

Cristina Miyamoto1; Lilian Cristina Espírito Santo1; Luiz Roisman1; Pilar de Andrade Memoria Moreno1; Angelino Julio Cariello1; Midori Hentosa Osaki1
DOI: 10.1590/S0004-27492011000100016
ABSTRACT
Floppy eyelid syndrome is characterized by the easy evertion of the upper eyelid which occurs spontaneously during the sleep, causing the exposure of the eye surface and chronic papillary conjunctivitis. Its pathogenesis is not totally defined yet: it is usually more frequent in middle-aged, male obese patients and it is associated with systemic disorders such as obstructive sleep apnea, high blood pressure and diabetes. On the occasions which conservative treatment fails, surgical procedures present good results, including surgical techniques which are constantly evolving.
Keywords: Conjunctiva; Conjunctivitis; Ectropion; Obesity; Hypertension; Diabetes Mellitus; Sleep apnea, obstructive; Eyelid diseases; Syndrome; Oculomotor Muscles; Eyelids; Corneal diseases
RESUMO
A síndrome de frouxidão palpebral é caracterizada pela fácil eversão da pálpebra que ocorre espontaneamente durante o sono causando exposição dos olhos, com consequente conjuntivite papilar crônica. Sua patogênese ainda não está totalmente definida e é mais comum em pacientes masculinos, obesos, de meia idade e está associada a doenças sistêmicas como apnéia obstrutiva do sono, hipertensão arterial e diabetes. Quando o tratamento clínico não apresenta boa resposta, procedimentos cirúrgicos apresentam bons resultados, com técnicas em constante evolução.
Descritores: Conjuntiva; Conjuntivite; Ectrópio; Obesidade; Hipertensão; Diabete Mellitus; Apnéia do sono tipo obstrutiva; Doenças palpebrais; Síndrome; Músculos oculomotores; Pálpebras; Doenças da córnea
CURRENT UPDATE
Floppy eyelid syndrome: review
Síndrome da frouxidão palpebral: revisão da literatura
Cristina Miyamoto; Lilian Cristina Espírito Santo; Luiz Roisman; Pilar de Andrade Memoria Moreno; Angelino Julio Cariello; Midori Hentosa Osaki
Physician, Department of Ophthalmology, Federal University of São Paulo - UNIFESP - São Paulo (SP), Brazil
ABSTRACT
Floppy eyelid syndrome is characterized by the easy evertion of the upper eyelid which occurs spontaneously during the sleep, causing the exposure of the eye surface and chronic papillary conjunctivitis. Its pathogenesis is not totally defined yet: it is usually more frequent in middle-aged, male obese patients and it is associated with systemic disorders such as obstructive sleep apnea, high blood pressure and diabetes. On the occasions which conservative treatment fails, surgical procedures present good results, including surgical techniques which are constantly evolving.
Keywords: Conjunctiva/pathology; Conjunctivitis; Ectropion; Obesity/complications; Hypertension/complications; Diabetes Mellitus/complications; Sleep apnea, obstructive/complications; Eyelid diseases/surgery; Syndrome; Oculomotor Muscles/surgery; Eyelids/surgery; Corneal diseases
RESUMO
A síndrome de frouxidão palpebral é caracterizada pela fácil eversão da pálpebra que ocorre espontaneamente durante o sono causando exposição dos olhos, com consequente conjuntivite papilar crônica. Sua patogênese ainda não está totalmente definida e é mais comum em pacientes masculinos, obesos, de meia idade e está associada a doenças sistêmicas como apnéia obstrutiva do sono, hipertensão arterial e diabetes. Quando o tratamento clínico não apresenta boa resposta, procedimentos cirúrgicos apresentam bons resultados, com técnicas em constante evolução.
Descritores: Conjuntiva/patologia; Conjuntivite; Ectrópio; Obesidade/complicações; Hipertensão/complicações; Diabete Mellitus/complicações; Apnéia do sono tipo obstrutiva/complicações; Doenças palpebrais/cirurgia; Síndrome; Músculos oculomotores/cirurgia; Pálpebras/cirurgia; Doenças da córnea
INTRODUCTION
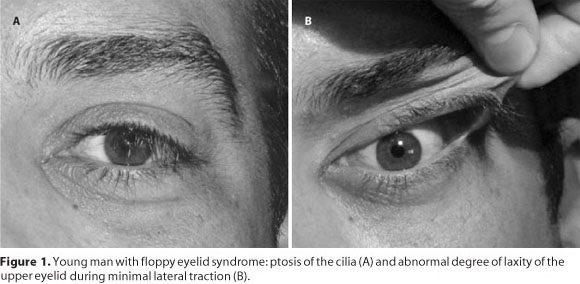
Floppy eyelid syndrome (FES), first reported in 1981 by Culbertson and Ostler(1), is recognized by a loose upper lid that readily everts by pulling it upward(1) (Figure1), a soft, rubbery tarsus that can be easily folded(2), and chronic papillary conjunctival response(1,3). Patients with this syndrome generally complain about non-specific irritation, foreign body sensation, mucoid discharge, dryness, redness, photosensitivity, eyelid swelling and decreased vision(4-5).
