

Roberto Pinto Coelho1; Jayter Silva Paula2; Rafael Nery e Silva2; Tatiana Vannucci Garcia2; Luiz Fernando Taranta Martin2
DOI: 10.1590/S0004-27492009000100024
ABSTRACT
Creating a continuous curvilinear capsulorhexis in eyes with white intumescent cataracts is a challenge due to the high risk of extension of capsular tears to the lens periphery. Several approaches have been described to avoid this complication and preoperative Nd:YAG laser anterior capsulotomy has been little reported as an optional technique. Eleven patients with white intumescent cataracts were submitted to preoperative Nd:YAG laser anterior capsulotomy. All patients had some degree of cortex falling in anterior chamber after laser application. No patient developed later complications. Thus, preoperative Nd:YAG laser anterior capsulotomy represents a safe and easy option for white intumescent cataracts.
Keywords: Capsulorhexis; Phacoemulsification; Cataract; Laser therapy; Preoperative care; Case reports
RESUMO
A realização da capsulorrexis curvilínea contínua em olhos com catarata branca intumescente é ainda considerada um desafio pelo alto risco de extensão da capsulotomia para a periferia do cristalino. Apesar da descrição de diversas técnicas cirúrgicas voltadas para a prevenção de tal complicação, o uso de Nd:YAG laser no pré-operatório tem raros relatos na literatura internacional. Onze pacientes com cataratas brancas intumescentes foram submetidos a capsulotomia pré-operatória com Nd:YAG laser. Todos os pacientes apresentaram, após a aplicação do laser, a saída de córtex liquefeito para a câmara anterior. Nenhum paciente apresentou complicações cirúrgicas com o procedimento. Desta forma, a capsulotomia anterior com Nd:YAG laser representa uma opção técnica fácil e segura no manejo de cataratas brancas intumescentes.
Descritores: Capsulorrexe; Facoemulsificação; Catarata; Terapia a laser; Cuidados pré-operatórios; Relato de casos
RELATOS DE CASOS
Preoperative Nd:YAG laser anterior capsulotomy in white intumescent cataracts: report of 11 cases
Capsulotomia anterior pré-operatória com Nd:YAG laser em cataratas brancas intumescentes: relato de 11 casos
Roberto Pinto CoelhoI; Jayter Silva PaulaII; Rafael Nery e SilvaIII; Tatiana Vannucci GarciaIV; Luiz Fernando Taranta MartinV
IMédico Assistente do Setor de Catarata do Departamento de Oftalmologia e Otorrinolaringologia da Faculdade de Medicina da Universidade de São Paulo - USP - Ribeirão Preto (SP) - Brasil
IIProfessor Doutor do Departamento de Oftalmologia e Otorrinolaringologia da Faculdade de Medicina da USP - Ribeirão Preto (SP) - Brasil
IIIResidente do Departamento de Oftalmologia e Otorrinolaringologia da Faculdade de Medicina da USP - Ribeirão Preto (SP) - Brasil
IVPós-graduanda do Departamento de Oftalmologia e Otorrinolaringologia da Faculdade de Medicina da USP - Ribeirão Preto (SP) - Brasil
VPós-graduando do Departamento de Oftalmologia e Otorrinolaringologia da Faculdade de Medicina da USP - Ribeirão Preto (SP) - Brasil
ABSTRACT
Creating a continuous curvilinear capsulorhexis in eyes with white intumescent cataracts is a challenge due to the high risk of extension of capsular tears to the lens periphery. Several approaches have been described to avoid this complication and preoperative Nd:YAG laser anterior capsulotomy has been little reported as an optional technique. Eleven patients with white intumescent cataracts were submitted to preoperative Nd:YAG laser anterior capsulotomy. All patients had some degree of cortex falling in anterior chamber after laser application. No patient developed later complications. Thus, preoperative Nd:YAG laser anterior capsulotomy represents a safe and easy option for white intumescent cataracts.
