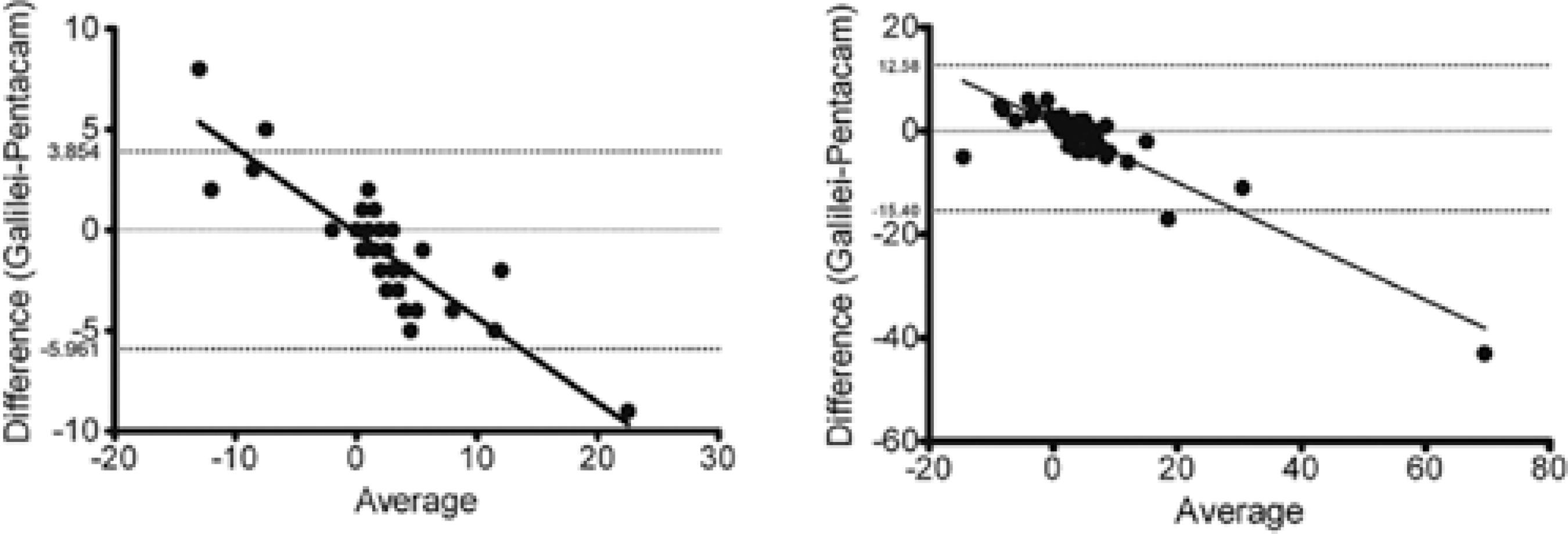
Anterior and posterior elevation
The anterior elevation measurements recorded by the 2 machines are summarized in table 2. Posterior elevation measurements recorded by the 2 machines are summarized in Table 3. The mean difference in between the dual and single Scheimpflug systems in central AE and central PE measurements was -1.04 ± 2.48 µm and -1.38 ± 7.08 µm, respectively. The mean absolute difference between the dual and single Scheimpflug systems in central AE and central PE measurements was 1.85 ± 1.86 µm and 2.77 ± 6.10 µm, respectively. Anterior and posterior Bland-Altman plots of central elevation are shown in figure 2. A similar trend was observed for pachymetry measurements, with the dual Scheimpflug system showing higher and lower values than the single Scheimpflug system for lower and higher elevations, respectively. The PCC for central anterior elevation was 0.952, while that for central posterior elevation was 0.974.
Table 2 Correlation of central anterior elevation measurements between the dual Scheimpflug system (Galilei) and the single Scheimpflug system (Pentacam)
| (µm) | Galilei | Pentacam | Pearson's correlation coefficient |
|---|---|---|---|
| Central elevation | 2.48 ± 2.98 | 4.23 ± 4.57 | 0.952 |
| Superior 2 mm | -8.05 ± 10.43 | -8.25 ± 12.79 | 0.933 |
| Inferior 2 mm | -1.10 ± 6.06 | 1.35 ± 12.81 | 0.871 |
| Nasal 2 mm | 0.35 ± 4.14 | -0.55 ± 5.01 | 0.784 |
| Temporal 2 mm | 1.30 ± 4.37 | 1.68 ± 4.49 | 0.749 |
| Superior 3 mm | -8.43 ± 8.73 | -12.08 ± 10.33 | 0.742 |
| Inferior 3 mm | -10.18 ± 9.89 | -9.30 ± 7.11 | 0.685 |
Table 3 Correlation of central posterior elevation measurements between the dual Scheimpflug system (Galilei) and the single Scheimpflug system (Pentacam)
| (µm) | Galilei | Pentacam | Pearson's correlation coefficient |
|---|---|---|---|
| Central elevation | 5.33 ± 7.69 | 7.15 ± 14.75 | 0.974 |
| Superior 2 mm | -20.43 ± 16.49 | -22.63 ± 24.59 | 0.961 |
| Inferior 2 mm | -3.25 ± 11.79 | 2.33 ± 26.92 | 0.807 |
| Nasal 2 mm | 1.23 ± 10.84 | 2.73 ± 11.64 | 0.804 |
| Temporal 2 mm | 4.50 ± 11.86 | 5.25 ± 12.27 | 0.961 |
| Superior 3 mm | -22.65 ± 10.75 | -35.03 ± 17.11 | 0.706 |
| Inferior 3 mm | -24.95 ± 17.77 | -26.53 ± 18.26 | 0.963 |
Keratometric values
Keratometric measurements recorded by the two machines are summarized in table 4. The mean difference in anterior radii between the dual and single Scheimpflug systems in steep and flat meridians were -0.05 mm and -0.02 mm, respectively. The mean absolute difference in anterior steep and flat meridian radii between the dual and single Scheimpflug systems was 0.08 ± 0.14 mm and 0.06 ± 0.07 µm, respectively. The mean difference in posterior steep and flat meridian radii between the dual and single Scheimpflug systems was -0.02 mm and -0.06 mm, respectively. The mean absolute difference in the posterior steep and flat meridian radii between the dual and single Scheimpflug systems was 0.08 ± 0.08 mm and 0.11 ± 0.12 µm, respectively. The PCC for central average keratometry was 0.931.
