

Luciano Sousa Pereira1; Amy P Wu2; Ganesha Kandavel3; Farnaz Memarzadeh4; Timothy James McCulley5
DOI: 10.1590/S0004-27492008000500020
ABSTRACT
In this report, we describe an unusual patient with a choreiform movement disorder, misdiagnosed as Huntington disease, who later developed dense vitreitis leading to the identification of Treponema pallidum as the underlying pathogen of both abnormalities.
Keywords: Vitreous body; Neurosyphilis; Treponema pallidum; HIV infections; Eye diseases
RESUMO
Neste relato descrevemos um caso infreqüente de um paciente com quadro de distúrbio motor coreiforme diagnosticado equivocadamente como doença de Huntington, o qual posteriormente desenvolveu quadro de intensa vitreíte, possibilitando a identificação do Treponema pallidum como o patógeno causador de ambas anormalidades.
Descritores: Oftalmopatias; Corpo vítreo; Neurosífilis; Treponema pallidum; Infecções por HIV
RELATOS DE CASOS
Vitreitis and movement disorder associated with neurosyphilis and human immunodeficiency virus (HIV) infection: case report
Vitreíte e distúrbio motor associados à neurosífilis e infecção pelo vírus da imunodeficiência humana (HIV): relato de caso
Luciano Sousa PereiraI; Amy P WuII; Ganesha KandavelIII; Farnaz MemarzadehIV; Timothy James McCulleyV
IDepartment of Ophthalmology, Faculdade de Ciências Médicas da Santa Casa de São Paulo, São Paulo (SP) - Brasil. Department of Ophthalmology, University of Califórnia, San Francisco, San Francisco - California (CA) - USA
IIDepartment of Ophthalmology, Stanford University School of Medicine, Stanford - California (CA) - USA
IIIDepartment of Ophthalmology, University of California at Irvine School of Medicine, Irvine - California (CA) - USA
IVDepartment of Ophthalmology, University of California at Irvine School of Medicine, Irvine - California (CA) - USA
VDepartment of Ophthalmology, University of California San Francisco, San Francisco - California (CA) - USA
ABSTRACT
In this report, we describe an unusual patient with a choreiform movement disorder, misdiagnosed as Huntington disease, who later developed dense vitreitis leading to the identification of Treponema pallidum as the underlying pathogen of both abnormalities.
Keywords: Vitreous body/pathology; Neurosyphilis; Treponema pallidum; HIV infections/complications; Oftalmopatias/etiologia
RESUMO
Neste relato descrevemos um caso infreqüente de um paciente com quadro de distúrbio motor coreiforme diagnosticado equivocadamente como doença de Huntington, o qual posteriormente desenvolveu quadro de intensa vitreíte, possibilitando a identificação do Treponema pallidum como o patógeno causador de ambas anormalidades.
Descritores: Corpo vítreo/patologia; Neurosífilis; Treponema pallidum; Infecções por HIV/complicações; Eye diseases/etiology
INTRODUCTION
Syphilis, Treponema pallidum infection, with its numerous presentations has been nicknamed "the great imitator". Potential ophthalmic manifestations are many and can aid in pathogen identification; however, isolated vitreitis has rarely been described(1-3). Although not infrequent, movement disorders are rarely the predominating abnormality in patients with neurosyphilis(4). In this report we describe a unique patient with severe choreiform movement disorder, misdiagnosed as Huntington's disease (HD), who later developed a dense vitreitis leading to the identification of T. pallidum as the underlying pathogen.
CASE REPORT
A 35-year-old male presented with unilateral decreased vision, photophobia and conjunctival injection. He carried the diagnosis of HD for four years based clinically on five-years of progressive writhing bilateral upper extremity movements. Right eye examination demonstrated hand-motion visual acuity, mild anterior segment inflammation and most notably dense vitreitis obscuring retinal visualization. Left eye examination was normal. Bilateral upper extremity choreoathetoid movements with facial grimacing, apraxic/dysarthric speech, and global ataxia were prominent. Neurological examination was otherwise unremarkable.
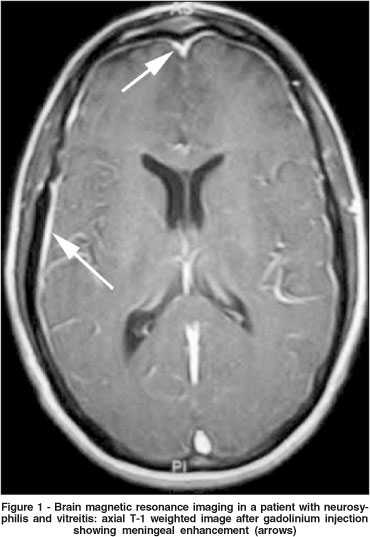
Rapid plasmin reagin - RPR (titer 1:1024) and fluorescent treponemal antibody absorption - FTA-ABS (4+ reactive) were both abnormal. Brain magnetic resonance imaging was significant for meningeal enhancement without focal abnormalities (Figure 1). Cerebral spinal fluid analysis was abnormal: 35 WBCs (100% lymphocytes), protein 57mg/ml, glucose 55mg/ml and positive VDRL (titer 1:4). Additionally, Huntington cytosine-adenosine-guanine (CAG) repeat genetic testing was normal and HIV testing was positive with a CD4 count of 242. Following treatment with intravenous penicillin, a prompt improvement of the vitreitis and chorea was observed.
