

Lígia Issa de Fendi1; Gustavo Viani Arruda1; Vital Paulino Costa3; Jayter Silva Paula1
DOI: 10.1590/S0004-27492011000400016
ABSTRACT
PURPOSE: To conduct a systematic review with meta-analysis on the efficacy of trabeculectomy (TREC) followed by beta irradiation (BRT/TREC) compared to TREC alone for glaucoma in terms of intraocular pressure (IOP) control and adverse effects of treatment in different ethnic groups. METHODS: A meta-analysis of randomized controlled trials (RCT) was performed comparing adjunct BRT treatment for glaucoma with standard TREC after 12 months. The MEDLINE, EMBASE, LILACS, and Cochrane Library databases, Trial registers, bibliographic databases and recent studies of relevant journals were searched. Two reviewers independently reviewed relevant reports and the references from these reports were searched for additional trials, using guidelines set by QUOROM statement criteria. RESULTS: Of a total of 1,350 citations, eight studies (five cohorts, three randomized) were identified and only 3 RCT were included in this meta-analysis. Higher IOP reductions were verified in the BRT arm compared to the control arm (mean difference=1.68 mmHg, 95% CI= 0.61-2.68, P=0.002). Uncontrolled postoperative IOP (>21 mmHg) was less frequent when BRT was used (BRT/ TREC arm) compared to the control arm (38/218=17.4% versus 9/239=3.8%; OR=6.7; 95% CI 3.2-14.3, P<0.0001). Although better IOP control was observed in all patients treated with adjuvant BRT, only Black patients displayed a significant difference (P=0.005). There were no significant differences between the BRT and control arms regarding loss of visual acuity, postoperative complications and necessity of cataract surgery. CONCLUSION: Adjunct BRT increases the success rate of TREC, with better results in non Caucasian patients, and does not influence the occurrence of postoperative complications.
Keywords: Glaucoma; Glaucoma; Glaucoma; Trabeculectomy; Eye; Beta particles; Meta-analysis
RESUMO
OBJETIVO: Realizar uma revisão sistemática com meta-análise sobre a eficácia da trabeculectomia (TREC), seguida ou não por irradiação beta (BRT/TREC) para o tratamento do glaucoma, em termos de controle da pressão intraocular (PIO) e de efeitos adversos, em diferentes grupos étnicos. MÉTODOS: Uma meta-análise de ensaios clínicos randomizados (RCT) foi realizada, comparando os resultados de 12 meses da TREC com o uso adjuvante de BRT, com aqueles da TREC padrão. Foram fontes de pesquisa as bases de dados MEDLINE, EMBASE, LILACS, Cochrane, além de sítios de registro de ensaios clínicos, estudos recentes em revistas da área e outras bases de dados bibliográficos. Dois revisores avaliaram independentemente publicações relevantes e as referências desses trabalhos foram pesquisadas para procura de ensaios adicionais, de acordo com as diretrizes estabelecidas pelos critérios do QUOROM. RESULTADOS: De um total de 1.350 citações, oito estudos (cinco coortes e três aleatorizados) foram identificados e apenas 3 RCT foram incluídos nesta meta-análise. Maiores reduções na PIO foram verificadas no braço de estudo da BRT, comparado com o braço controle (diferença média=1,68 mmHg, 95% CI= 0,61-2,68, P=0,002). A frequência de PIO pós-operatória não controlada (>21 mmHg) foi menor quando utilizada a BRT (BRT/TREC) em relação ao grupo controle (38/218 =17,4% versus 9/239 =3,8%; OR= 6,7 IC 95% 3,2 14,3, P<0,0001). Apesar do melhor controle da PIO ter sido observada em todos os pacientes do braço BRT, apenas os pacientes negros apresentaram uma diferença significativa (P=0,005). Não houve diferenças significativas entre os braços BRT e controle, em termos de perda da acuidade visual, complicações pós-operatórias e necessidade de cirurgia de catarata. CONCLUSÃO: O uso de BRT adjuvante aumenta a taxa de sucesso da TREC, com melhores resultados em pacientes não-caucasianos, não influenciando a ocorrência de complicações pós-operatórias.
