INTRODUCTION
A cataract is characterized by clouding that develops in the crystalline lens of the eye or its envelope and varies from a slight to a complete opacity that can obstruct the passage of light. Cataracts are specifically defined as any opacification in one or more layers of the crystalline lens that diffracts light and causes impaired vision(1). Cataract is the main cause of curable blindness and represents a public health problem that negatively affects patient quality of life(2,3). The blindness caused by cataract incapacitates the individual, increases dependency, decreases the patient's social condition, and results in early professional retirement(4). Vision recovery facilitated by cataract surgery results in social and economic benefits to the individual, their family, and the community as a whole(5,6).
In the United States, approximately 1.5 million individuals undergo surgery for cataracts every year(7). According to the Brazilian Council of Ophthalmology (CBO), approximately 2% of the Brazilian population aged 60 years is affected by impaired vision due to cataracts(8).
Assessing the quality of life after public health procedures is important. In the field of ophthalmology, maximum emphasis is placed on visual improvement in patients who have undergone cataract surgery using instruments for measuring the quality of life and visual function. Packer et al.(9) described the term visual function as the impact of vision on the quality of life or the capacity to realize everyday activities directly related to visual usefulness(9). Quality of life has different aspects, and because health is not only defined as the lack of disease but also as physical, mental, and social welfare, the term quality of life is considered more often(10,11).
Developed in the United States, the Visual Function 14 (VF-14) questionnaire measures functional capacity related to the vision of patients who have undergone cataract surgery. The VF-14 is based on 14 daily activities that can be affected by ocular diseases. Implantation of an intraocular lens (IOL) is currently one of the most common surgical procedures for cataracts because of the benefits to patients(12,13). The techniques used in cataract surgery are extracapsular cataract extraction (ECEE) and phacoemulsification (PHACO)(14). PHACO is currently the most used technique in the majority of developed countries because of the fast visual recovery and decreased pre- and postsurgical complications(15). The present study aimed to evaluate the quality of life, treatment outcomes, and satisfaction in patients who underwent cataract surgery in Belém, State of Pará, Brazil.
METHODS
The present study is an interventionist study performed at the University Hospital Bettina Franco de Souza (HUBFS). The patients signed a written informed consent form, and the research was approved by the Committee of Ethics and Research with Human Beings of the Núcleo de Medicina Tropical da Universidade Federal do Pará under number 005/2007-CEP/NMT. All the rules of resolution 196/1996 of the National Council of Health were followed. The study was compliant with the Declaration of Helsinki for studies involving humans.
Sixty individuals with senile cataract indicated for surgery and attended to at the Ophthalmology Service of the HUBFS were selected. The patients were divided into 2 groups; 30 underwent ECEE and 30 underwent PHACO. All surgeries were performed by the same surgeon.
Patients completed the VF-14 in the waiting room of the Ophthalmology ambulatory clinic of the HUBFS or in one of the patient assistance offices. A similar questionnaire was administered to patients in a population study of corneal transplantation in Brazil(16). The VF-14 comprises 14 questions, each of which can have 5 answers (0 = impossible to realize, 1 = intense difficulty, 2 = moderate difficulty, 3 = minimal difficulty, 4 = without difficulty). The corresponding number is multiplied by 25 to obtain the final score, which varies from 0 (worst index of visual function) to 100 (best index of visual function)(17).
To characterize the sample, the following variables were selected: sex, age, schooling, occupation, and visual acuity. Quality of life variables included physical domains (near vision and far vision) and the level of independence (daily activities, social activities, physical activities, and capacity to drive an automobile). Visual acuity is presented as logMAR (Snellen equivalent). The results of the questionnaire before and after surgery were compared, taking into consideration evident improvements in the ability to perform daily tasks after surgery as reported by the patients, using ANOVA and the sign test.
RESULTS
The average age of the study population was 68 ± 8.4 years (mean ± standard deviation) in the PHACO group and 67 ± 8.0 years in the ECEE group. With regard to schooling, 16 patients (53.3%) in the PHACO group had completed primary and secondary school, 8 (26.7%) had completed high school, 4 (13.3%) had a college degree, and 2 (6.7%) had no school background. In the ECEE group, 24 patients (80%) had completed primary and secondary school, 3 (10%) had received high school level education, and 3 (10%) had no schooling background.
