

Miguel Hage Amaro1; Cristina Muccioli2; Mariza Toledo Abreu3
DOI: 10.1590/S0004-27492007000400003
ABSTRACT
PURPOSE: To report some cases of ocular histoplasmosis-like syndrome from a nonendemica area. DESIGN: Observational case series. METHODS: This is a prospective study of 16 eyes from 8 immunocompetent patients evaluated between January 2001 to September 2005. Six patients were female and 2 male aged between 20 to 44 years, average 28 years. All patients presented clinical features that resembled ocular histoplasmosis. All patients had a negative antibody test for histoplasmosis and negative medical and laboratory evaluation of toxoplasmosis, syphilis, and tuberculosis. All patients were submitted to a complete ocular examination including fluorescein angiography. One patient was submitted to indocyanine green angiography. RESULTS: Five patients presented the classical triad of clinical features that include peripapillary scarring, histo spots, choroidal neovascularization, one patient presentd enlargement of atrophic chorioretina scar, one patient presented multiple retinal pigment epithelial detachment, one, neovascularized retinal pigment epithelial detachment. Another patient presented only histo spots. CONCLUSION: These findings of ocular histoplasmosis-like syndrome in patients with negative antibody serum test from a nonendemica area suggest that other agents could cause these similar fundus findings of ocular histoplasmosis.
Keywords: Histoplasmosis; Histoplasma; Histoplasma; Eye infections, fungal; Choroiditis; Fluorescein angiography; Fundus oculi; Choroidal neovascularization; Observational studies
RESUMO
OBJETIVO: Descrevemos os achados clínicos oftalmológicos de 16 olhos de 8 pacientes imunocompetentes que apresentavam características fundoscópicas da síndrome de histoplasmose ocular. MÉTODOS: Os pacientes foram submetidos aos exames oculares de rotina e ainda à fluoresceinografia e à indocianinografia, além de exames laboratoriais para histoplasmome, toxoplasmose, sífilis, síndrome de insuficiência imunológica adquirida, tuberculose. RESULTADOS: Os exames fundoscópicos, fluoresceinográficos e indocianinográficos demonstraram múltiplas coroidites em saca-bocado, atrofia peripapilar e neovascularização de coróide. Os exames laboratoriais foram considerados normais. CONCLUSÃO: Uma outra etiologia que não a histoplasmose pode ser considerada para os achados encontrados. Uma micobactéria atípica ou o Mycobacterium avium que causam lesões semelhantes às descritas nos exames oculares podem ser consideradas.
Descritores: Histoplasmose; Histoplasma; Histoplasma; Infecções oculares fungicas; Coroidite; Angiofluoresceinografia; Fundo de olho; Neovascularização coroidal; Estudos observacionais
ORIGINAL ARTICLE
Ocular histoplasmosis-like syndrome: a report from a nonendemic area
Síndrome de histoplasmose ocular símile: relato de uma área não endêmica
Miguel Hage AmaroI; Cristina MuccioliII; Mariza Toledo AbreuIII
IMD, Eye Institute, Department of Ophthalmology, Universidade Federal de São Paulo - UNIFESP - São Paulo (SP) - Brazil
IIProfessor, Eye Institute, Department of Ophthalmology - UNIFESP - São Paulo (SP) - Brazil
IIIProfessor, Eye Institute, Vice-Coordinator of post graduation, Department of Ophthalmology - UNIFESP - São Paulo (SP) - Brazil
ABSTRACT
PURPOSE: To report some cases of ocular histoplasmosis-like syndrome from a nonendemica area.
DESIGN: Observational case series.
METHODS: This is a prospective study of 16 eyes from 8 immunocompetent patients evaluated between January 2001 to September 2005. Six patients were female and 2 male aged between 20 to 44 years, average 28 years. All patients presented clinical features that resembled ocular histoplasmosis. All patients had a negative antibody test for histoplasmosis and negative medical and laboratory evaluation of toxoplasmosis, syphilis, and tuberculosis. All patients were submitted to a complete ocular examination including fluorescein angiography. One patient was submitted to indocyanine green angiography.
RESULTS: Five patients presented the classical triad of clinical features that include peripapillary scarring, histo spots, choroidal neovascularization, one patient presentd enlargement of atrophic chorioretina scar, one patient presented multiple retinal pigment epithelial detachment, one, neovascularized retinal pigment epithelial detachment. Another patient presented only histo spots.