Descritores: Glaucoma; Glaucoma; Trabeculectomia; Olho; Partículas beta; Metanálise
REVIEW ARTICLE ARTIGO DE REVISÃO
Meta-analysis of beta radiation augmentation for trabeculectomy - results in distinct ethnic groups
Meta-análise da trabeculectomia potencializada pela radiação beta - resultados em grupos étnicos distintos
Lígia Issa de FendiI; Gustavo Viani ArrudaI,II; Vital Paulino CostaIII; Jayter Silva PaulaIV
IPhysician, Department of Ophthalmology, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo - USP - São Paulo (SP), Brazil
IIPhysician, Department of Radiotherapy, Faculdade de Medicina de Marília - São Paulo (SP), Brazil
IIIProfessor, Department of Ophthalmology, Faculdade de Ciências Médicas, Universidade Estadual de Campinas - UNICAMP - Campinas (SP), Brazil
IVProfessor, Department of Ophthalmology, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo - USP - São Paulo (SP), Brazil
ABSTRACT
PURPOSE: To conduct a systematic review with meta-analysis on the efficacy of trabeculectomy (TREC) followed by beta irradiation (BRT/TREC) compared to TREC alone for glaucoma in terms of intraocular pressure (IOP) control and adverse effects of treatment in different ethnic groups.
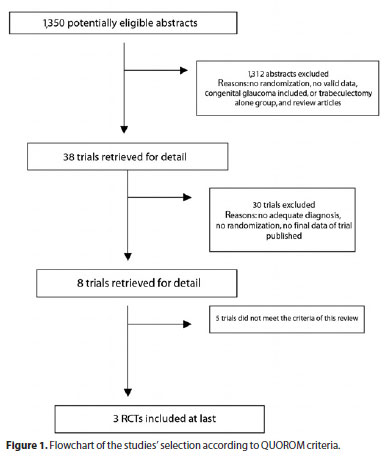
METHODS: A meta-analysis of randomized controlled trials (RCT) was performed comparing adjunct BRT treatment for glaucoma with standard TREC after 12 months. The MEDLINE, EMBASE, LILACS, and Cochrane Library databases, Trial registers, bibliographic databases and recent studies of relevant journals were searched. Two reviewers independently reviewed relevant reports and the references from these reports were searched for additional trials, using guidelines set by QUOROM statement criteria.
RESULTS: Of a total of 1,350 citations, eight studies (five cohorts, three randomized) were identified and only 3 RCT were included in this meta-analysis. Higher IOP reductions were verified in the BRT arm compared to the control arm (mean difference=1.68 mmHg, 95% CI= 0.61-2.68, P=0.002). Uncontrolled postoperative IOP (>21 mmHg) was less frequent when BRT was used (BRT/ TREC arm) compared to the control arm (38/218=17.4% versus 9/239=3.8%; OR=6.7; 95% CI 3.2-14.3, P<0.0001). Although better IOP control was observed in all patients treated with adjuvant BRT, only Black patients displayed a significant difference (P=0.005). There were no significant differences between the BRT and control arms regarding loss of visual acuity, postoperative complications and necessity of cataract surgery.
CONCLUSION: Adjunct BRT increases the success rate of TREC, with better results in non Caucasian patients, and does not influence the occurrence of postoperative complications.
Keywords: Glaucoma/radiation effects; Glaucoma/surgery; Glaucoma/radiotherapy; Trabeculectomy; Eye/radiation effects; Beta particles; Meta-analysis
RESUMO
OBJETIVO: Realizar uma revisão sistemática com meta-análise sobre a eficácia da trabeculectomia (TREC), seguida ou não por irradiação beta (BRT/TREC) para o tratamento do glaucoma, em termos de controle da pressão intraocular (PIO) e de efeitos adversos, em diferentes grupos étnicos.
MÉTODOS: Uma meta-análise de ensaios clínicos randomizados (RCT) foi realizada, comparando os resultados de 12 meses da TREC com o uso adjuvante de BRT, com aqueles da TREC padrão. Foram fontes de pesquisa as bases de dados MEDLINE, EMBASE, LILACS, Cochrane, além de sítios de registro de ensaios clínicos, estudos recentes em revistas da área e outras bases de dados bibliográficos. Dois revisores avaliaram independentemente publicações relevantes e as referências desses trabalhos foram pesquisadas para procura de ensaios adicionais, de acordo com as diretrizes estabelecidas pelos critérios do QUOROM.