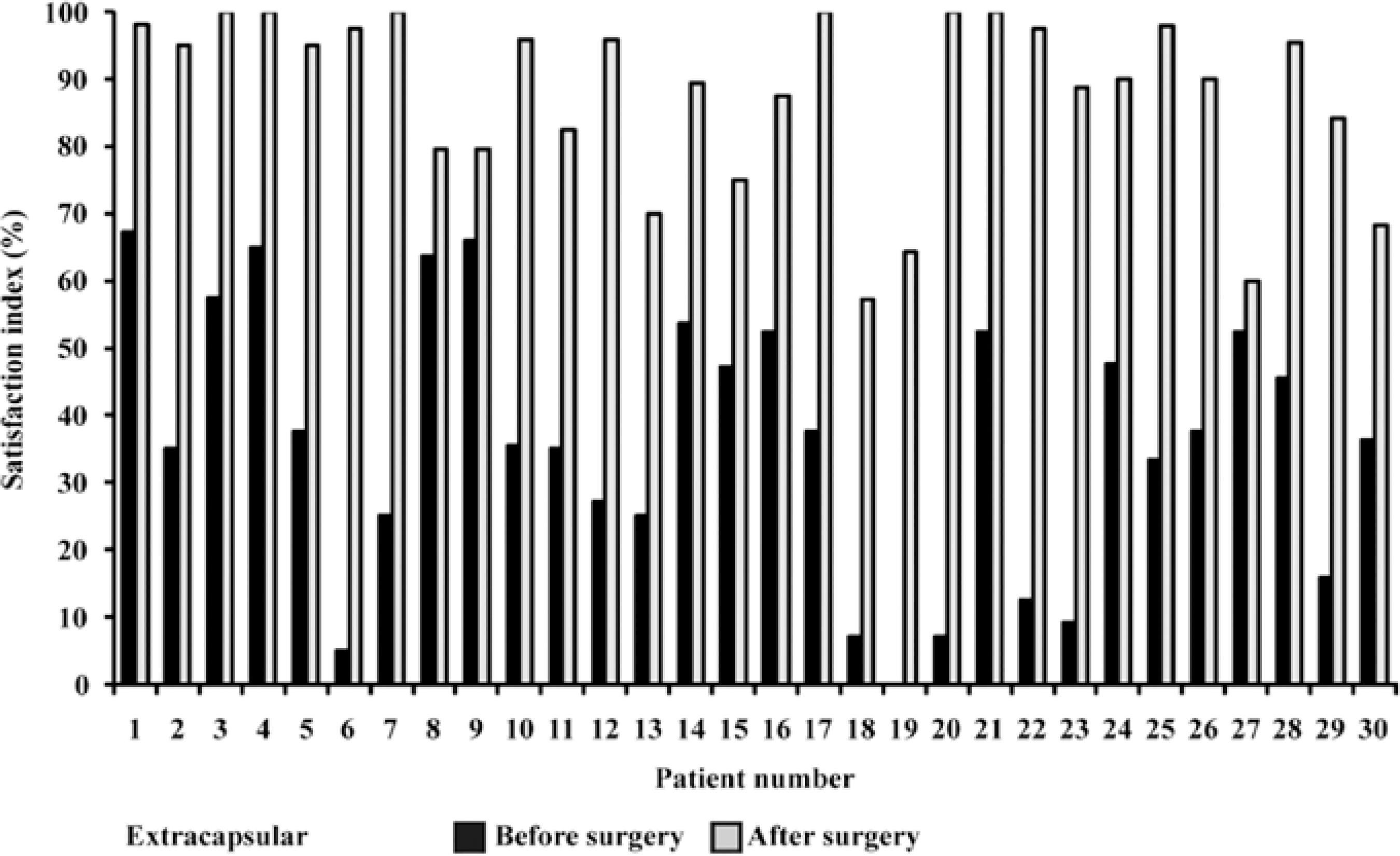
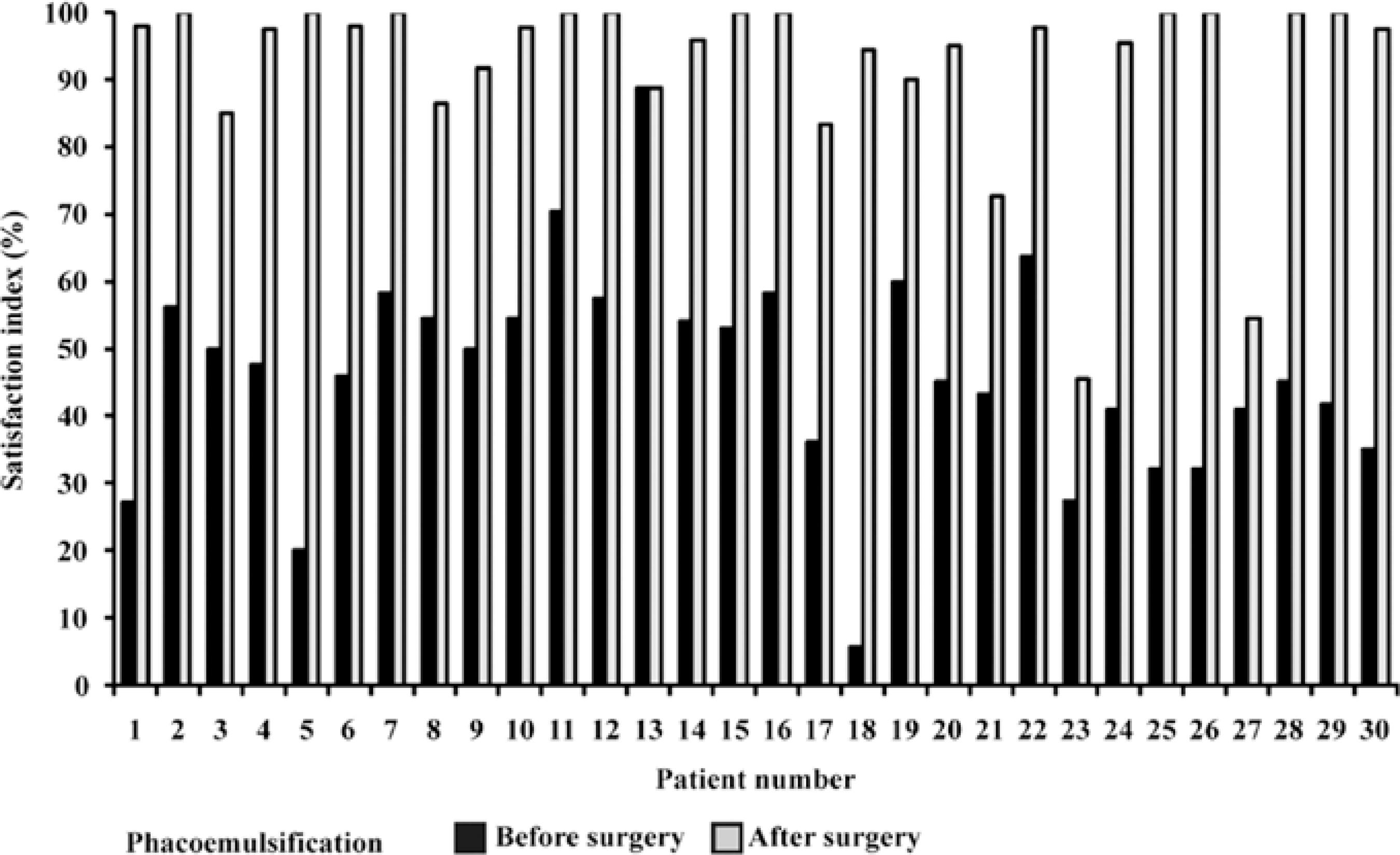
With regard to occupation, 7 patients (23.3%) in the ECEE group worked in rural areas and 7 (23.3%) patients were maids. In the PHACO group, 8 patients (26.7%) were maids and 6 patients (20%) were retired. The average VF-14 score was 47.0 before and 94.1 after PHACO, while it was 38.0 before and 89.4 after ECEE. Significant differences were found between the averages calculated before and after surgery in both groups (Figures 1 and 2).