DISCUSSION
Anterior uveitis is probably the most common ocular finding in secondary syphilis, and many ocular abnormalities can develop in either secondary or tertiary disease such as blepharitis, keratitis, uveitis, chorioretinitis and neuroretinitis(5). This case illustrates two important points: 1) that dense vitreitis can occur as an isolated ocular finding due to T pallidum infection and 2) that this manifestation is seemingly precipitated by concurrent HIV infection. Although syphilis has ophthalmic manifestations in roughly 10% of patients, reports of isolated vitreitis are exceedingly rare(5-6). Kuo et al. reported three patients with isolated syphilitic vitreitis(1). McLeish et al. also reported a patient with dense vitreitis and chorioretinal disease(2). Similar to ours, all three patients reported by Kuo et al. and the patient described by McLeish et al. were HIV positive(2-3). Although admittedly speculative, an HIV altered immune system may result in dense vitreitis with little to no visible retinal abnormalities as opposed to the prominent chorioretinitis, seen more commonly in immunocompetent hosts.
HD is an autosomal dominant disorder of the CNS that becomes symptomatic in adulthood. It is characterized by progressive movement disorder, usually chorea, and psychological disturbances, including cognitive impairment and affective disturbances. When family history is present, the diagnosis is usually straightforward. The main diagnostic problem occurs when the clinical features of HD are present without a positive family history. In those cases, genetic study is warranted. DNA analysis of the father discloses trinucleotide CAG repeats in the intermediate range - greater than in the general population but less than in patients with the disease, that usually present more than 40 CAG repeats(7). In the case presented herein, the misdiagnosis of HD would probably be avoided if a genetic study had been made in the beginning. This would probably anticipate the neurosyphilis diagnosis.
In closing, dense vitreitis occurring in conjunction with "Huntington's disease" or other neurological abnormalities should raise suspicion of syphilis. When encountered, testing for HIV is probably warranted.
REFERENCES
1. Kuo IC, Kapusta MA, Rao NA. Vitritis as the primary manifestation of ocular syphilis in patients with HIV infection. Am J Ophthalmol. 1998;125(3):306-11. Comment in: Am J Ophthalmol. 1998;125(3):374-82. Am J Ophthalmol. 1998;125(3):383-5. Am J Ophthalmol. 1998;125(3):411-5.
2. McLeish WM, Pulido JS, Holland S, Culbertson WW, Winward K. The ocular manifestations of syphilis in human immunodeficiency virus type 1-infected host. Ophthalmology. 1990;97(2):196-203.
3. Schlaegel TF Jr, Kao SF. A review (1970-1980) of 28 presumptive cases of syphilitic uveitis. Am J Ophthalmol. 1982;93(4):412-4.
4. Jones AL, Bouchier IA. A patient with neurosyphilis presenting as chorea. Scott Med J. 1993;38(3):82-4.
5. Woods AC. Syphilis of the eye. Am J Syph Gonorrhea Vener Dis. 1943;27: 133-86.
6. Whitcup SM, Raizman MB. Spirochetal infections and the eye. In: Albert DM, Jakobiec FA, editors. Principles and practice of ophthalmology. 2nd ed. Philidelphia: WB Saunders; 2000. p.4940-55.
7. MacMillan JC, Snell RG, Tyler A, Houlihan GD, Fenton I, Cheadle JP, et al. Molecular analysis and clinical correlations of the Huntington's disease mutation. Lancet. 1993;342(8877):954-8. Comment in: Lancet. 1994;343(8895):487-8.
 Corresponding Author:
Corresponding Author:
Luciano Sousa Pereira
University of California San Francisco
Department of Ophthalmology. 10 Koret Way, K-301 - San Francisco - CA
E-mail: [email protected]
Recebido para publicação em 22.08.2007
Última versão recebida em 15.04.2008
Aprovação em 23.04.2008
Trabalho realizado na University of California, San Francisco - UCSF - USA.
Nota Editorial: Depois de concluída a análise do artigo sob sigilo editorial e com a anuência do Dr. Mário Luiz Ribeiro Monteiro sobre a divulgação de seu nome como revisor, agradecemos sua participação neste processo.