These symptoms are usually worse on awakening in the morning, and the affected side seems to correspond to the side the patient usually sleeps(1). In most cases, the patient is chronically treated with topical therapeutic agents with no response. Although initially reported to be typical in middle-aged overweight men(1,3), FES has also been found in women, different age groups, and no obese patients(6-7). The syndrome is not completely understood and it may be associated with many systemic and ophthalmic diseases such as obesity, obstructive sleep apnea, hypertension, ischemic heart disease, skin and collagen pathologies, corneal and eyelids abnormalities and glaucoma.
The treatment is basically surgical, however clinical management, like eye shields, lubricants and weight loss can be efficient in some cases. The purpose of this article is to make a review of floppy eyelid syndrome emphasizing the main associated conditions, theories about its pathogenesis, and treatments.
PATHOGENESIS
Since the initial description of the floppy eyelid syndrome in 1981, several hypotheses have been made for its pathogenesis. Culbertson and Ostler(1), who first pointed out this condition, postulated that spontaneous nocturnal eversion of the upper eyelid would cause events, such as mechanical insult to the conjunctiva, subsequent papillary conjunctivitis and conjunctival keratinization leading to the loss of tarsal elasticity. They made this hypothesis based on the observation that the ocular signs and symptoms are generally more frequent and/or more severe in the eye corresponding to the side on which the patient prefers to sleep. They also suggested an X-chromosome-linked inheritance pattern or hormone influence associated to the problem, since they only found it in men.
Parunovic(2), however, proposed that the laxity of the lids was the cause of the irritative symptoms mentioned by the patients. The reduced interface between the loose eyelids and the epibulbar surface would compromise the distribution of the tear film over the cornea and conjunctiva, producing poor wetting and subsequent ocular surface disease. This proposition was based on diffuse keratitis found in FES different of that one usually localized resulting from nocturnal exposure. Schwartz et al.(8) and Goldberg et al.(9) also suggested this mechanism of injury.
Later, other researchers postulated that a genetically predisposition, like genetic abnormalities in collagen, elastin, or both, associated with age and sleeping patterns, would cause the FES(3,10). The obstructive sleep apnea (OSA), often present in patients with FES, lead to the hypothesis that a common underlying connective tissue disorder would explain the syndrome. Redundancy of tissue in the tarsal plate of lateral canthal tendons might contribute to the development of FES, like the excess of oropharyngeal tissues found in OSA cause upper airway obstruction specially when the person is sleeping(3,11-12).
Inflammation was also pointed out as a contributing factor to FES. Since blepharochalasis and FES share many of the same ocular findings and significant chronic inflammation are encountered in both conditions, a theory of a common inflammatory pathway was made. Inflammation would cause generalized atrophy and attenuation of muscles, tendons and ligaments. Nevertheless, histological studies of the tarsus showed normal structure along with the presence of chronic inflammatory infiltrate(3,11).
Hyperglycinemia was another condition that was speculated to be involved in the pathogenesis of FES, because glycine is present in high concentrations in collagen and gelatin, and a patient with floppy lids and hyperglycinemia was described. The high concentration of glycine in collagen would induce structural changes in the tarsus(6). Goldberg et al., however, observed that hyperglycinemia is not classically associated with collagen disorders(9).
Another theory claims that a combination of local pressure-induced lid ischemia and systemic hypoventilation followed by reperfusion oxidation injury during sleep (sleep apnea) is responsible for changes, such as chronic inflammation, which leads to higher temperature and lost of the normal barrier against water evaporation. This, in turn, would cause additional damage to the skin and this vicious cycle would aggravate lid inflammation, contributing to meibomian gland dysfunction, a condition that might be associated with FES(12) and lid floppiness(4). The nonspecific ocular surface irritation related with FES might be due to abnormality in tear film dynamics. There is a high correlation between the eye with worse symptoms with more severe floppy lids and the ocular surface evaporation rate. Tear film alterations is prevalent in patients with FES, most of them due to lipid tear deficiency(4), which might be caused by abnormalities of meibomian glands(12).