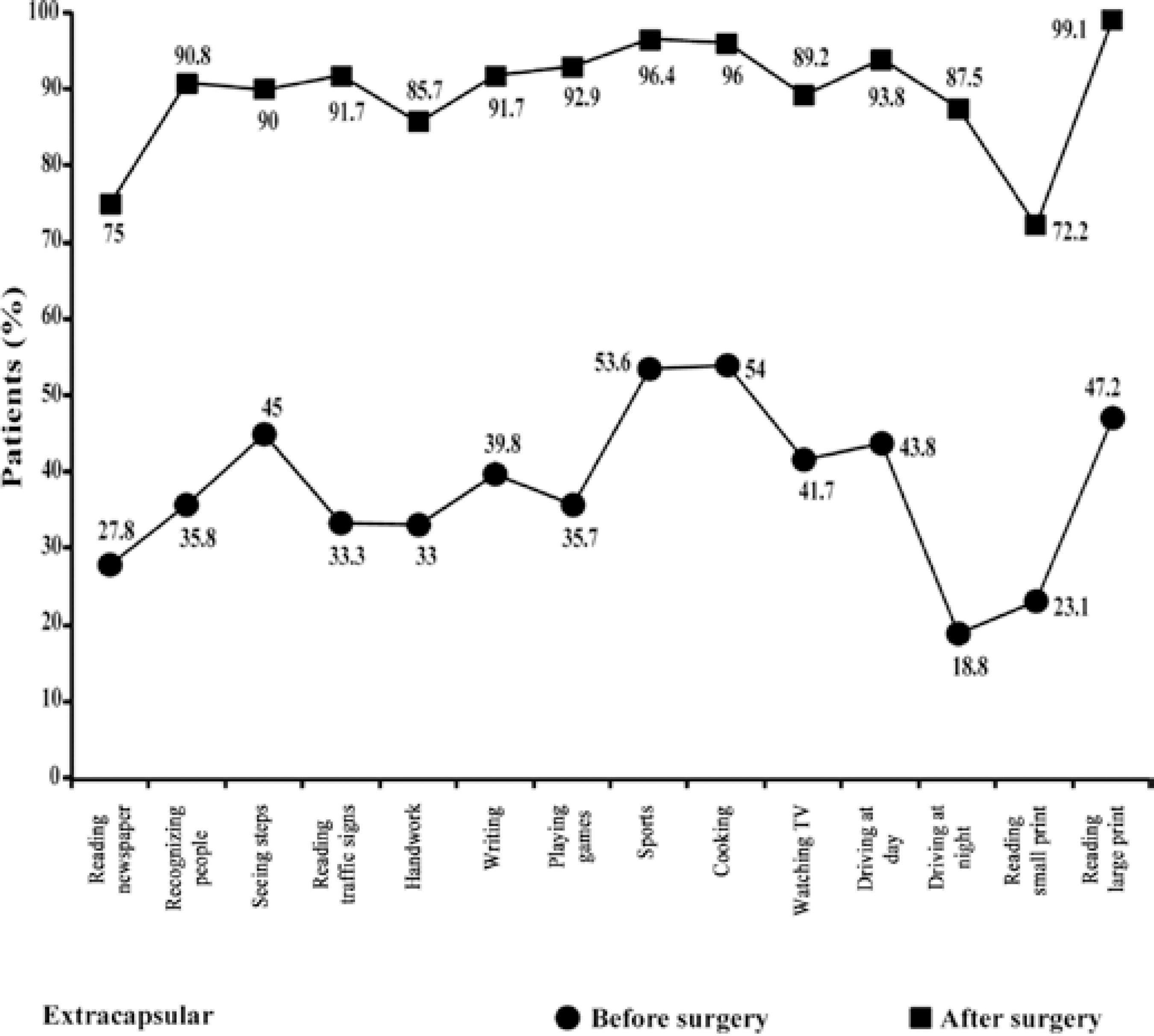
Figure 1 Average VF-14 score per question before and after surgery among patients who underwent extracapsular cataract extraction.
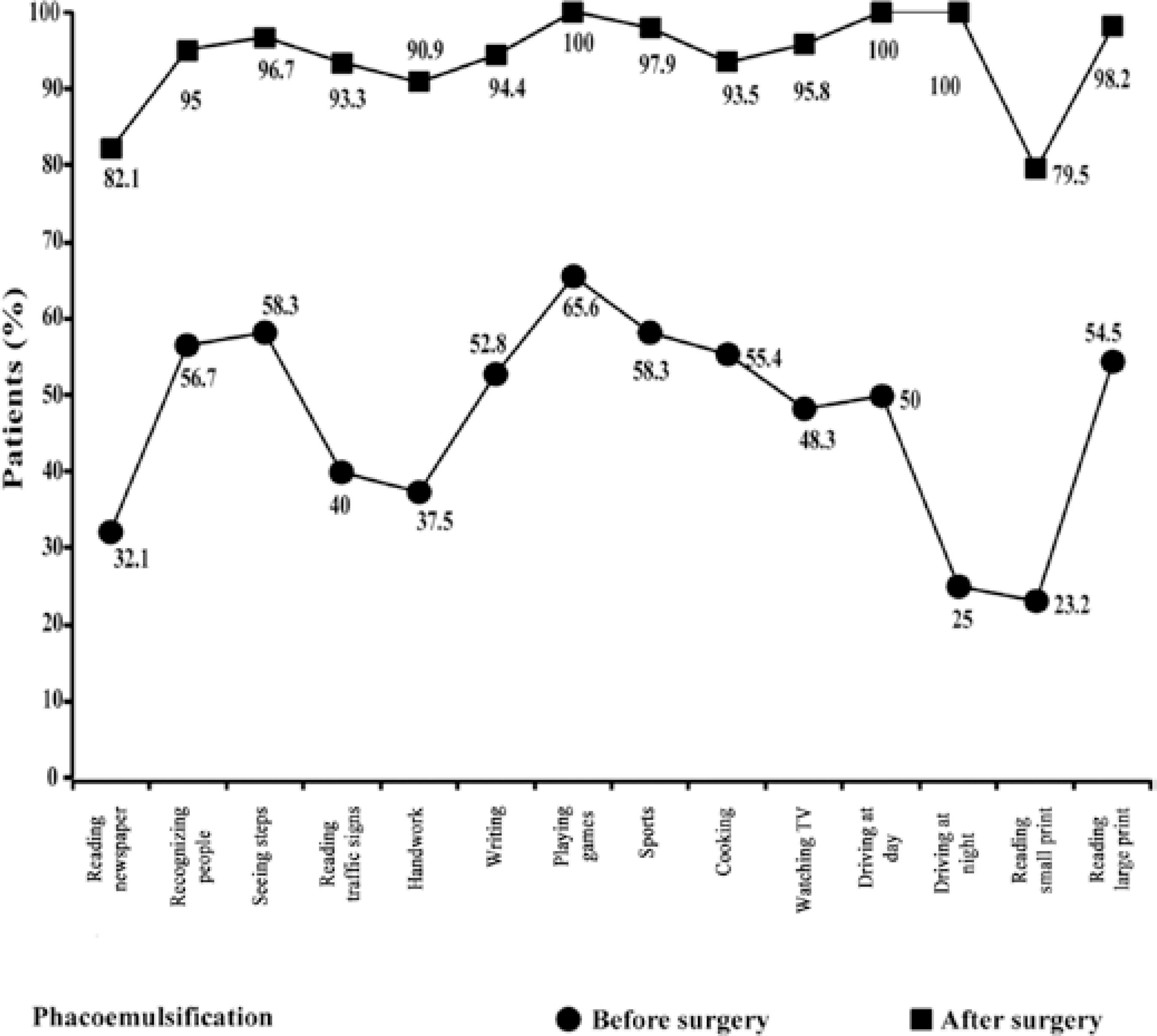
Figure 2 Average VF-14 score per question before and after surgery among patients who underwent phacoemulsification.
The visual acuity before surgery was considerably low, mainly in patients who underwent ECEE, 30% of whom had an visual acuity of 1.2 logMAR (20/400). The acuities of patients in the PHACO group varied greatly before surgery, with a predominant acuity of 0.6 (20/80) in 26.7% patients. After surgery, an improvement was observed in 83.3% patients, with an acuity of >0.3 logMAR (20/40). A number of ECEE patients had a visual acuity of 0.0 logMAR (20/20), corresponding to 43.3% of the total sample (Table 1).
Table 1 Patient visual acuity before and after cataract surgery according to surgical procedure
