

Jayter Silva Paula1; João Marcello Fortes Furtado1; Fabiano Cade Jorge1; Eduardo Melani Rocha1; Ingrid U. Scott2; Luciane Loures dos Santos3; Maria de Lourdes Veronese Rodrigues1; José Sebastião dos Santos4
DOI: 10.1590/S0004-27492011000300006
ABSTRACT
PURPOSE: To describe the procedures used in developing Clinical and Regulatory Protocols for primary care teams to use in the management of the most common scenarios of impaired vision in Southern Brazil. METHODS: A retrospective review of 1.333 referral forms from all primary care practitioners was performed in Ribeirão Preto city, during a 30-day period. The major ophthalmic diagnostic categories were evaluated from those referrals forms. The Clinical and Regulatory Protocols development process was held afterwards and involved scientific cooperation between a university and the health care system, in the form of workshops attended by primary care practitioners and regulatory system team members composed of health care administrators, ophthalmologists, and professors of ophthalmology and social medicine. RESULTS: The management of impaired vision was chosen as the theme, since it accounted for 43.6% of the ophthalmology-related referrals from primary care providers of Ribeirão Preto. The Clinical and Regulatory Protocols developed involve distinctive diagnostic and therapeutic interventions that can be performed at the primary care level and in different health care settings. The most relevant clinical and regulatory interventions were expressed as algorithms in order to facilitate the use of the Clinical and Regulatory Protocols by health care practitioners. CONCLUSIONS: These Clinical and Regulatory Protocols could represent a useful tool for health systems with universal access, as well as for health care networks based on primary care and for regulatory system teams. Implementation of these Clinical and Regulatory Protocols can minimize the disparity between the needs of patients with impaired vision and the treatment modalities offered, resulting in a more cooperative health care network.
Keywords: Vision disorders; Delivery of health care; Public Health; Health Services; Primary health care; Health systems; Clinical protocols
RESUMO
OBJETIVO: Descrever os procedimentos utilizados no desenvolvimento de Protocolos Clínicos e de Regulação, para equipes de atenção primária à saúde, voltados à condução dos cenários clínicos mais comuns de dificuldade visual observados na região sudeste do Brasil. MÉTODOS: Realizou-se a revisão retrospectiva de 1.333 guias de encaminhamento advindas de todos os profissionais da atenção primária da cidade de Ribeirão Preto, durante um período de 30 dias. As principais categorias diagnósticas oftalmológicas foram avaliadas nessas guias de referência. O processo de desenvolvimento dos Protocolos Clínicos e de Regulação ocorreu na sequência e envolveu a cooperação científica entre a universidade e o sistema de saúde, sob a forma de oficinas com médicos da atenção primária e membros da equipe do sistema de regulação, composto por gestores de saúde, oftalmologistas, além de professores de oftalmologia e medicina social. RESULTADOS: A dificuldade visual foi escolhida como tema central, uma vez que representou 43,6% dos encaminhamentos oftalmológicos advindos de serviços de atenção primária de Ribeirão Preto. Os Protocolos Clínicos e de Regulação desenvolvidos envolveram diferentes procedimentos diagnósticos e terapêuticos que podem ser executados na atenção primária e outros níveis ou contextos de cuidados à saúde. As intervenções clínicas e de encaminhamento mais relevantes foram expressas como algoritmos, a fim de facilitar a utilização do protocolo pelos profissionais da saúde. CONCLUSÕES: Os Protocolos Clínicos e de Regulação poderão representar uma ferramenta útil para os sistemas de saúde que contam com acesso universal, bem como para as redes de cuidados de saúde baseadas na atenção primária e nos sistemas de regulação. A implementação de Protocolos Clínicos e de Regulação poderá minimizar a disparidade entre as necessidades dos pacientes com dificuldade visual e as formas de condução de casos oftalmológicos, resultando em uma rede de saúde mais eficiente.
