

Otacílio de Oliveira Maia Júnior1; Danilo Sone Soriano2; Walter Yukihiko Takahashi3; Hisashi Suzuki2
DOI: 10.1590/S0004-27492008000600022
ABSTRACT
The authors describe a patient with macular detachment in the right eye, secondary to congenital pit of the optic disc, submitted to vitrectomy, drainage of the subretinal fluid, perfluorocarbon, endolaser and perfluoropropane gas (C3F8). A sample of the vitreous humor was taken for comparative analysis with the subretinal fluid. Results of retinography, optical coherence tomography, and illustrations of the surgical procedure are presented. Optical coherence tomography revealed the detachment resolved 6 months after surgery. Visual acuity improved from 20/400 to 20/30. This surgical technique can lead to successful reattachment of the macula and improvement of central vision. Additionally, a qualitative and comparative analysis showed a similar biochemical composition of the subretinal fluid and the vitreous. Despite technical limitations, this analysis can confirm the pathophysiology of the disease, suggesting that the subretinal fluid may originate from the vitreous cavity in macular detachment secondary to congenital pit of the optic disc.
Keywords: Optic nerve; Vitreous body; Vitrectomy; Retinal detachment; Retinal detachment; Tomography, optical coherence; Case reports
RESUMO
Os autores descrevem um paciente portador de descolamento macular secundário à fosseta congênita do nervo óptico no olho direito, submetido à vitrectomia, drenagem do fluido sub-retiniano, perfluorcarbono, endolaser e gás perfluoropropano (C3F8). Foi retirada amostra do humor vítreo para análise comparativa com o fluido sub-retiniano. São apresentadas retinografia, tomografia de coerência óptica e ilustrações do procedimento cirúrgico. Após 6 meses da cirurgia, houve resolução do descolamento evidenciada por meio da tomografia de coerência óptica. A acuidade visual melhorou de 20/400 para 20/30. A técnica cirúrgica utilizada pode ter melhorado os resultados obtidos. Adicionalmente, a análise bioquímica qualitativa e comparativa do fluido sub-retiniano e do vítreo mostrou composição semelhante. Apesar das limitações técnicas, esta análise pode corroborar na fisiopatogênese da doença, sugerindo que o fluido sub-retiniano pode ser originado da cavidade vítrea na fosseta congênita de papila.
Descritores: Nervo óptico; Corpo vítreo; Vitrectomia; Descolamento retiniano; Descolamento retiniano; Tomografia de coerência óptica; Relatos de casos
RELATOS DE CASOS
Surgical treatment of macular detachment secondary to congenital pit of the optic disc: case report
Tratamento cirúrgico do descolamento macular secundário à fosseta congênita do disco óptico: relato de caso
Otacílio de Oliveira Maia JúniorI; Danilo Sone SorianoII; Walter Yukihiko TakahashiIII; Hisashi SuzukiIV
IVitreoretinal Specialist at the Department of Ophthalmology, São Rafael Hospital, Monte Tabor Foundation, Salvador (BA) - Brazil
IIVitreoretinal Specialist at the Department of Ophthalmology, Universidade de São Paulo - USP, São Paulo (SP) - Brazil
IIIHead of the Vitreoretinal Service, Department of Ophthalmology - USP, São Paulo (SP) - Brazil
IVAssociate Professor, Department of Ophthalmology - USP, São Paulo (SP) - Brazil
ABSTRACT
The authors describe a patient with macular detachment in the right eye, secondary to congenital pit of the optic disc, submitted to vitrectomy, drainage of the subretinal fluid, perfluorocarbon, endolaser and perfluoropropane gas (C3F8). A sample of the vitreous humor was taken for comparative analysis with the subretinal fluid. Results of retinography, optical coherence tomography, and illustrations of the surgical procedure are presented. Optical coherence tomography revealed the detachment resolved 6 months after surgery. Visual acuity improved from 20/400 to 20/30. This surgical technique can lead to successful reattachment of the macula and improvement of central vision. Additionally, a qualitative and comparative analysis showed a similar biochemical composition of the subretinal fluid and the vitreous. Despite technical limitations, this analysis can confirm the pathophysiology of the disease, suggesting that the subretinal fluid may originate from the vitreous cavity in macular detachment secondary to congenital pit of the optic disc.