Keywords: Capsulorhexis/methods; Phacoemulsification/methods; Cataract/pathology; Laser therapy/methods; Preoperative care; Case reports [Publication type]
RESUMO
A realização da capsulorrexis curvilínea contínua em olhos com catarata branca intumescente é ainda considerada um desafio pelo alto risco de extensão da capsulotomia para a periferia do cristalino. Apesar da descrição de diversas técnicas cirúrgicas voltadas para a prevenção de tal complicação, o uso de Nd:YAG laser no pré-operatório tem raros relatos na literatura internacional. Onze pacientes com cataratas brancas intumescentes foram submetidos a capsulotomia pré-operatória com Nd:YAG laser. Todos os pacientes apresentaram, após a aplicação do laser, a saída de córtex liquefeito para a câmara anterior. Nenhum paciente apresentou complicações cirúrgicas com o procedimento. Desta forma, a capsulotomia anterior com Nd:YAG laser representa uma opção técnica fácil e segura no manejo de cataratas brancas intumescentes.
Descritores: Capsulorrexe/métodos; Facoemulsificação/métodos; Catarata/patologia; Terapia a laser/métodos; Cuidados pré-operatórios; Relato de casos [Tipo de Publicação]
INTRODUTION
An intact capsulorhexis is crucial to safe and successful phacoemulsification, and facilitates in-the-bag posterior chamber intraocular lens (IOL) implantation(1). Creating a continuous curvilinear capsulorhexis (CCC) in eyes with white intumescent cataracts is a challenge, because of the difficulty to recognize the intumescent cataract and risk of extension of capsular tears to the lens periphery(2-3). Several approaches have been described to avoid this complication(4-12), including preoperative neodymium:YAG (Nd:YAG) laser capsulotomy(13).
The objective of this study was to describe the use of preoperative Nd:YAG laser anterior capsulotomy for phacoemulsification in eyes with white intumescent cataracts in terms of the intraoperative difficulties and postoperative outcomes.
CASE REPORTS
This study comprised 11 eyes of 11 patients with white intumescent cataracts operated upon from January to December, 2007. Patients with any other ocular disease, such as lens-induced uveitis, or glaucoma, or with a history of ocular trauma were excluded.
Preoperative examination included visual acuity, detailed slit-lamp evaluation, applanation tonometry, keratometry, anterior chamber depth (ACD), and ocular axial length (AXL) measurements.
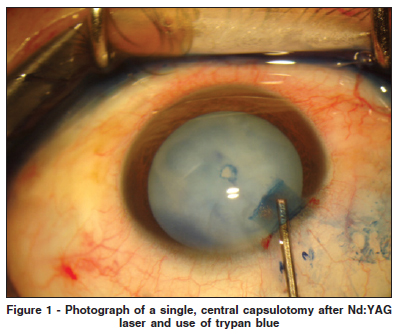
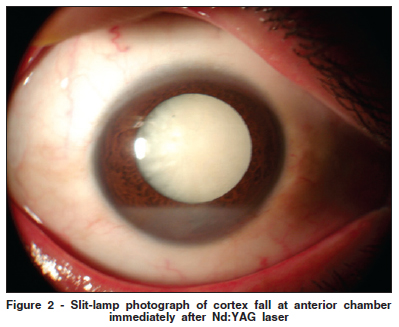
A preoperative opening was performed in the central area of the anterior capsule using the Nd:YAG laser with a single 2.0 mJ laser spot, 10 minutes before surgery (Nd:2300, Alcon Laboratories). This opening could be seen clearly after use of 0.1% trypan blue during surgery (Figure 1). After Nd:YAG laser anterior capsulotomy all eyes developed a visible milky liquefied level in the anterior chamber, and no complication was observed (Figure 2).
All surgeries were performed by the same surgeon (L.F.T.M.) with Stop and Chop technique and peribulbar anesthesia. Briefly, pupils were dilated preoperatively with 1% tropicamide and 2.5% phenylephrine hydrochloride. BSS Plus was employed as the infusion liquid in all eyes. A temporal 2.75 mm clear corneal incision was made and the anterior chamber was filled with 0.1% trypan blue for at least one minute. The anterior chamber was washed with balanced saline solution (BSS) and 2% methylcellulose was injected to deepen it. The side port was done 90 degrees from the incision. Capsulorhexis was completed using a cystotome.