| Visual acuity | Phacoemulsification | Extracapsular extraction | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Snellen | logMAR | (n) | % | (n) | % | ||||
| Before surgery | <20/400 | >1.3 | 5 | 16.7 | 9 | 30.0 | |||
| 20/400 | 1.3 | 3 | 10.0 | 7 | 23.3 | ||||
| 20/200 | 1.0 | 6 | 20.0 | 4 | 13.3 | ||||
| 20/125 | 0.8 | 1 | 3.3 | 0 | 0 | ||||
| 20/100 | 0.7 | 7 | 23.3 | 8 | 26.7 | ||||
| 20/80 | 0.6 | 8 | 26.7 | 2 | 6.7 | ||||
| Total | 30 | 100 | 30 | 100 | |||||
| After surgery | 20/20 | 0 | 9 | 30.0 | 13 | 43.3 | |||
| 20/25 | 0.10 | 6 | 20.0 | 2 | 6.7 | ||||
| 20/30 | 0.20 | 7 | 23.3 | 2 | 6.7 | ||||
| 20/40 | 0.30 | 3 | 10.0 | 5 | 16.7 | ||||
| 20/50 | 0.40 | 0 | 0 | 2 | 6.7 | ||||
| 20/60 | 0.50 | 3 | 10.0 | 1 | 3.3 | ||||
| 20/70 | 0.55 | 0 | 0 | 2 | 6.7 | ||||
| 20/100 | 0.70 | 2 | 6.7 | 3 | 10.0 | ||||
| Total | 30 | 100 | 30 | 100 | |||||
With regard to satisfaction, graphic analysis using the sign test (Figures 3 and 4) and ANOVA revealed significant satisfaction in both surgical groups (p<0.0001), which resulted in an improved quality of life (Figures 5 and 6).