Keywords: Optic nerve/abnormalities; Vitreous body/surgery; Vitrectomy/methods; Retinal detachment/etiology; Retinal detachment/therapy; Tomography, optical coherence/methods; Case reports [Publication type]
RESUMO
Os autores descrevem um paciente portador de descolamento macular secundário à fosseta congênita do nervo óptico no olho direito, submetido à vitrectomia, drenagem do fluido sub-retiniano, perfluorcarbono, endolaser e gás perfluoropropano (C3F8). Foi retirada amostra do humor vítreo para análise comparativa com o fluido sub-retiniano. São apresentadas retinografia, tomografia de coerência óptica e ilustrações do procedimento cirúrgico. Após 6 meses da cirurgia, houve resolução do descolamento evidenciada por meio da tomografia de coerência óptica. A acuidade visual melhorou de 20/400 para 20/30. A técnica cirúrgica utilizada pode ter melhorado os resultados obtidos. Adicionalmente, a análise bioquímica qualitativa e comparativa do fluido sub-retiniano e do vítreo mostrou composição semelhante. Apesar das limitações técnicas, esta análise pode corroborar na fisiopatogênese da doença, sugerindo que o fluido sub-retiniano pode ser originado da cavidade vítrea na fosseta congênita de papila.
Descritores: Nervo óptico/anormalidades; Corpo vítreo/cirurgia; Vitrectomia/métodos; Descolamento retiniano/etiologia; Descolamento retiniano/ terapia; Tomografia de coerência óptica/métodos; Relatos de casos [Tipo de publicação]
INTRODUCTION
Congenital pit of the optic nerve head is a rare anomaly first described by Wiethe in 1882(1). Serous macular retinal detachment is associated with 25% to 75% of optic nerve head pits(2-4). Using the cross-sectional retinal imaging provided by optical coherence tomography (OCT), several authors have confirmed the concept of a bilaminar structure with schisis-like retinal changes overlying a more central neurosensory retinal detachment(5-7).
The pathogenesis of the optic disc pit maculopathy is unknown. It has been proposed that the vitreous could be the origin of the subretinal fluid, considering the higher incidence of posterior vitreous detachment in eyes with optic disc pits and retinal detachment(8). The transfer of the dye from the vitreous cavity to the subretinal space has been demonstrated in animal models. However, these studies failed to identify, in the subretinal space, any glycosaminoglycan, an important component of the vitreous(9). Others believe the cerebrospinal fluid should be considered as the source of subretinal fluid in eyes with pits(10-11), although no animal or human model has demonstrated a connection between the pit and the subarachnoid space. Other possibilities would be leakage from the choroid or from vessels within the pit(12).
On the other hand, the management of this entity has also been controversial, since no treatment has clearly proved more advantageous than the others. However, the low incidence of this entity makes it difficult to obtain series large enough to determine the efficacy of the vitrectomy-laser-gas procedure, and other treatment modalities and be able to suggest a procedure of choice.
The objective of this report is to describe an alternative surgical technique for the management of retinal detachment with active internal drainage of subretinal fluid, and to analyze the subretinal fluid in one case of macular detachment secondary to congenital pit of the optic disc, comparing it with the vitreous composition of the patient himself, in order to help understand the pathogenesis of retinal changes.
CASE REPORT
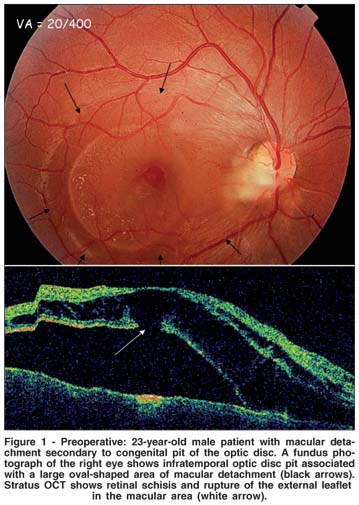
MSC, 23 years old, male, Caucasian, university student, born and raised in São Paulo, was referred to the Emergency Room of the Hospital das Clínicas, University of São Paulo Medical School, for evaluation, due to a decrease in visual acuity of the right eye first noticed 3 months ago. The patient denied other ocular changes. Medical and family history was not significant. Best corrected visual acuity was 20/400 in the right eye and 20/20 in the left eye. Biomicroscopy and intraocular pressure were normal in both eyes. Fundoscopy showed neurosensory detachment in the macular area and inner retinal schisis associated with optic disc pit was found on OCT, showing that the retinal elevation consisted of separation of both the inner and outer layers in the right eye (Figure 1). No changes were observed in the left eye.