CONCLUSION: These findings of ocular histoplasmosis-like syndrome in patients with negative antibody serum test from a nonendemica area suggest that other agents could cause these similar fundus findings of ocular histoplasmosis.
Keywords: Histoplasmosis; Histoplasma/isolatin & purification; Eye infections, fungal; Choroiditis; Fluorescein angiography; Fundus oculi; Choroidal neovascularization; Observational studies
RESUMO
OBJETIVO: Descrevemos os achados clínicos oftalmológicos de 16 olhos de 8 pacientes imunocompetentes que apresentavam características fundoscópicas da síndrome de histoplasmose ocular.
MÉTODOS: Os pacientes foram submetidos aos exames oculares de rotina e ainda à fluoresceinografia e à indocianinografia, além de exames laboratoriais para histoplasmome, toxoplasmose, sífilis, síndrome de insuficiência imunológica adquirida, tuberculose.
RESULTADOS: Os exames fundoscópicos, fluoresceinográficos e indocianinográficos demonstraram múltiplas coroidites em saca-bocado, atrofia peripapilar e neovascularização de coróide. Os exames laboratoriais foram considerados normais.
CONCLUSÃO: Uma outra etiologia que não a histoplasmose pode ser considerada para os achados encontrados. Uma micobactéria atípica ou o Mycobacterium avium que causam lesões semelhantes às descritas nos exames oculares podem ser consideradas.
Descritores: Histoplasmose; Histoplasma/isolamento & purificação; Infecções oculares fungicas; Coroidite; Angiofluoresceinografia; Fundo de olho; Neovascularização coroidal; Estudos observacionais
INTRODUCTION
Woods et al.(1) were the first to describe an ocular syndrome consisting of a disciform macular detachment associated with peripheral chorioretinal scars in healthy young adults. Peripapillary scarring was another characteristic added later to the classic triad of the discase(2). Infection with histoplasmosis and the geographic distribution of presumed ocular histoplasmosis syndrome is a suggestive evidence of Histoplasma capsulatum as the etiological agent. The endemic areas include valleys of the Ohio and Mississippi rivers in the United States. In this endemic area about 80 million people are at risk for ocular involvement.
The clinical features of the presumed ocular histoplasmosis syndrome (POHS) include histo spots which are punched-out chorioretinal scars, peripapillary chorioretinal atrophy, and choroidal neovascularization. Curvilinear streaks of chorioretinal scars have also been described(3). POHS affects young healthy adults between the second and fifth decades of life with no gender predilection(4-5). The prevalence rate of disciform scarring in an endemic area is estimated to be 1.2 per 1000 persons(6). Reports of similar clinical features of ocular histoplasmosis from nonendemic parts of the world have been published(7-18).
This study presents a series of patients with clinical features that are similar to POHS and to discuss possible other etiological causes of this clinical symptomatology.
METHODS
This is an institutional prospective study. The protocol of this study was approved by the Medical Ethics Committee of the Federal University of São Paulo (Paulista School of Medicine). In a prospective evaluation 16 eyes from 8 immunocompetent patients who were examined between January 2001 and September 2005. There were six women and two men with average age of 28 years (20 to 44 years old). All patients had clinical features that resembled the POHS. All patients had negative antibody serum test for histoplasmosis and negative medical and laboratory work-up for toxoplasmosis, syphilis and tuberculosis. All patients underwent a complete ocular examination including fluorescein angiography and one patient was also submitted to indocyanine green angiography. Patients were treated when they presented with active choroidal neovascularization. We used diode laser photocoagulation or oral prednisone (1 mg/kg/day) or intraocular injection of steroids (triamcinolone acetonide 4 mg.)