RESULTADOS: De um total de 1.350 citações, oito estudos (cinco coortes e três aleatorizados) foram identificados e apenas 3 RCT foram incluídos nesta meta-análise. Maiores reduções na PIO foram verificadas no braço de estudo da BRT, comparado com o braço controle (diferença média=1,68 mmHg, 95% CI= 0,61-2,68, P=0,002). A frequência de PIO pós-operatória não controlada (>21 mmHg) foi menor quando utilizada a BRT (BRT/TREC) em relação ao grupo controle (38/218 =17,4% versus 9/239 =3,8%; OR= 6,7 IC 95% 3,2 14,3, P<0,0001). Apesar do melhor controle da PIO ter sido observada em todos os pacientes do braço BRT, apenas os pacientes negros apresentaram uma diferença significativa (P=0,005). Não houve diferenças significativas entre os braços BRT e controle, em termos de perda da acuidade visual, complicações pós-operatórias e necessidade de cirurgia de catarata.
CONCLUSÃO: O uso de BRT adjuvante aumenta a taxa de sucesso da TREC, com melhores resultados em pacientes não-caucasianos, não influenciando a ocorrência de complicações pós-operatórias.
Descritores: Glaucoma/cirurgia; Glaucoma/radioterapia; Trabeculectomia; Olho/efeitos de radiação; Partículas beta; Metanálise
INTRODUCTION
Glaucoma is the world's most common blinding condition causing irreversible visual loss(1). Strong evidence suggests that lowering intraocular pressure (IOP) is beneficial in reducing the development and progression of the disease(2,3). Trabeculectomy (TREC) is the surgical procedure of choice to reduce IOP in patients with glaucoma. However, TREC is not 100% successful in maintaining adequate IOP control. A major cause of surgical failure is related to fibroblast proliferation and scarring of the conjunctival bleb(4-6). In patients at high risk for failure, adjuvant therapy aiming to inhibit wound healing has been used. 5-fluorouracil (5-FU) or mitomycin C (MMC) have been shown to be effective in increasing TREC success rate(7-13), however they have been associated with postoperative complications, such as corneal epithelial defects, wound leak, ischemic bleb, hypotony, blebitis, and endophthalmitis(4,5).
Beta radiation (BRT) is a particulate radiation consisting of high-speed electrons, which are rapidly attenuated by biological tissues. This makes it very useful for superficial radiation treatments where deep tissue penetration is undesirable. Strontium-90 (90Sr), an unstable fission product of uranium-235 (235U), has been found to be a clinically useful source of beta radiation with a long half-life
(28.7 years), and emits only high-energy beta particles as it decays. Among the emitters employed in ophthalmology, the 90Sr source has the most marked attenuation in biological tissues, making it particularly suitable for treatment of the ocular surface.
It has also been used as an auxiliary measure in some ocular procedures, including in pterygium and in age-related macular degeneration(6-11). BRT inhibits the proliferation of fibroblasts from the Tenon's capsule and the conjunctiva, both in vitro and in animal models(5). The effectiveness and safety of adjunct BRT in glaucoma surgery has not been adequately investigated because of small sample size, variable radiation doses and mixed patient groups(6,14-20). Recently a meta-analysis on this issue was published(21), however in this study the authors did not evaluate the differences on IOP reduction among races, adverse effects as hypotony, hyphema, bleb leak and choroidal effusion. So, we decided to perform a systematic review and metaanalysis in order to analyze the efficacy and safety of TREC followed by beta irradiation (BRT/TREC) compared to TREC alone, including potential differences between distinct ethnic groups.
METHODS
Criteria for considering studies for this systematic review were:
1. TYPES OF STUDIES
All randomized and quasi-randomized controlled trials were eligible for inclusion.
2. TYPES OF PARTICIPANTS
Eligibility criteria were: adults with age of 40 years or more, characteristic glaucomatous changes in the optic disc, IOP >21 mmHg and open angle on gonioscopy. Trials with participants under 18 years old were not included. There were no restrictions regarding gender or ethnicity.
3. TYPES OF INTERVENTION
All trials were included when TREC (without adjuvants) was compared to BRT/TREC. All beta radiation emitters contained strontium-90/yttrium-90b (strontium-90 decays to yttrium-90 on release of the beta particle) in 8 mm disc applicator.