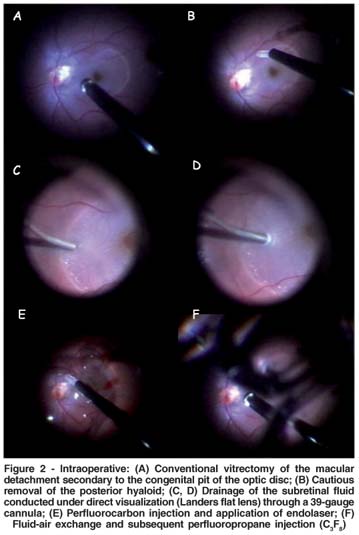
The patient underwent a standard vitrectomy, removal of the posterior hyaloid, with perfluorocarbon, laser photocoagulation, fluid-gas exchange and 12% perfluoropropane (C3F8) injection. The whole procedure was explained to the patient beforehand. The drainage of subretinal fluid was performed under direct visualization (Landers flat lens) through a 39-gauge cannula. In addition, a sample of the vitreous humor was taken for comparative analysis. There were no intercurrent events during the surgical procedure (Figure 2).
The qualitative and comparative analysis of subretinal fluid and vitreous was carried out by the Biochemical and Cerebrospinal Fluid Laboratory of the Hospital das Clínicas. Similar results (pH, hyaluronic acid, glycoproteins, sodium, potassium, bicarbonate, glucose and ascorbic acid) were obtained from both samples.
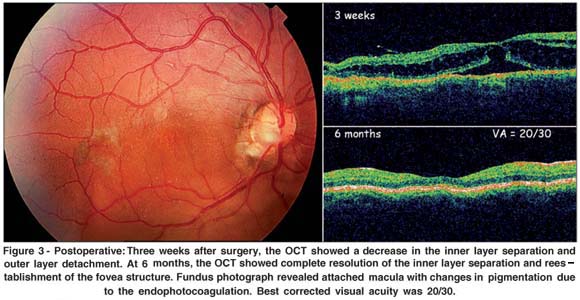
Postoperatively, the patient was asked to remain in a face-down position for three weeks. After 2 months, the macular elevation gradually resolved, and the OCT showed the flattening of the outer layer detachment in the fovea. At the last ophthalmologic evaluation (6 months), an OCT revealed complete resolution of the detachment (Figure 3), and visual acuity was 20/30.
DISCUSSION
There is controversy about the treatment of retinal detachment associated with congenital pit of the optic disc. Treatment modalities such as external laser therapy alone(13), intravitreous gas injection alone(14), laser therapy combined with gas(15), vitrectomy associated with gas tamponade, with or without additional laser treatment(16-17) and scleral buckling(18) have been described in the literature. In this particular case, the best choice was posterior vitrectomy via pars plana, with perfluorocarbon, endophotocoagulation and gas tamponade (C3F8); however, active internal drainage of the subretinal fluid can lead to successful reattachment of the macula and improvement of central vision. Subretinal fluid is eventually absorbed by the retinal pigment epithelium (RPE) and eventually complete apposition of the neurosensory retina with the RPE is achieved. Some retinal detachments are associated with a high volume of subretinal fluid, and its removal can be an important step for the successful surgical procedure. Several factors related to retinal detachment associated with congenital pit of the optic disc are noteworthy. First, good visual recovery is possible even months after the onset of maculopathy(19), and serous macular retinal detachment responds well to early vitrectomy(20).
Macular detachments associated with pits of optic disc occur in young patients, who usually do not have significant vitreous liquefaction, which, in turn, makes less likely the hypothesis that the liquid comes from the vitreous(21). The absence of separation of the posterior vitreous in patients with macular detachment suggests that vitreous traction in this area could play a part in the genesis of the passive movement of fluid to the subretinal space(22-23). The fluid from the pit elevates the layer of nerve fibers, causing internal retinal layers to separate and evolving into serous retinal detachment(24). Spaide et al. published a case that had a rapid improvement in acuity and fundus appearance with the simple introduction of a partial thickness fenestration near the optic disc pit, to redirect the flow of fluid from the retina into the vitreous cavity(25). Yet, there is still no consensus on the pathogenesis of the retinal alterations.