Table 4 Correlation of corneal keratometric measurements between the dual Scheimpflug system (Galilei) and the single Scheimpflug system (Pentacam)
| (µm) | Galilei | Pentacam | Pearson's correlation coefficient |
|---|---|---|---|
| Central average keratometry (D) | 45.14 ± 3.20 | 44.81 ± 3.02 | 0.931 |
| R steep front (mm) | 7.43 ± 0.46 | 7.46 ± 0.44 | 0.979 |
| R flat front (mm) | 7.66 ± 0.42 | 7.68 ± 0.40 | 0.984 |
| R steep back (mm) | 6.02 ± 0.47 | 6.03 ± 0.48 | 0.968 |
| R flat back (mm) | 6.36 ± 0.45 | 6.42 ± 0.40 | 0.946 |
DISCUSSION
Our results demonstrated that both the Galilei Dual Scheimpflug Analyzer and the Pentacam Single Scheimpflug Analyzer display similar values for the same subjects measured in terms of keratometric readings, anterior and posterior elevations, and pachymetry. Both machines gave values comparable with the points lying along the line of equality, with small limits of agreements (Figures 1 and 2). Previous studies have reported good correlations between both machines in either pachymetry or corneal power measurements(6-8).
One of the main diagnostic tools for keratoconus and keratectasia is abnormal topography. Threshold values of topography, beyond which the topography would be labeled as abnormal, are specific for each machine. Problems with the existence of 2 systems will make it more difficult to set common standard cut-off values. In addition, refractive surgery physicians who have access to both systems may be faced with the need to compare serial images of the same patient using 2 different machines. Machine threshold values were first studied on the Orbscan (Bausch and Lomb)(2,9-11) and later on the Pentacam(12,13). With the availability of the Galilei Dual Scheimpflug Analyzer, the primary concern was whether values obtained using the dual Scheimpflug system correlated with those obtained using the single Scheimpflug system and whether images captured by both systems can be safely compared. Our study showed that the 2 systems were strongly correlated in terms of keratometry, anterior and posterior elevation, and pachymetry measurements. Therefore, a conclusion or a trend in values in a specific patient can be generalized from the single Scheimpflug system and applied to the dual Scheimpflug system when considering threshold values and overall patterns. Our results, in terms of pachymetry, were in agreement with those published by Jahadi-Hoseini et al.(6).
The central keratometric, curvature, and pachymetric values showed a high correlation (and high agreement) and were not very different between both systems. As we moved peripherally, the correlation remained high, albeit not as strong as that in the central area. Similarly, other authors have reported an increase in variability in corneal pachymetry measurements from the center to the periphery, particularly in the superior cornea(4,14-17). They attributed this variability to the effects of the superior eyelid(4). We believe that the differences observed in paracentral (peripheral) values were very predictable because small decentration in the BFS would lead to a false high value, considering that the peripheral cornea is farther away from the BFS because of its prolate shape. Even within the same system, small decentrations in BFS can manifest as large deviations in peripheral elevation. The effects of contact lenses on corneal elevation and curvature have been eliminated from the equation because all subjects were advised to stop wearing soft contact lenses for at least 2 weeks(3); furthermore, all subjects that had worn rigid contact lenses in the past 6 months were excluded from the study. The images were obtained on the same day, thus decreasing any additional confounding factors.
Keratometric values in both machines, despite the fact that they were obtained in a different manner, showed a high degree of correlation between both systems; keratometric values with the dual Scheimpflug system were obtained mainly from the Placido image and were only complemented by the rotating Scheimpflug cameras, while keratometry using the single Scheimpflug system relied solely on information from the Scheimpflug images.
The objective of our paper was not to show the advantage of one system over the other, but to assess the degree of correlation. A previously published study showed a difference between the single and dual Scheimpflug systems, with values obtained by the former system (Pentacam) being higher than those obtained by the latter (Galilei)(1). We believe that the difference was primarily due to the different BFS diameters pre-set for each system: 9 mm in the single Scheimpflug system and 8 mm in the dual Scheimpflug system. Current versions of the Pentacam software, similar to the software used in our study, have adopted the 8-mm pre-set BFS diameter. The fact that both machines showed similar results for all indices made it possible to compare the follow-up findings of patients obtained with these two systems, provided the radius of the BFS was set to 8 mm in both machines.
The reason for incorporating two Scheimpflug cameras may solely be patency issues. The strong correlation between measurements obtained by both systems does not preclude the potential advantages offered by the dual Scheimpflug system over the single Scheimpflug system; in theory, the former should be less sensitive to eye movements while obtaining pachymetry measurements. This theoretical advantage could be translated into a clinical one only in a small subset of patients with eye movements beyond a certain critical threshold. Therefore, potential advantages of the dual Scheimpflug system observed in some patients would be easily diluted while evaluating aggregate results. Further studies with the objective of testing the theoretical advantages of the dual Scheimpflug system and comparing them with those of a gold standard system are required.
Our study was limited by the small sample size.
In conclusion, the single and dual Scheimpflug analyzers correlated well in terms of pachymetry, anterior and posterior elevation, and curvature measurements.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