4. TYPES OF OUTCOME MEASURES
Main outcomes
The primary outcome measurement was surgical failure within 12 months, defined as IOP > 21 mmHg with antiglaucoma medications. Secondary outcomes were visual acuity, mean IOP reduction, surgical reintervention for cataract, and intraoperative and postoperative complications.
SEARCH STRATEGY FOR STUDIES IDENTIFICATION
The databases on MEDLINE (Ovid) (1996 to May 2007), BIOSIS (1985 to July 2007) and CINAHL (1982 to August 2007), SIGLE, ZETOC, NRR and http://www.controlled-trials.com were all searched in February 2008 and revised in January 2011, using the terms: "glaucoma" (Medical Subject Heading [MeSH]), "trabeculectomy" (text word), "postoperative beta irradiation" (text words), "surgery drainage" (text words) and "adjuvant radiotherapy" (MeSH and text words). These terms were then combined with the search terms for the following study designs: practice guidelines, systematic reviews or meta-analyses, reviews, randomized controlled trials and controlled clinical trials. References of all retrieved studies and reviews were searched for additional trials. Manual searches in ophthalmology, journals or conference proceedings were not undertaken. We did not contact pharmaceutical companies or manufacturers of ophthalmic lasers and surgical equipment.
Two authors independently viewed the titles and abstracts of all the studies identified in the electronic searches. All methodological steps followed the guidelines set by QUOROM statement criteria(22). The full copies of all possibly or definitely relevant studies were obtained and independently inspected by two authors to determine whether they met the inclusion criteria. When a difference in opinion occurred, a third reviewer was consulted, as an arbiter. The authors of the selected studies could be contacted to elucidate any doubts, when necessary.
DATA ANALYSIS
Studies were examined as to whether the unit of randomization was eyes or people. In all three included studies, the unit of randomization was one eye per patient. Whenever possible, data were extracted on the basis of an intention to treat analysis. Outcomes were analyzed, when possible, in a stratified manner according to short, medium and long-term outcome assessment. One author entered the data into comprehensive meta-analysis and a second author re-entered the data using the double-entry facility to check errors and inconsistencies. IOP was analyzed as a continuous variable. For each study, the mean IOP change from baseline, including the standard deviation (SD) of change for each intervention group, was calculated when possible. If the SD of change was not reported, it was calculated assuming a correlation of 0.5 between the baseline and end-point IOPs(23). When visual field and visual acuity outcomes were reported as mean scores, data were analyzed as mean score change from baseline and the SD of change. Visual field progression and visual acuity were analyzed when possible as categorical variables. If reported as a score, the data were analyzed as continuous variables. If summary effect measures were reported, the logarithm of the odds ratio (Ln OR) and the standard error (SE) were entered into comprehensive meta-analysis as generic inverse variance measures. When other studies presented similar outcomes using proportions, the OR and the 95% confidence interval (95% CI) were calculated. All meta-analyses were assessed for heterogeneity as a preliminary test. A random-effects model was used if the test of heterogeneity was significant (P<0.05), otherwise a fixed-effects model was used. An OR with a P value < 0.05 was considered statistically significant. Publication bias was assessed with the Begg funnel plot and Egger weighted regression for funnel plot asymmetry. Publication bias was considered significant if the Egger test was significant (P<0.05) and the Begg plot suggested bias(24-26). Our statistical analysis was performed with comprehensive metaanalysis software (Comprehensive Meta-analysis Version 2; Biostat, Inc. Englewood NJ, 2005).
RESULTS
The electronic and manual searches retrieved 1,350 citations. All citations were screened and 38 full text articles were retrieved for further assessment. Reasons to withdraw the unselected studies included: no randomization, no valid data, absent of control group, review works, etc. Five studies were excluded(18-20), since they were either not randomized, controlled or were comparisons of medical versus surgical treatment. The reasons for exclusion are detailed in the figure 1. Three randomized trials met the criteria for inclusion(15-17). No newer study could be considered during the last search performed in January 2011. A summary of the characteristics of the included studies is displayed in table 1.
SETTING AND PARTICIPANTS
The three selected studies(15-17) included trials with a total of 457 randomized participants. All participants had newly diagnosed open-angle glaucoma with no prior surgical treatment.