Descritores: Transtornos da visão; Assistência à saúde; Saúde Pública; Serviços de Saúde; Atenção primária à saúde; Sistema de saúde; Protocolos clínicos
ORIGINAL ARTICLE ARTIGO ORIGINAL
Clinical and regulatory protocols for the management of impaired vision in the public health care network
Protocolos clínicos e de regulação para condução da dificuldade visual na rede pública de saúde
Jayter Silva PaulaI; João Marcello Fortes FurtadoII; Fabiano Cade JorgeII; Eduardo Melani RochaI; Ingrid U. ScottIII; Luciane Loures dos SantosIV; Maria de Lourdes Veronese RodriguesI; José Sebastião dos SantosV
IProfessor, Department of Ophthalmology, Otorhinolaryngology and Head and Neck Surgery. Ribeirão Preto School of Medicine, Universidade de São Paulo - USP - Ribeirão Preto (SP), Brazil
IIPhysician, Department of Ophthalmology, Otorhinolaryngology and Head and Neck Surgery. Ribeirão Preto School of Medicine, Universidade de São Paulo - USP - Ribeirão Preto (SP), Brazil
IIIProfessor, Departments of Ophthalmology and Public Health Sciences, Penn State College of Medicine, Hershey, Pennsylvania, USA
IVProfessor, Department of Social Medicine, Ribeirão Preto School of Medicine, Universidade de São Paulo - USP - Ribeirão Preto (SP), Brazil
VProfessor, Department of Surgery and Anatomy, Ribeirão Preto, School of Medicine Universidade de São Paulo - USP - Ribeirão Preto (SP), Brazil
ABSTRACT
PURPOSE: To describe the procedures used in developing Clinical and Regulatory Protocols for primary care teams to use in the management of the most common scenarios of impaired vision in Southern Brazil.
METHODS: A retrospective review of 1.333 referral forms from all primary care practitioners was performed in Ribeirão Preto city, during a 30-day period. The major ophthalmic diagnostic categories were evaluated from those referrals forms. The Clinical and Regulatory Protocols development process was held afterwards and involved scientific cooperation between a university and the health care system, in the form of workshops attended by primary care practitioners and regulatory system team members composed of health care administrators, ophthalmologists, and professors of ophthalmology and social medicine.
RESULTS: The management of impaired vision was chosen as the theme, since it accounted for 43.6% of the ophthalmology-related referrals from primary care providers of Ribeirão Preto. The Clinical and Regulatory Protocols developed involve distinctive diagnostic and therapeutic interventions that can be performed at the primary care level and in different health care settings. The most relevant clinical and regulatory interventions were expressed as algorithms in order to facilitate the use of the Clinical and Regulatory Protocols by health care practitioners.
CONCLUSIONS: These Clinical and Regulatory Protocols could represent a useful tool for health systems with universal access, as well as for health care networks based on primary care and for regulatory system teams. Implementation of these Clinical and Regulatory Protocols can minimize the disparity between the needs of patients with impaired vision and the treatment modalities offered, resulting in a more cooperative health care network.
Keywords: Vision disorders; Delivery of health care; Public Health; Health Services; Primary health care; Health systems; Clinical protocols
RESUMO
OBJETIVO: Descrever os procedimentos utilizados no desenvolvimento de Protocolos Clínicos e de Regulação, para equipes de atenção primária à saúde, voltados à condução dos cenários clínicos mais comuns de dificuldade visual observados na região sudeste do Brasil.
MÉTODOS: Realizou-se a revisão retrospectiva de 1.333 guias de encaminhamento advindas de todos os profissionais da atenção primária da cidade de Ribeirão Preto, durante um período de 30 dias. As principais categorias diagnósticas oftalmológicas foram avaliadas nessas guias de referência. O processo de desenvolvimento dos Protocolos Clínicos e de Regulação ocorreu na sequência e envolveu a cooperação científica entre a universidade e o sistema de saúde, sob a forma de oficinas com médicos da atenção primária e membros da equipe do sistema de regulação, composto por gestores de saúde, oftalmologistas, além de professores de oftalmologia e medicina social.