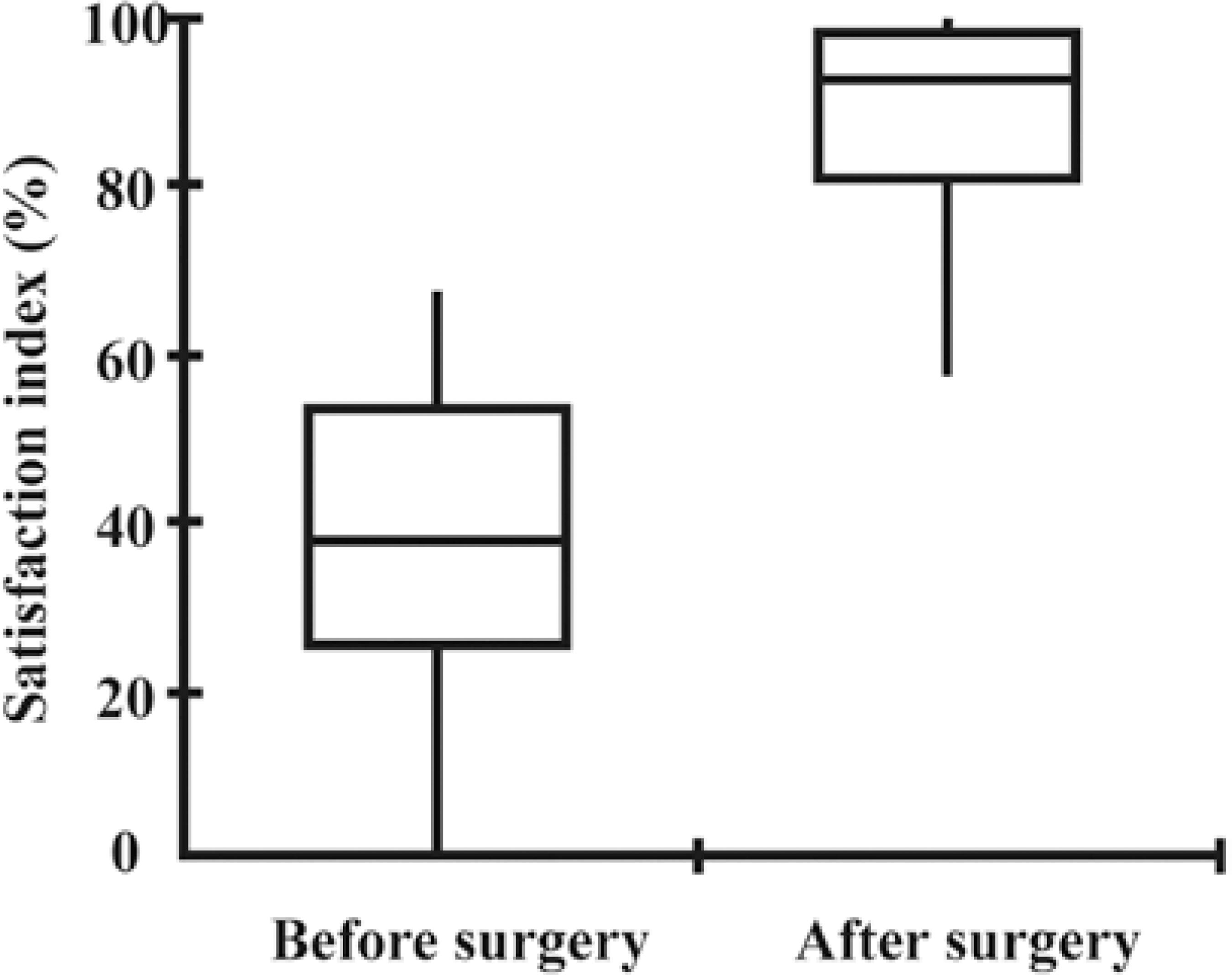
Figure 3 Satisfaction analysis using the sign test among patients who underwent extracapsular cataract extraction. Horizontal bars represent the median, first, and third quartiles. Vertical bars represent the standard deviation from the mean.