MAIN OUTCOMES
The primary outcome measure in all the trials was the rate of failure to maintain the IOP < 21 mmHg at 12 months. Two trials assessed change in visual acuity during the follow-up. Cataract surgery was reported in two trials(16,17) and additional glaucoma surgery, as a consequence of failure, was reported by all studies. Adverse events were observed in the intervention group in all trials. As the description of these adverse effects was different in each trial, we analyzed each complication separately (Table 2).
SURGICAL FAILURE
The three studies reported IOP maintained < 21 mmHg at 12 months follow-up as one of the outcomes. Surgical failure rates were lower for the BRT/TREC arm (9/239 = 3.8%) compared to control arms (38/218 =17.4%). The individual odds ratios ranged from 2.97 to 9.29, with a pooled odds ratio for all of the trials of 6.7 with a 95% CI of 3.2 to 14.3 (Figure 2). Since the heterogeneity test showed no statistical significance (P=0.47), the pooling of the data was considered valid. Ethnic subgroups analysis displayed a tendency towards less surgical failure, but not significantly, in the BRT/TREC arm comparing to control arm, in Caucasian patients (P=0.055) (Figure 3).
IOP REDUCTION
At 12 months, the BRT/TREC group was associated with significantly greater IOP reduction than TREC alone (difference in the IOP reduction from baseline of 1.65 between groups, 95% CI: 0.61 2.68), as demonstrated in figure 4. The subgroups' analysis according to ethnic group revealed that the IOP reduction was greater in Black patients than Caucasian patients in BRT/TREC arm. Black patients showed significant mean difference in the IOP from baseline (2.0 mmHg; 95% CI: 0.6 - 3.3, p=0.005), while Caucasian patients presented no significant mean difference (1.2 mmHg; 95% CI: 0.32 2.8, P=0.120) (Figure 5).
POSTOPERATIVE COMPLICATIONS
All three studies reported postoperative adverse events as one of the outcomes. No complication was described repeatedly in all of these studies. Thus, each complication was analyzed when described in more than one study. Endophthalmitis, uveitis and suprachoroidal hemorrhage were reported in only one of these studies (Table 2). No significant difference in the proportion of each complication was observed between BRT/TREC arm and control arm: hyphema (p=0.835), hypotony (P=0.541), shallow anterior chamber (P=0.726), bleb leak (P=0.485) and choroidal effusion (P=0.473).
There was no significant difference in visual acuity reduction (OR=0.84, 95% CI: 0.5 - 1.3, P=0.43) between the two arms. Moreover, no decrease in visual acuity was observed in either group during the study period.
The BRT/TREC group experienced a higher incidence of cataract considering the need for extraction than did the TREC group (25/195 - 12.8% versus 9/190 - 4.7% participants), however this difference was not statistically significant (OR=1.85, 95% CI: 0.82 - 4.16, P=0.13).
DISCUSSION
The use of BRT in glaucoma surgery has been investigated by several authors(6,14-20) but all reports included small numbers of patients, and the irradiation tended to be used in mixed groups of patients with poor prognosis. There are no convincing data from these studies indicating that BRT improves the IOP control posttrabeculectomy, which explains why this technique has not gained popularity.
In our study, combining the results of three randomized trials (457 patients), we were able to demonstrate a significant positive adjunctive effect of BRT in eyes undergoing TREC. The mean difference between the IOP reduction from baseline obtained in BRT-treated eyes and the control group at one year follow-up was 1.64 mmHg (P=0.002).
We did not find any significant difference in the analysis of each complication regarding radiotherapy adjunctive treatment. However, the radiation group experienced a higher incidence of cataract requiring extraction than did the control group (12.8% versus 4.7% respectively; P=0.13). We are not aware if this difference would be significant with an increment of sample size.
The calculated amount of radiation reaching the germinal epithelium of lenses in all trials was probably less than the minimum dosage reported to cause cataract (200 cGy)(27,28). Radiation-induced cataract has a characteristic pattern of cortical opacity, starting at the site of application(29), which was not observed in the patients of those studies.