RESULTADOS: A dificuldade visual foi escolhida como tema central, uma vez que representou 43,6% dos encaminhamentos oftalmológicos advindos de serviços de atenção primária de Ribeirão Preto. Os Protocolos Clínicos e de Regulação desenvolvidos envolveram diferentes procedimentos diagnósticos e terapêuticos que podem ser executados na atenção primária e outros níveis ou contextos de cuidados à saúde. As intervenções clínicas e de encaminhamento mais relevantes foram expressas como algoritmos, a fim de facilitar a utilização do protocolo pelos profissionais da saúde.
CONCLUSÕES: Os Protocolos Clínicos e de Regulação poderão representar uma ferramenta útil para os sistemas de saúde que contam com acesso universal, bem como para as redes de cuidados de saúde baseadas na atenção primária e nos sistemas de regulação. A implementação de Protocolos Clínicos e de Regulação poderá minimizar a disparidade entre as necessidades dos pacientes com dificuldade visual e as formas de condução de casos oftalmológicos, resultando em uma rede de saúde mais eficiente.
Descritores: Transtornos da visão; Assistência à saúde; Saúde Pública; Serviços de Saúde; Atenção primária à saúde; Sistema de saúde; Protocolos clínicos
INTRODUCTION
The Brazilian Sistema Único de Saúde (SUS, Unified Health Care System), established in 1988, provides universal, decentralized access to health care and has increasingly become a hierarchically complex network based on primary health care(1,2).
Although implementation of the SUS has amplified the primary health care structure, inefficient clinical interventions and poor primary care coordination have resulted in excessive demand for specialized and emergency care services(3). Measures adopted in order to streamline access to various health care services include the implementation of the Regulatory System (RS), which is aimed at mapping the allocation of health care resources and structuring the various regulatory bodies. Non-emergency cases that require specialty care are referred to a RS team via the heath care network. Medical teams and users can also consult the various RS units, the emergency unit in particular, by telephone, internet and fax(3-5).
Ineffective ophthalmologic interventions and limited knowledge of community eye health on the part of primary care providers have led to various problems related to local treatment and referral of ophthalmologic cases. The objective of the present study was to evaluate the major ocular conditions in patients referred to health care clinics, as well as to present Clinical and Regulatory Protocols (CRPs) for the treatment and management of those conditions, developed through scientific cooperation between the university and the health care system.
METHODS
SELECTION OF THEMES FOR DEVELOPING CRPS
The CRPs presented here were developed by ophthalmologists, general practitioners, nurses and representatives of the Municipal Health Department of the city of Ribeirão Preto, Brazil. The CRP themes were categorized as "mixed" (when no specified ocular diagnosis was mentioned) or "authentic" (when a specific ophthalmologic problem/diagnosis was described or suspected) based on ophthalmic cases included on the referral forms reviewed. Treatment, conduction or any kind of clinical resolution proposed for a specific theme implied in the use of several health care network elements and other social resources.
The themes were analyzed and selected, in workshops, by a team composed of two primary care practitioners (family physicians) and two specialized health practitioners (ophthalmologists) associated with the University of São Paulo (a matrix care team) and an RS team, composed of three health care administrators. In order to identify the major ocular problems, we surveyed all ophthalmic patients referred to Ribeirão Preto Municipal Health Department clinics in August of 2007. The themes selected are representative of the most prevalent problems in the health care network.
GUIDELINES FOR CRP DEVELOPMENT
Each CRP defines the clinical dimension of a given theme in terms of the various health care network elements involved, as well as stating whether and why specialized services of moderate or high complexity must be provided. The CRP format includes a brief introduction of the theme, including clinical findings setting limits for each service provided. Relevant observations can be attached together with bibliographic references. In accordance with the recommendations of the World Health Organization(6) and the Pan American Health Organization, the guidelines used for CRP development are based on scientific evidence, collected from the systematic reviews published by the Brazilian Cochrane Centre and PubMed citations, as well as from publications describing Brazilian health care policies related to treatment allocation and regulation of user access to the SUS(7-11).