During retinal detachment, subretinal fluid is present, whose composition and pathophysiology are still little known. Subretinal fluid composition varies according to detachment duration; total protein concentration in subretinal fluid increases with time. In addition, all proteins are qualitatively modified. The detached retina loses its oxygen supply, and it then uses the anaerobic pathway to degrade glucose. Thus, long-duration retinal detachments feature increased lactic acid and dextrose concentrations. Phospholipids are also increased in subretinal fluid, reflecting retinal degradation(26). On the other hand, the presence of components derived from hyaluronic acid depolarization is a valid argument in favor of the predominantly vitreous origin of subretinal fluid(26). So, the composition of the subretinal fluid was similar to that of the vitreous humor, suggesting that the origin of the fluid may be the vitreous cavity. The limitation of this result was that, during surgery, the drainage of the subretinal fluid was carried out under direct visualization, drainage being technically impossible after fluid-air exchange that would isolate the subretinal fluid from potential contamination by the vitreous cavity liquid. The amount of subretinal fluid and vitreous was enough to conduct the analysis, and results were similar. However, in our hospital, the test for β-trace protein is not available. This protein is produced by the epithelial cells of the choroid plexus and the leptomeninges, and a highly accurate cerebrospinal fluid marker(27). Despite technical limitations, this analysis can corroborate the pathophysiological mechanism of this disease, suggesting that the subretinal fluid may originate from the vitreous cavity.
The present case showed reestablishment of the anatomic macular structure and significant functional improvement after 6 months of the surgery. OCT helped in monitoring the macular elevation that resolved gradually, with a progressive increase in visual acuity coinciding with the reabsorption of subretinal fluid. The limited recovery of visual function is probably related to its longstanding nature, and to the deposition of exudate on the posterior retinal surface and marked alteration in macular function characteristic of these detachments.
In conclusion, this case report documents the successful reattachment of a serous macular detachment associated with optic disc pit by vitrectomy, active internal drainage of the subretinal fluid, perfluorocarbon, endolaser, and fluid-gas exchange. OCT permitted anatomic assessment of the retina before and after treatment and was useful in the diagnosis and follow-up of this case. Further reports of the management of this uncommon condition are required so that firmer guidelines on treatment can be established.
REFERENCES
1. Wiethe T. Ein Fall von angeborener Difformität der Sehnervenpapille. Arch Augenheilkd. 1881/2;11:14-9.
2. Kranenburg EW. Crater-like holes in the optic disc and central serous retinopathy. Arch Ophthalmol. 1960;64:912-24.
3. Brown GC, Shields JA, Goldberg RE. Congenital pits of the optic nerve head. II. Clinical studies in humans. Ophthalmology. 1980;87(1):51-65.
4. Bonnet M. Serous macular detachment associated with optic nerve pits. Graefes Arch Clin Exp Ophthalmol. 1991;229(6):526-32.
5. Krivoy D, Gentile R, Liebmann JM, Stegman Z, Rosen R, Walsh JB, Ritch R. Imaging congenital optic disc pits and associated maculopathy using optical coherence tomography. Arch Ophthalmol. 1996;114(2):165-70. Erratum in: Arch Ophthalmol. 1996;114(7):840.
6. Lincoff H, Schiff W, Krivoy D, Ritch R. Optic coherence tomography of optic disk pit maculopathy. Am J Ophthalmol. 1996;122(2):264-6.
7. Brasil OF, Brasil MV, Brasil OM. Different presentations of intraretinal fluid collections in optic disc pits: OCT study of 3 cases. Arq Bras Oftalmol. 2006; 69(5):745-7.
8. Sugar HS. An explanation for the acquired macular pathology associated with congenital pits of the optic disc. Am J Ophthalmol. 1964;57:833-5.
9. Brown GC, Shields JA, Patty BE, Goldberg RE. Congenital pits of the optic nerve head. I. Experimental studies in collie dogs. Arch Ophthalmol. 1979; 97(7):1341-4.
10. Regenbogen L, Stein R, Lazar M. Macular and juxtapapillar serous retinal detachment associated with pit of optic disc. Ophthalmologica. 1964;148:247-51.