Phacoemulsification with a 0.9 mm, 30 degrees MicroTip (Alcon) was performed with the Legacy 20,000® unit (Alcon Laboratories). In all eyes, a three-piece IOL (AcrySof, Alcon) was implanted in the bag using the Monarch II delivery system. The surgery was concluded with a subconjunctival injection of 20 mg gentamicin sulfate and 2 mg dexamethasone sodium phosphate. Postoperatively, all patients received topical tobramycin 3.0 mg/ml-dexamethasone 1.0 mg/ml (Tobradex®) four times daily for 4 weeks.
Intraoperative findings including mean surgical time, mean effective phaco time and frequency of complications were recorded.
Patients were examined 1 day, 2 and 4 weeks, and 6 months after surgery or as needed. The follow-up visits consisted of a complete ophthalmic examination including slit-lamp examination, tonometry, and fundus examination.
The male:female proportions were 1.75:1 and mean age was 61.9 ± 11.8 years. Follow-up time was 6 months (range: 3-12 months). Mean surgical time, after Nd:YAG laser capsulotomy was 21.2 ± 1.41 min.
The mean values for ACD, AXL and effective phaco time were 3.32 ± 0.17 mm, 23.33 ± 0.25 mm, and 0.80 ± 0.07 s respectively.
Preoperatively all cases varied from light perception to count fingers at 1 m. Postoperative mean corrected visual acuity was 0.85 ± 0.06. Only one patient had incomplete capsulorhexis due anterior fibrosis and, during this study, no patient developed intraocular hypertension or other postoperative complications.
DISCUSSION
The term white cataract does not represent a homogenous group of cases. Both preoperative slit-lamp and echography characteristics, including deep of anterior chamber, A-scan and measurement of the lens, as well as intraoperative particularities like observation of visible milky liquefied cortex after starting the anterior capsulotomy are determinants for the correct diagnosis and define if the white cataract is intumescent(14).
The great challenges of white cataract surgery are how to determine which cataracts are intumescent, with high intracapsular pressure, and how to prevent the extension of capsulotomy to the periphery(10).
For this purpose, Gimbel and Willerscheidt originally suggested the two-stage CCC approach with a small capsulorhexis or a multipuncture of the anterior capsule before capsulotomy(7). After emulsification of the nucleus, the small CCC was enlarged to the desired diameter. With this technique, CCC was achieved in 57 eyes (95%)(11); but other authors reported a 28.3% incidence of incomplete capsulorhexis(12), within a very low success rate in white cataracts with a liquefied cortex (68%) compared to those with a solid cortex(13).
CCC can also be performed in a sealed anterior chamber(8) using a 27 or 30 gauge needle mounted on a 2.5 ml syringe filled with BSS. A successful CCC was achieved in all eyes.
Another report described the successful preoperative use of Nd:YAG laser capsulotomy in the presence of an intact anterior chamber(10).
The use of a single central disruptive pulse of energy may maintain an equal distribution of vector forces, preventing uncontrolled splitting of the anterior capsule to the periphery. We believe that when Nd:YAG laser is done in the presence of an intact anterior chamber, intraocular pressure guarantees safer pressure balance comparing to other techniques.
The presence of a cortex fall at anterior chamber in all Nd:YAG laser capsulotomy cases corroborates the assumption of higher intracapsular pressure than anterior chamber pressure, and this gradient of forces could be a possible risk factor for anterior capsule splitting. It seems clear to us that preoperative Nd:YAG laser anterior capsulotomy represents an easy and useful option for white intumescent cataracts, with a low rate of complications.
REFERENCES
1. Nichamin LD. Prevention and management of complications. Ophthalmol Clin N Am. 1995;8(5):523-8.
2. Bhattacharjee K, Bhattacharjee H, Goswami BJ, Sarma P. Capsulorhexis in intumescent cataract. J Cataract Refract Surg. 1999;25(8):1045-7. Comment in: J Cataract Refract Surg. 2000;26(4):477-8.