The CRPs were developed by the matrix team under the supervision of a technical group (composed of two professors of ophthalmology and one professor of social medicine) designated to monitor the methodological aspects. The content of each protocol mirrors the multidisciplinary intervention undertaken to handle a specific health-related problem and is in accordance with the policies of the national and local health care networks.
The rationale for regulating access to health care services is based on using primary care as a portal of entry, both in terms of elective needs and referral to other health providers(2-11). Emergency cases of low complexity can be addressed at the primary care level, whereas severe cases must be referred to emergency care facilities as required by the regulatory guidelines(3-5).
The technical and regulatory components of the CRPs reflect the interactions among the facilities (hospitals, health care clinics, ambulance services, etc.) available in the community under study, taking into consideration their complexity and capacity, which may be useful as an example of the health system as a whole. Clinically, CRPs for impaired vision are grounded in the description of ophthalmic signs and symptoms, or of the disease itself. The CRPs presented here were revised by the technical group linked to the Ribeirão Preto Municipal Health Department and services provided by the Department itself.
DEFINITION OF IMPAIRED VISION
Impaired or blurred vision, in one or both eyes, should be preferentially measured using a logMAR chart (visual acuity of a normal eye was then recorded as decimals, for example, 1.0). Normal visual acuity can vary according to patient age, as follows: 6 months to 2 years - fixate and maintain steady fixation on light and objects; 2 to 5 years - 0.5 or better; and older than 5 years - 0.7 or better and a difference of less than two lines between eyes. Patients who do not reach these levels of visual acuity are classified as having impaired vision. The findings of the clinical history, examination parameters and results of visual acuity measurement, should all be addressed on the referral form, together with individual patient data, prior to the proposal of diagnoses. The RS team uses these forms to refer patients to a higher level of the SUS for an ophthalmologic consultation.
CRPS FOR VISUAL IMPAIRMENT
Considering the SUS administrative planning and the multidisciplinary research goals, CRPs for visual impairment were developed according to the methods proposed for the five most common clinical scenarios.
RESULTS
PRINCIPAL OPHTHALMOLOGICAL CONDITIONS IN CASES REFERRED FROM HEALTH CARE CLINICS
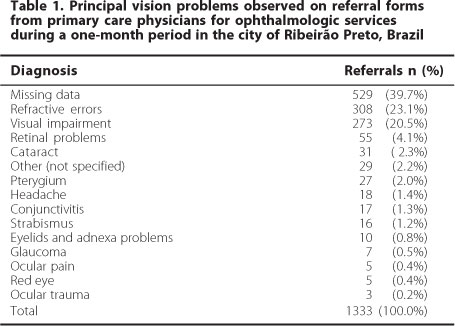
In evaluating the records related to all cases referred for ophthalmological treatment during the study period, we found the principal conditions to be suspected are refractive error (in 23.1%) and undiagnosed impaired vision (in 20.5 %), although 39.7 % of the case files were incomplete (Table 1). Since the majority of refractive error suspects are accompanied by some degree of impaired or blurred vision, 43.6 percent of the cases could be said to be associated with a diagnosis of impaired vision. Based on these findings, we decided to create CRPs for impaired vision and the various conditions with which it is associated. Table 2 details the CRP for each scenario, and Figure 1 provides an overview.
DISCUSSION
The reality of health care in Brazil is far from the SUS concepts theoretically ensured by the laws, policies and rules. According to new concepts, norms and governmental decrees, primary health care is the main portal for clinical interventions and is expected to coordinate access to all levels of treatment(2,7,8,10) whereas the RS is charged with the evaluation of all referrals and with the coordination of patient flow to specific components of the health care network depending on the health needs of the user(3-5,9,11). Difficulties in this coordination have contributed to the decision to amplify and strengthen primary health care, as well as to implement the RS, at the local level. Despite such difficulties, these objectives have been met and the RS implementation process has been discussed(3-5,9,12). The development, validation, and dissemination of the CRPs, which involve efforts by primary care practitioners, academicians and RS team members, might contribute to the development of the bases underlying the health care networks in various specialties(3,8,12).