Since the main finding in FES is the laxity of the lids, as the name of the syndrome suggests, it was postulated that alterations in collagen would explain this condition. In fact, mutations in the type V collagen genes COL5A1 and COL5A2 were found in patients with ocular phenotype of classic Ehlers-Danlos syndrome (EDS), a disease characterized by laxity and fragility of soft connective tissues. Type V collagen is a quantitatively minor fibril-forming collagen that is present in type I collagen-rich connective tissues such as dermis, tendon and ligament. Mechanisms producing the abnormalities in those tissues were probably associated with altered regulation of collagen fibrillogenesis due to alterations in heterotypic I/V collagen interactions(5). Meanwhile, tarsal collagen appeared normal using hematoxylin-eosin and Masson trichrome stains in eyelid biopsy specimens of FES patients, and electron microscopy showed that the quantity of collagen in the tarsus was normal. Also, the localization of collagen types I and III was similar in patients with FES and controls(12).
Reduced amount of tarsal elastin was observed in patients with FES by immunohistochemical studies using Verhoeff's modified elastin stain suggesting that abnormal elastogenesis might be associated with this syndrome(12). The marked decrease in the amount of elastin within the tarsal plate and eyelid skin, however, might be explained by an up-regulation of elastolytic enzymes, particularly matrix metalloproteinases 7 and 9 (MMP-7 and MMP-9), most probably stimulated by repeated mechanical stress, like eye rubbing and sleeping habits. This up-regulation could also be the cause of eyelash misdirection frequently found in FES(10). The up-regulation of matrix metalloproteinase (MMP) expression, by the way, might be due to elevated levels of leptin that has been shown to regulate the expression of MMP-9 in a dose-dependent manner. Besides, hyperleptinemia correlates positively with the severity of obstructive sleep apnea (OSA), a condition frequently present in patients with FES. Therefore, hyperleptinemia may be involved in the pathogenesis of both FES and OSA(5).
CORNEAL ABNORMALITY AND SYSTEMIC CONDITIONS RELATED WITH FLOPPY EYELID SYNDROME
Corneal abnormality
Culbertson and Tseng(13), in a retrospective review of 60 patients with floppy eyelid syndrome followed at the Bascom Palmer Eye Institute found a prevalence of seventy-one per cent of patients with clinically significant corneal abnormalities related with FES, that could affect all layers of cornea. Punctate epithelial keratitis was described as the most common corneal disorder, usually diffuse and found only in the involved eye(13).
Another corneal abnormality reported by Culberston and Tseng(13) was keratoconus, present in 10% of all patients. FES associated with keratoconus was also described by Parunovic(2), Donnenfeld et al.(14), and Negris(15). Corneal endotheliopathy associated with FES was described as a progressive non guttate dystrophy and as a possible Chandler's variant of the iridocorneal endothelial syndrome(13). Other corneal signs include subepithelial scarring and deep neovascularization(16).
OBSTRUCTIVE SLEEP APNEA
Obstructive sleep apnea (OSA) is characterized by intermittent and repeated interruption of airflow during the sleep due to elevated airway resistance. It causes sleep disorder, waking the patient during the night, resulting in excessive daytime somnolence. The patient could present snoring and arterial hypertension. This syndrome is strongly associated with obesity and FES(17). The diagnosis is made by polysomnography and the treatment is based in losing weight. Severe cases may be treated by uvulopalatopharyngoplasty and continuous positive airway pressure (CPAP). The first case associating this entities was reported in 1987 by Gonnering and Sonneland (18). In 1989, Goldberg et al.(9), described another patient with ectropion due to FES and sleep disorders that they called Pickwickian respiratory syndrome. No conclusion between this association had been taken yet.
In 1990, Young et al.(17) reported 3 patients with FES and OSA and proposed a tissue abnormality to correlate these two syndromes. In 1987, Gonnering and Sonelland(18) selected patients with FES to underwent polysomnography and patients with OSA to be examined for ocular abnormalities and measurement of vertical upper lid pull. In a group of 8 patients with FES, all of them had also OSA in different degrees; however, among 20 patients with OSA, only one case of FES was diagnosed. Nevertheless, measurement of vertical upper lid pull was significantly higher in these patients compared with normal population. McNab(18) also showed one patient with the 2 entities, that improved of FES after treatment of OSA (uvulopalatopharyngoplasty and CPAP), with no papillary conjunctivis and normal lid laxity(19).