A possible limitation of the present study could be related to differences in the clinical characteristics of patients included in the groups. Although Rehman et al.(15) and Barnes et al.(16) have compared basically patients on maximal tolerated medical therapy, Kirwan et al.(17) performed surgeries in both patients on maximal therapy and those without previous treatment (Table 1). These details could explain differences in the surgical results and represent a potential heterogeneity, however a division in subgroups for statistical purposes could be also a source of bias. Moreover, this analysis was not possible due to the lack of detailed data(17) (Table 3).
The application of beta radiation is rapid and focal, both dose and the area treated can be controlled with accuracy, which reduces the risk of accidental over dosage. A customized applicator is applied only to the desired area. Despite of these advantages of beta radiation, most of glaucoma surgeons choose not to use this procedure probably because the severe adverse events observed in the postoperative period of adjuvant BRT in pterygium surgery. However, we believe that the benefits and complications of the ocular use of beta radiation are open to debate and further studies are necessary.
A previous systematic review has shown similar results(21), however it was based on an extra study, which is not a RCT and has not been completely published yet(30).
In our analysis, a significant IOP reduction was observed in Black patients (P=0.005), however there is only a trend towards a significant difference for the IOP control in the Caucasian patients treated by BRT (P=0.05). Although Black patients have shown an aggressive healing response(31), this difference could be explained by sample size of these trials, instead of a real difference due to ethnic subgroups. The necessary statistic power for these two studies(15,16) able to detect a 10% (postulated) difference in the primary outcome, considering the confidence intervals of 95%, was around 20-25%. In this way, the small number of participants in these studies may compromise the presented statistical analysis. For example, in order to detect a 10% reduction in TREC failure, more than 250 surgeries would be required. Thus, further RCT with an enough sample size should be performed to evaluate the benefits of the BRT in Caucasian patients.
CONCLUSIONS
Our data suggest a significant impact on the outcomes of TREC followed by BRT, mainly in Black patients. Perioperative application of a single dose of BRT in the surgical site showed to be safe, with no significant differences in the frequency of complication, at 12 months follow-up. Further studies are required to assess the impact of BRT in TREC and to determine whether increasing dosage and/or fractionating treatment could enhance the success of routine TREC. Thus, these presented data might be used to guide further randomized clinical trial comparing MMC or 5-FU with adjuvant BRT in glaucoma patients.
REFERENCES
1. Resnikoff S, Pascolini D, Etya'ale D, Kocur I, Pararajasegaram R, Pokharel GP, Mariotti SP. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82(11): 844-51.
2. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. The AGIS Investigators. Am J Ophthalmol. 2000;130(4):429-40.
3. Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M; Early Manifest Glaucoma Trial Group. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002;120(10):1268-79.
4. Addicks EM, Quigley HA, Green R, Robin AL. Histologic characteristics of filtering blebs in glaucomatous eyes. Arch Ophthalmol. 1983;101(5):795-8.
5. Khaw PT, Ward S, Grierson I, Rice NS. Effect of beta radiation on proliferating human Tenon's capsule fibroblasts. Br J Ophthalmol. 1991;75(10):580-3.
6. Miller MH, Rice NS. Trabeculectomy combined with beta irradiation for congenital glaucoma. Br J Ophthalmol. 1991;75(10):584-90.
7. Ruderman JM, Welch DB, Smith MF, Shoch DE. A randomized study of 5-fluorouracil and filtration surgery. Am J Ophthalmol. 1987;104(3):218-24.
8. Yamamoto T, Varani J, Soong HK, Lichter PR. Effects of 5-fluorouracil and mitomycin C on cultured rabbit subconjunctival fibroblasts. Ophthalmology. 1990;97(9):1204-10.
9. Fluorouracil Filtering Surgery Study one-year follow-up. The Fluorouracil Filtering Surgery Study Group. Am J Ophthalmol. 1989;108(6):625-35.
10. Knapp A, Heuer DK, Stern GA, Driebe WT Jr. Serious corneal complications of glaucoma filtering surgery with postoperative 5-fluorouracil. Am J Ophthalmol. 1987;103(2):183-7.
11. Rockwood EJ, Parrish RK 2nd, Heuer DK, Skuta GL, Hodapp E, Palmberg PF, et al. Glaucoma filtering surgery with 5- fluorouracil. Ophthalmology. 1987;94(9):1071-8.