In general, protocols described in the literature address only clinical elements and are designed to coordinate specific interventions, such as outpatient, inpatient and intensive care. Therefore, the challenge resides not only in organizing clinical and regulatory interventions using CRPs but also in validating these CRPs in cooperation with primary care practitioners and managers in order to ensure integrity and equity(3,13).
Impaired vision was chosen as the major theme here because we observed that a considerable portion of the cases referred for ophthalmology consults were in patients who presented with refractive errors or with some degree of undiagnosed impaired vision, both of which are frequently associated with blurred vision(14). In our region, forms that are missing data might account for many of the difficulties encountered by primary health care physicians in understanding ocular conditions. It is likely that many of these forms were related to patients with some kind of impaired vision. These difficulties might be associated with a lack of knowledge and experience in ophthalmology on the part of general practitioners, which probably dates back to their university education. However, the present CRP, which was based on simple ophthalmologic details, could help general practitioners in solving ocular problems adequately through the health care system.
The development of a CRP requires knowledge of scientific, operational and administrative processes, making it a potential tool for qualifying health care delivery, improving professional skills and facilitating treatment access. One limitation of the present study was the failure to consider other potential causes of impaired vision. However, the primordial objective here was to organize relevant ophthalmic scenarios based on the reality of primary health care.
The management of impaired vision involves various clinical forms, ranging from mild to severe. It is common to see patients with mild blurred vision, due to acute conjunctivitis, referred to tertiary emergency hospitals for specialized investigation. In contrast, it is likely that there are patients with severe uveitis who encounter difficulties in gaining access to such treatment.
In general, primary care teams have immediately referred the majority of simple cases, such as cases of conjunctivitis, for tertiary care. We believe that the treatment of such cases can be initiated at the primary care level, being referred for specialized attention only if there is no healing. However, patients presenting with signs and symptoms of cataracts should be sent to secondary or tertiary care for surgery. Therefore, correct diagnoses made at the primary care level could reduce treatment delays.
The inequities between clinical and social conditions, embodied by the inability of some patients to undergo clinical evaluations, exams and procedures, are imposed by a fragmented health care system that lacks coordination and organization. These inequities result in generalized dissatisfaction, treatment delay and wasted resources. Once developed, CRPs for impaired vision need to be validated in order to promote appropriate access to the best quality vision care, defined as receiving clinical eye care from the right professional, at the right time and in the right place.
The CRPs described here can further the understanding of ophthalmological issues by general physicians, promoting accurate diagnosis and rapid movement of patients through the health care system.
CONCLUSIONS
Impaired vision was a common ophthalmic reason of referrals in the primary care services and the presented CRPs could improve the ophthalmological knowledge in those settings as well as the efficacy of this hierarchical-based referral system.
REFERENCES
1. Brasil. Ministério da Saúde. Lei nº 8142/90 de 28 de dezembro de 1990. Dispõe sobre a participação da comunidade na gestão do Sistema Único de Sáude (SUS) e sobre as transferências intergovernamentais de recursos financeiros na área da saúde e dá outras providências [Internet]. Brasília; MS; 1990. [citado 2010 Dez 12]. Disponível em: http://www.jusbrasil.com.br/legislacao/109610/lei-8142-90
2. Starfield B. Primary care: concept, evaluation and policy. New York: Oxford University Press; 1992.
3. Santos JS, Kemp R, Sankarankutty AK, Salgado Jr W, Souza FF, Teixeira AC, et al. Clinical and regulatory protocol for treatment of jaundice in adults and elderly: a support for health care network and regulatory system. Acta Cir Bras. 2008;23 Suppl 1:133-42.