3. Vieira E, Alonso RS, Souza Júnior WF, Azevedo MS, Lima VS. Capsulorrexe na catarata leitosa. Rev Bras Oftalmol. 2004;63(3):190-5.
4. Brusini P. Use of air in phacoemulsification of intumescent cataract. J Cataract Refract Surg. 1998;24(7):874-5.
5. Rao SK, Padmanabhan P. Capsulorhexis in white cataracts. J Cataract Refract Surg. 1998;26(4):478-9. Comment in: J Cataract Refract Surg. 1998;24(7):882-4; J Cataract Refract Surg. 1999;25(8):1045-7; J Cataract Refract Surg. 1999;25(8):1157-60.
6. Centurion, V, Lacava, AC, Caballero JC, Modé E. Capsulorrexe em catarata branca. Rev Bras.Oftalmol. 1999;58(7):517-21.
7. Gimbel HV, Willerscheidt AB. What to do with limited view: the intumescent cataract. J Cataract Refract Surg. 1993;19(5):657-61. Comment in: J Cataract Refract Surg. 1994;20(3):365-6.
8. Jacob S, Agarwal A, Agarwal A, Agarwal S, Chowdhary S, Chowdhary R, et al. Trypan blue as an adjunct for safe phacoemulsification in eyes with white cataract. J Cataract Refract Surg. 2002;28(10):1819-25.
9. Marques FF, SoccolI FM, Marques DM, Rehder JR. Impregnação inadvertida da cápsula posterior do cristalino com azul de tripano durante facectomia. Arq Bras Oftalmol. 2006;69(1):111-3.
10. Vasavada A, Singh R, Desai J. Phacoemulsification of white mature cataracts. J Cataract Refract Surg. 1998;24(2):270-7. Comment in: J Cataract Refract Surg. 1998;24(7):874-5.
11. Chan DD, Ng AC, Leung CK, Tse RK. Continuous curvilinear capsulorhexis in intumescent hypermature cataract with liquefied cortex. J Cataract Refract Surg. 2003;29(3):431-4.
12. Hausmann N, Richard G. Investigations on diathermy for anterior capsulotomy. Invest Ophthalmol Vis Sci. 1991;32(7):2155-9.
13. Richards JC, Harrison DC. Preoperative neodymium:YAG anterior capsulotomy in intumescent cataract: preventing extension of the capsular tear to the lens periphery. J Cataract Refract Surg. 2003;29(8):1630-1.
14. Brazitikos PD, Tsinopoulos IT, Papadopoulos NT, Fotiadis K, Stangos NT. Ultrasonographic classification and phacoemulsification of white senile cataracts. Ophthalmology. 1999;106(11):2178-83.
15. Phacoemulsification in eyes with white cataract. Chakrabart A, Singh S, Kushnadas R J Cataract Refract Surg. 2000;26:1041-7. Am J Ophthalmol. 2000; 130(6):864-5.
 Endereço para correspondência:
Endereço para correspondência:
Roberto Pinto Coelho
Departamento de Oftalmologia, Otorrinolaringologia e Cirurgia de Cabeça e Pescoço
Hospital das Clínicas de Ribeirão Preto, Universidade de São Paulo
Av. Bandeirantes, 3.900
Ribeirão Preto (SP) CEP 14049-900
E-mail: [email protected]
Recebido para publicação em 20.04.2008
Última versão recebida em 10.08.2008
Aprovação em 20.08.2008
Trabalho realizado no Departamento de Oftalmologia e Otorrinolaringologia da Faculdade de Medicina de Ribeirão Preto - USP - Ribeirão Preto (SP) - Brasil
Nota Editorial: Depois de concluída a análise do artigo sob sigilo editorial e com a anuência do Dr. José Beniz Neto sobre a divulgação de seu nome como revisor, agradecemos sua participação neste processo.