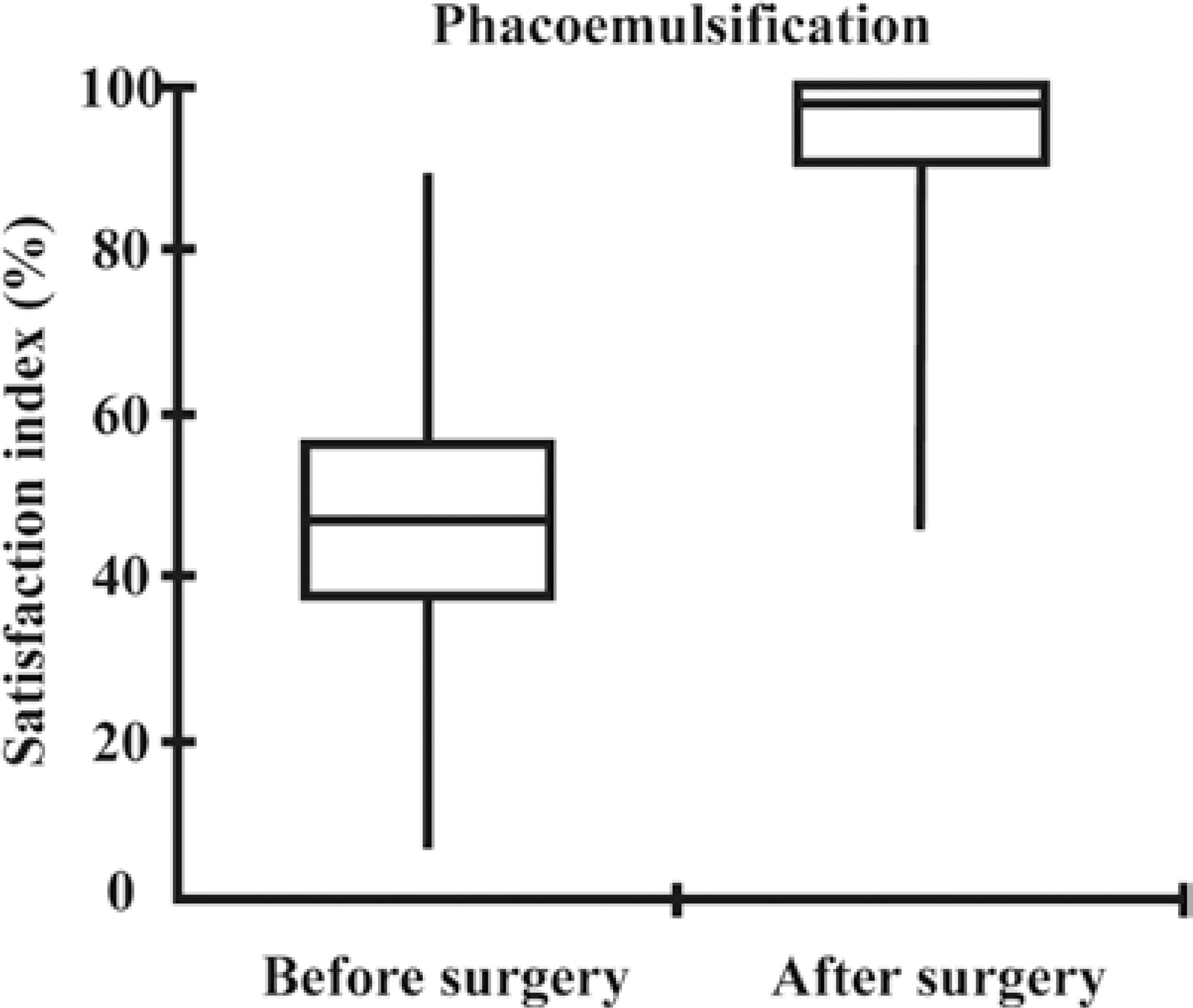
Figure 4 Satisfaction analysis among patients who underwent phacoemulsification. Horizontal bars represent the median, first, and third quartiles. Vertical bars represent the standard deviation from the mean.
DISCUSSION
In a study by McKee et al.(18), the average patient age was 75 years for men and 77 years for women. In the present study, the proportion of patients aged 61-70 years was high at 36.7% and 43.3% in the PHACO and ECEE groups, respectively, probably because patients visit ophthalmological centers earlier because of the lack of visual function or increased awareness about cataracts and their surgical treatment.
With regard to patient occupations, we found no data in the literature. However, although the majority of patients were elderly, 77% were still working, increasing the importance of vision recovery for the continuity of professional activities. The high proportion of working patients reflects the reality of the studied population that, despite being of retirement age, still needed to work to make a living.