11. Gass JD. Serous detachment of the macula. Secondary to congenital pit of the optic nervehead. Am J Ophthalmol. 1969;67(6):821-41.
12. Gordon R, Chatfield RK. Pits in the optic disc associated with macular degeneration. Br J Ophthalmol. 1969;53(7):481-9.
13. Tobe T, Nishimura T, Uyama M. Laser photocoagulation for pit-macular syndrome. Ganka Rinshoiho. 1991;85:124-30.
14. Lincoff H, Yannuzzi L, Singerman L, Kreissig I, Fisher Y. Improvement in visual function after displacement of the retinal elevations emanating from optic pits. Arch Ophthalmol. 1993;111(8):1071-9.
15. Rosa AAM, Primiano Júnior HP, Nakashima Y. Retinopexia pneumática e fotocooagulação a laser para tratamento de descolamento secundário à fosseta de disco óptico: relato de caso. Arq Bras Oftalmol. 2006;69(1):101-5.
16. Snead MP, James N, Jacobs PM. Vitrectomy, argon laser, and gas tamponade for serous retinal detachment associated with an optic disc pit: a case report. Br J Ophthalmol. 1991;75(6):381-2.
17. Hirakata A, Okada AA, Hida T. Long-term results of vitrectomy without laser treatment for macular detachment associated with an optic disc pit. Ophthalmology. 2005;112(8):1430-5.
18. Theodossiadis GP. Treatment of maculopathy associated with optic disk pit by sponge explant. Am J Ophthalmol. 1996;121(6):630-7.
19. García-Arumí J, Guraya BC, Espax AB, Castillo VM, Ramsay LS, Motta RM. Optical coherence tomography in optic pit maculopathy managed with vitrectomy-laser-gas. Graefes Arch Clin Exp Ophthalmol. 2004;242(10):819-26.
20. Ghosh YK, Banerjee S, Konstantinidis A, Athanasiadis I, Kirkby GR, Tyagi AK. Surgical management of optic disc pit associated maculopathy. Eur J Ophthalmol. 2008;18(1):142-6.
21. Brodsky MC. Congenital optic disk anomalies. Surv Ophthalmol. 1994;39(2): 89-112. Erratum in: Surv Ophthalmol. 1995;40(2):172. Comment in: Surv Ophthalmol. 1995;40(2):172.
22. Schatz H, McDonald HR. Treatment of sensory retinal detachment associated with optic nerve pit or coloboma. Ophthalmology. 1988;95(2):178-86.
23. Krásnik V, Strmen P, Hasa J, Izáková A, Hrachovcová J. [Surgical treatment of macular hole and maculopathy associated with optic disk pits]. Cesk Slov Oftalmol. 1999;55(5):263-7. Slovak.
24. Lincoff H, Lopez R, Kreissig I, Yannuzzi L, Cox M, Burton T. Retinoschisis associated with optic nerve pits. Arch Ophthalmol. 1988;106(1):61-7.
25. Spaide RF, Fisher Y, Ober M, Stoller G. Surgical hypothesis: inner retinal fenestration as a treatment for optic disc pit maculopathy. Retina. 2006;26(1): 89-91.
26. Quintyn JC, Brasseur G. Subretinal fluid in primary rhegmatogenous retinal detachment: physiopathology and composition. Surv Ophthalmol. 2004;49(1): 96-108.
27. Risch L, Lisec I, Jutzi M, Podvinec M, Landolt H, Huber AR. Rapid, accurate and non-invasive detection of cerebrospinal fluid leakage using combined determination of beta-trace protein in secretion and serum. Clin Chim Acta. 2005;351(1-2):169-76.
 Inquiries to:
Inquiries to:
Otacílio O. Maia Jr
Serviço de Retina e Vítreo, Departamento de Oftalmologia Hospital São Rafael, Fundação Monte Tabor
Av. São Rafael 2142
Salvador (BA) CEP 41253-190
E-mail: [email protected]
Recebido para publicação em 22.05.2007
Última versão recebida em 06.04.2008
Aprovação em 30.04.2008
Study carried out at the Retina and Vitreous Service, Universidade de São Paulo - USP, São Paulo (SP) - Brazil, and São Rafael Hospital, Monte Tabor Foundation, Salvador (BA) - Brazil.