In 2005, McNab(20) analyzed 50 patients with FES and found that 96% of them had symptoms of OSA. Seventeen of these patients were undergone sleep studies and in sixteen (94%) was confirmed the diagnosis of OSA. This result corroborated with his previous study showing that patients with FES and OSA had worse degrees of severity, higher number of apnoeic or hypopnoiec episodes per hour, and lower minimum saturation of arterial oxygen, when compared with patients who had only OSA. It suggests that FES is a severity marker of OSA. In 2006, Karger et al.(21) confirmed McNab findings. They encountered an association with subjectively easy lid eversion and sleep disorders, but a low frequency of FES. According to currently data, most of the patients with FES have OSA, however the opposite is not true. Patients with FES should undergo polysomnography to evaluate a possible OSA, whose treatment could give a better life quality to the patient.
Several other systemic conditions have already been associated with FES, such as diabetes, ischemic heart disease, hypercholesterolemia, osteoarthritis, asthma, gastroesophageal reflux disease, chronic renal failure, and schizophrenia(22). However, many of these conditions are directly or indirectly linked with obesity, which may represent a confounding factor.
TREATMENT
Based on the speculative etiologies of FES, many different kinds of clinical and surgical treatments were proposed. The clinical treatment involves losing weight, taping the eyelids during the night(1), eye shields and topical lubricants(2). Improvement of FES manifestations by the treatment of OSA with CPAP was seen by McNab(19).
The surgical techniques changed in the years and are constantly being improved to treat this condition. Gerner and Hughes(6) first described a shortening procedure in a patient with hyperglycinemia and floppy eyelids. Dutton had also tried an eyelid shortening procedure, in which a full thickness resection of the lateral one third to one half of the eyelid was performed with primary layered closure(23). Later, lateral tarsorrhaphy was used by Bouchard(24).
Karesh et al.(25) had done a similar procedure to Dutton's by using a lateral canthal tendon placation, and lower eyelid horizontal shortening. Despite of the good effectiveness, these procedures do not have a fine aesthetic result. Therefore, Periman and Sires(26) presented a modified technique in which a temporally placed, modified back tapered wedge resection and advancement flap is used to create a wound and scar that satisfactorily falls within or more nearly parallel to the eyelid crease, camouflaging it, having a better cosmetic result. More recently, Burkat and Lemke(27) described a lateral tarsal strip fixation to periosteal flaps based inside the orbital rim to achieve horizontal tightening, with 91% of improvement of symptoms in a follow-up of 52 months.
Valenzuela and Sullivan(28) performed, based on the presence of predominately medial upper laxity, a medial upper eyelid horizontal shortening with an upper eyelid skin reduction when excess of skin was present, and some other patients also underwent horizontal lower eyelid shortening additionally or not to the lower eyelid retractor plication. The authors had a great success in 18 months of follow-up, with relief of the symptoms and good aesthetic appearance.
Besides the surgical management is the main and more effective treatment for FES, a long-term study(29) involving 71 patients who had undergone surgery for FES at Moorfields Eye Hospital demonstrate significant recurrence rates varying from 25.6% to 60.6% depending on the procedure used. The data provided by this showed better survival outcomes using the medial canthal and lateral canthal plication and upper lid lateral tarsal strip procedures in comparison with the full-thickness wedge excision procedure, which was recommended to be avoided(29).
REFERENCES
1. Culbertson WW, Ostler HB. The floppy eyelid syndrome. Am J Ophthalmol. 1981;92(4):568-75.
2. Parunovic A. Floppy eyelid syndrome. Br J Ophthalmol. 1983;67(4):264-6.
3. Brown MD, Potter JW. Floppy eyelid syndrome: a case report and clinical review. J Am Optom Assoc. 1992;63(5):309-14.
4. Leibovitch I, Selva D. Floppy eyelid syndrome: clinical features and the association with obstructive sleep apnea. Sleep Med. 2006;7(2):117-22. Comment in: Sleep Med. 2006;7(2): 97-9.
5. Taban M, Taban M, Perry JD. Plasma leptin levels in patients with floppy eyelid syndrome. Ophthal Plast Reconstr Surg. 2006;22(5):375-7.
6. Gerner EW, Hughes SM. Floppy eyelid with hyperglycinemia. Am J Ophthalmol. 1984;98(5): 614-6.
7. Segev F, Heon E, Cole WG, Wenstrup RJ, Young F, Slomovic AR, et al. Structural abnormalities of the cornea and lid resulting from collagen V mutations. Invest Ophthalmol Vis Sci. 2006;47(2):565-73.