12. Skuta GL, Beeson CC, Higginbotham EJ, Lichter PR, Musch DC, Bergstrom TJ, et al. Intraoperative mitomycin versus postoperative 5-fluorouracil in high-risk glaucoma filtering surgery. Ophthalmology. 1992;99(3):438-44.
13. Weinreb RN. Adjusting the dose of 5-fluorouracil after filtration surgery to minimize side effects. Ophthalmology. 1987;94(5):564-70.
14. Miller MH, Joseph NH, Wishart PK, Hitchings RA. Lack of beneficial effect of intensive topical steroids and beta irradiation of eyes undergoing repeat trabeculectomy. Ophthalmic Surg. 1987;18(7):508-12.
15. Rehman SU, Amoaku WM, Doran RM, Menage MJ, Morrell AJ. Randomized controlled clinical trial of beta irradiation as an adjunct to trabeculectomy in open-angle glaucoma. Ophthalmology. 2002;109(2):302-6.
16. Barnes RM, Mora JS, Best SJ. Beta radiation as an adjunct to low-risk trabeculectomy. Clin Exp Ophthalmol. 2000;28(4):259-62.
17. Kirwan JF, Cousens S, Venter L, Cook C, Stulting A, Roux P, Murdoch I. Effect of beta radiation on success of glaucoma drainage surgery in South Africa: randomised controlled trial. BMJ. 2006;333(7575):942.
18. Ogino N, Masuda H, Abe Y. [Beta-irradiation in the filtering operation]. Nihon Ganka Gakkai Zasshi. 1966;70(11):1834-9. Japanese.
19. Cohen LB, Graham TF, Fry WE. Beta radiation; as an adjunct to glaucoma surgery in the Negro. Am J Ophthalmol. 1959;47(1 Pt 1):54-61.
20. Cameron ME. Beta irradiation as an adjunct to surgery in refractory glaucoma. Trans Aust Coll Ophthalmol. 1970;2:53-60.
21. Kirwan JF, Rennie C, Evans JR. Beta radiation for glaucoma surgery. Cochrane Database Syst Rev. 2009;(2):CD003433. Review.
22. Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet. 1999;354(9193):1896-900. Comment in Lancet. 2005;366(9503):2081-2; author reply 2083-6. Lancet. 1999;354(9193):1834-5. Lancet. 2000;355(9205):756-7.
23. Follmann D, Elliot P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. J Clin Epidemiol. 1992;45(7):769-73.
24. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088-101.
25. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple graphical test. BMJ. 1997;315(7109):629-34.
26. Cochran WG. The combination of estimates from different experiments. Biometrics. 1954;10(1):101-29.
27. Gleckler M, Valentine JD, Silberstein EB. Calculating lens dose and surface dose rates from 90Sr ophthalmic applicators using Monte Carlo modeling. Med Phys. 1998;25(1):29-36.
28. Kirwan JF, Constable PH, Murdoch IE, Khaw PT. Beta irradiation: new uses for an old treatment: a review. Eye (Lond). 2003;17(2):207-15.
29. Thomas CI, Storaasli JP, Friedell HL. Lenticular changes associated with beta irradiation of the eye and their significance. Radiology. 1962;79:588-97.
30. Lai JSM, Ho PCP. Trabeculectomy combined with beta irradiation in uncomplicated primary open angle glaucoma. Invest Ophthalmol Vis Sci. 1994;35:Abstract number 825.
31. Ederer F, Gaasterland DA, Dally LG, Kim J, VanVeldhuisen PC, Blackwell B, Prum B, Shafranov G, Allen RC, Beck A; AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 13. Comparison of treatment outcomes within race: 10-year results. Ophthalmology. 2004;111(4):651-64.
 Correspondence address:
Correspondence address:
Jayter Silva Paula
Departamento de Oftalmologia, Otorrinolaringologia e Cirurgia de Cabeça e Pescoço. Faculdade de Medicina de Ribeirão Preto - Universidade de São Paulo
Av. Bandeirantes, 3.900 - 12º Andar
Ribeirão Preto (SP) - 14049-900 - Brazil
E-mail: [email protected]
Submitted for publication: January 11, 2011
Accepted for publication: August 8, 2011
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: L.I.de Fendi, None; G.V.Arruda, None; V.P.Costa, None; J.S.Paula, None.