Twenty-two (37%) of the 60 patients presented with a postsurgical visual acuity of 0.0 (20/20), indicating a total recovery of visual acuity. Nevertheless, 27% patients (n = 16) had a visual acuity of <0.7 (20/100). Norregaard et al. considered 0.3 to be the optimal visual acuity after surgery(19). We can conclude that a significant proportion of patients did not achieve the desired acuity. However, on the basis of the results obtained in the visual function test, even though the visual acuity of some patients remained low, surgery clearly enabled them to perform daily activities. Therefore, the association of both methods, objective and subjective, is important to the final evaluation of surgical outcomes.
After surgery, considerable improvement was observed in the ability to perform all activities, with an improvement of approximately 40 points for each activity. Some activities such as reading the newspaper and reading small print still remained below the 95 points set by Norregaard et al.(19), even with the significant improvement in outcome. In that previous study, a VF-14 score of 95 was used as an indicator of success or optimum visual function after surgery.
The results obtained before and after surgery are of great importance in complementing the current literature. In the study by Friedman et al.(20), approximately 50% patients interviewed before surgery reported difficulty or inability to drive at night or read small print, consistent with the major difficulties reported by patients in the present study.
Friedman et al. disagreed with some questions included in the VF-14 that inform little about the functional status of most patients(20). For example, 4 out of 5 patients did not practice sports, indicating that this issue did not contribute to the VF-14 score. A similar situation was observed in the current study, not only with practicing sports but also with car driving and playing games such as dominoes and cards. Therefore, the test should be adapted to activities related to the culture of each region, with an increased focus on the elderly.
In general, the average VF-14 score among patients who underwent PHACO was 47 points before and 94.1 points after surgery, indicating an improvement of 47.1 points. In the ECEE group, the average VF-14 score was 38 points before and 89.4 points after surgery, indicating an improvement of 51.4 points. These results are similar to those of other studies in which the average VF-14 score was 82.6 before and 94.8 after surgery(18).
The results after surgery were like other results observed around the world. Several conclusions concerning patients who used the service in the city of Belém can be made. First, patients who visited the service usually had poor visual function; the difficulties these patients faced in everyday life were so grave that they preferred surgical correction. In developed countries, patients with an average of more than 70 points before surgery usually do not exhibit an obvious improvement after surgery, which directly influences patient satisfaction with the surgical outcome.
The visual acuity of patients demonstrated a good improvement after surgery. Reading the newspaper, performing manual tasks, reading at night, and reading texts with small letters were the daily activities that most often impaired the existence of the cataract. Activities such as playing games (cards, dominoes, etc.), practicing sports, and driving were associated with low scores in the satisfaction and quality of life analysis of patients; 75% patients did not play games, 68% did not practice sports, and 87% did not drive. However, after surgery, a considerable improvement was observed in the ability to perform all these activities.
The observed improvement in the quality of life was significant (p<0.0001) and directly related to patient satisfaction with surgical outcomes, which was also significant (p<0.0001), as assesse using the VF-14. Satisfaction and quality of life are individual factors; consequently, patient responses to questions regarding improvements in the ability to perform each activity are subjective and depend uniquely on individual perception.
CONCLUSIONS
What is known
Developed in the United States, the VF-14 questionnaire measures functional capacity related to the vision of patients who have undergone cataract surgery. The VF-14 is based on 14 daily activities that can be affected by ocular diseases. Implantation of an IOL is currently one of the most common surgical procedures for cataract because of the benefits to patients. The techniques used in cataract surgery are ECEE and PHACO, the latter being the most used technique in the majority of developed countries because of the fast visual recovery and decreased pre- and postsurgical complications. The VF-14 has been widely used, particularly in advanced countries, and has validated the use of both ECEE and PHACO; however, it determines that PHACO results in the best outcome in terms of patient quality of life. No other study has evaluated the outcomes of ECEE and PHACO in cataract patients living in remote areas such as the Amazon region.
What this paper adds
The VF-14 was used, for the first time as per our knowledge, to evaluate patients in the Amazon Region and validated the use of both ECEE and PHACO as surgical procedures that considerably improve the quality of life of patients after surgery. The observed improvement in quality of life was significant and directly related to patient satisfaction with surgical outcomes, which was also significant, as assessed using the VF-14. Satisfaction and quality of life are individual factors; consequently, patient responses to questions about improvements in the ability to perform each activity are subjective and depend uniquely on individual perception.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