8. Schwartz LK, Gelender H, Forster RK. Chronic conjunctivitis associated with "floppy eyelids". Arch Ophthalmol. 1983;101(12):1884-8.
9. Goldberg RA, Coden DJ, Hornblass A, Mitchell JP. Floppy eyelid syndrome associated with marked lower eyelid ectropion. Am J Ophthalmol. 1989;108(5):610-2.
10. Schlotzer-Schrehardt U, Stojkovic M, Hofmann-Rummelt C, Cursiefen C, Kruse FE, Holbach LM. The pathogenesis of floppy eyelid syndrome: involvement of matrix metalloproteinases in elastic fiber degradation. Ophthalmology. 2005;112(4):694-704.
11. Netland PA, Sugrue SP, Albert DM, Shore JW. Histopathologic features of the floppy eyelid syndrome. Involvement of tarsal elastin. Ophthalmology. 1994;101(1):174-81.
12. Liu DT, Di Pascuale MA, Sawai J, Gao YY, Tseng SC. Tear film dynamics in floppy eyelid syndrome. Invest Ophthalmol Vis Sci. 2005;46(4):1188-94.
13. Culbertson WW, Tseng SC. Corneal disorders in floppy eyelid syndrome. Cornea. 1994; 139(1):33-42.
14. Donnenfeld ED, Perry HD, Gibralter RP, Ingraham HJ, Udell IJ. Keratoconus associated with floppy eyelid syndrome. Ophthalmology. 1991;98(11):1674-8.
15. Negris R. Floppy eyelid syndrome associated with keratoconus. J Am Optom Assoc. 1992; 63(5):316-9.
16. Dufek MA, Schechtman DL. Floppy eyelid syndrome: a diagnostic dilemma. J Am Optom Assoc. 1999;70(7):450-4.
17. Young TT, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165(9):1217-39.
18. Gonnering RS, Sonelland PR. Meibomiam gland dysfunction in floppy eyelid syndrome. Ophthal Plast Reconstr Surg. 1987;3(2):99-103.
19. McNab AA. Reversal of floppy eyelid syndrome with treatment of obstructive sleep apnoea. Clin Experiment Ophthalmol. 2000;28(2):125-6.
20. McNab AA. The eye and sleep. Clin Experiment Ophthalmol. 2005;33(2):117-25.
21. Karger RA, White WA, Park WC, Rosales AG, McLaren JW, Olson EJ, et al. Prevalence of floppy eyelid syndrome in obstructive sleep apnea-hypopnea syndrome. Ophthalmology. 2006;113(9):1669-74.
22. Ezra DG, Beaconsfield M, Sira M, Bunce C, Wormald R, Collin R. The associations of floppy eyelid syndrome: a case control study. Ophthalmology. 2010;117(4):831-8. Comment in: Ophthalmology. 2010;117(11):2237e1; author reply 2238.
23. Dutton JJ. Surgical management of floppy eyelid syndrome. Am J Ophthalmol. 1985;99(5): 557-60.
24. Bouchard CS. Lateral tarsorraphy for a noncompliant patient with floppy eyelid syndrome. Am J Ophthalmol. 1992;114(3):367-9.
25. Karesh JW, Nirankari VS, Hameroff SB. Eyelid imbrication. An unrecognized cause of chronic ocular irritation. Ophthalmology. 1993;100(6):883-9.
26. Periman LM, Sires BS. Floppy eyelid syndrome: a modified surgical technique. Ophthal Plast Reconstr Surg. 2002;18(5):370-2.
27. Burkat CN, Lemke BN. Acquired lax eyelid syndrome: an unrecognized cause of the chronically irritated eye. Ophthal Plast Reconstr Surg. 2005;21(1):52-8.
28. Valenzuela AA, Sullivan TJ. Medial upper eyelid shortening to correct medial eyelid laxity in floppy eyelid syndrome: a new surgical approach. Ophthal Plast Reconstr Surg. 2005; 21(4):259-63.
29. Ezra DG, Beaconsfield M, Sira M, Bunce C, Shah-Desai S, Verity DH, et al. Long-term outcomes of surgical approaches to the treatment of floppy eyelid syndrome. Ophthalmology. 2010; 117(4):839-46.
 Correspondence address:
Correspondence address:
Angelino Julio Cariello
Rua Botucatu, 820 - São Paulo (SP)
ZIP Code 04023-062
E-mail: [email protected]
Recebido para publicação em 24.11.2009
Última versão recebida em 11.10.2010
Aprovação em 30.10.2010
Study carried out at the Department of Ophthalmology, Federal University of São Paulo - UNIFESP - São Paulo, Brazil.