4. Lopes SL, Santos JS, Scarpelini S. The implementation of the medical regulation office and mobile emergency attendance system and its impact on the gravity profile of non-traumatic afflictions treated in a University Hospital: a research study. BMC Health Serv Res. 2007;7:173.
5. Santos JS, Scarpelini S, Brasileiro SL, Ferraz CA, Dalloro ME, Sá MF. Avaliação do modelo de organização da Unidade de Emergência do HCFMRP-USP, adotando, como referência as políticas nacionais de atenção às urgências e de humanização. Medicina (Ribeirão Preto). 2003; 36(2/4):498-515.
6. World Health Organization. Global Programme on Evidence for Health Policy. Guidelines for WHO Guidelines [Internet]. Geneva: WHO; 2003. [cited 2010 Jan 12]]. Available from: http://whqlibdoc.who.int/HQ/2003/EIP_GPE_EQC_2003_1.pdf
7. Brazilian Heath Ministry´s. Law number 399; February 22, 2006. [Internet]. Disponível em: http://dtr2001.saude.gov.br/sas/PORTARIAS/Port2006/GM/GM-399.htm
8. Brasil. Ministério da Saúde. Portaria nº. 399/GM de 22 de fevereiro de 2006. Divulga o pacto pela saúde 2006- Consolidação do SUS e aprova as diretrizes operacionais do referido pacto [Internet]. Brasília: MS; 2006. [citado 2009 Nov 20]. Disponível em: em: http://www.mp.go.gov.br/portalweb/hp/2/docs/ma_pga2008_por._399_colegiado_ de_gestao.pdf
9. Ribeirão Preto. Prefeitura Municipal de Ribeirão Preto. Secretaria Municipal da Saúde. Plano de saúde de Ribeirão Preto: período 2005-2008. Ribeirão Preto (SP); 2005. [citado em 2006 Fev 24]. Disponível em: http://www.ribeiraopreto.sp.gov.br/ssaude/vigilancia/planeja/plano05-08.Pdf
10. Brasil. Ministério da Saúde. Portaria nº. 1101 de 12 de junho de 2002. Estabelece os parâmetros de cobertura assistencial sejam estabelecidos pela Direção Nacional do Sistema Único de Saúde - SUS [Internet]. Brasília: MS; 2002. [citado em 2006 Jul 27]. Disponível em: http://dtr2001.saude.gov.br/sas/PORTARIAS/Port2002/Gm/GM-1101.htm
11. Persaud DD, Jreige S, LeBlanc RP. Enhancing vision care integration: 1. Development of practice algorithms. Can J Ophtalmol. 2004;39(3):219-24.
12. Persaud DD, Jreige S, LeBlanc RP. Enhancing vision care integration: 2. Implementation of practice algorithms. Can J Ophtalmol. 2004; 39(3):225-33.
13. Hartz ZM, Contandripolus AP. [Comprehensive health care and integrated health services: challenges for evaluating the implementation of a "system without walls"]. Cad Saude Publica. 2004;20 Suppl 2:331-6. Portuguese.
14. Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ. 2008;86(1):63-70. Comment in: Bull World Health Organ. 2008;86(8): B-C; author reply C.
 Correspondence address:
Correspondence address:
Jayter Silva Paula
Department of Ophthalmology, Otorhinolaryngology and Head and Neck Surgery. Ribeirão Preto School of Medicine - University of São Paulo
Av. Bandeirantes, 3900 - 12º. Andar
Ribeirão Preto - SP
14049-900 - Brazil
E-mail: [email protected]
Submitted for publication: March 10, 2011
Accepted for publication: April 21, 2011
Study was carried out at the Ribeirão Preto School of Medicine - University of São Paulo
Funding: This study was supported by CNPq, FAEPA and Fundação Waldemar Barnsley Pessoa.
Disclosure of potential conflicts of interest: Paula JS, None; Furtado JMF, None; Jorge FC, None; Rocha EM, None; Scott IU, None; dos Santos LL, None; Rodrigues MLV, None; dos Santos JS, None.