RESULTS
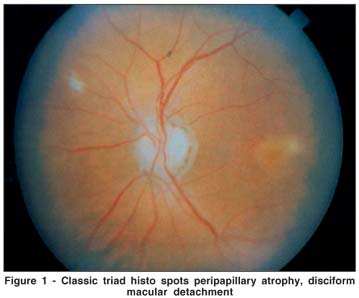
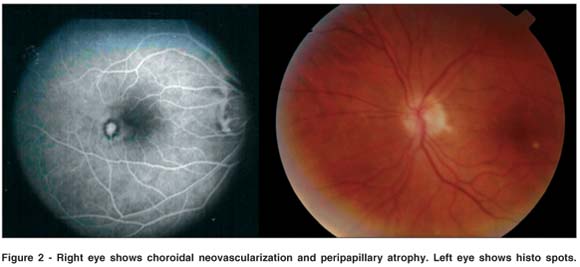
Five of 8 patients presented with the classical triad of clinical features that include peripapillary scarring, histo spots, and choroidal neovascularization (Figures 1 and 2). One patient had an enlargement of an atrophic chorioretinal scar (Figure 3). One patient had multiple RPE detachments (Figure 4). One had a neovacularized RPE detachment and one had only histo spots.

DISCUSSION
Sixteen eyes from eight patients presented similar findings to those observed in ocular histoplasmosis syndrome. These patients had no signs of systemic or laboratory histoplasmosis. We believe that the findings in these patients were not due to histoplasmosis but another etiology should be associated with this clinical presentation. One of these possible agents could include atypical mycobacteria(19). Some authors postulated that atypical mycobacteria or Mycobacterium avium intracellulare could produce a subclinical systemic infection that would cause a choroiditis leaving choroidal scars(19-21).
In conclusion, clinical findings of ocular histoplasmosis were described in non-histoplasmosis patients. Further studies will be required to confirm the other ethiological agents and determine the cause of the clinical features found in this series of patients.
REFERENCES
1. Woods AC, Wahlen HE. The probable role of benign histoplasmosis in the etiology of granulomatous uveitis. Trans Am Ophthalmol Soc.1959;57:318-43.
2. Schlaegel TF, Kenney D. Changes around the optic nervehead in presumed ocular histoplasmosis. Am J Ophthalmol. 1966;62(3):454-8.
3. Fountain JA, Schlaegel TF. Linear streaks of the equator in presumed ocular histoplasmosis syndrome. Arch Ophthalmol. 1981;99(2):246-8.
4. Feman SS, Podgorski SF, Penn MK. Blindness from presumed ocular histoplasmosis in Tennessee. Ophthalmology. 1982;89(12):1295-8.
5. Smith RE, Ganley JP, Knox DL. Presumed ocular histoplasmosis II. Patterns of peripheral and peripapillary scarring in persons with nonmacular disease. Arch Ophthalmol. 1972;87(3):251-7
6. Smith RE, Ganley JP. An epidemiological study of presumed ocular histoplasmosis. Trans Am Ophthalmol Otolaryngol. 1971;75:994-1005.
7. Braunstein RA, Rosen DA, Bird AC. Ocular histoplasmosis syndrome in the United Kingdom. Br J Ophtalmol. 1974;58(11):893-8.
8. Edwards PQ, Billings EL. Worldwide pattern of skin sensitivity to histoplasmin. Am J Trop Med Hyg. 1971;20(2):288-319.
9. Deutman AF. Fluorescein angiography in macular disease. Doc Ophthalmol 1973;197-222.
10. Francois J, De Laey JJ, Dakir M. [Hemorrhagic macular choroidopathy in young subjects (presumed histoplasmosis choroiditis)]. Bull Soc Belge Ophthalmol. 1974;167:664-78. French.
11. Archer DB, Maquiere CJ. Multifocal choroiditis. Trans Ophthalmol Soc UK. 1975;95(1):184-91.
12. Schildberg P, Wessing A. [Focal hemorrhagic chorioditis]. Klin Monatsbl Augenheilkd. 1975;166(5):651-9. German.
13. Notting JG, Deutman AF, van der Werf PJ. [Diagnosis and treatment of macular lesionos in multifocal chorioiditis (presumed histoplasmosis)]. Klin Monatsbl Augenheilkd. 1975;166(5):629-36. German.
14. Flage T, Sand AB, Syrdalen P. Haemorrhagic maculopathy in young adults. Acta Ophthalmol (Copenh). 1977;55(3):489-96.
15. De Lay JJ. Fluoro-angiographic study of the choroid in man. Doc Ophthalmol. 1978;45(1):1-217.
16. Craandijk A Focal macular choroidopathy. Doc Ophthalmol. 1979;48(1):1-99.
17. Saraux H, Pelosse B, Guigui A. [Multifocal inner choroiditis: pseudohistoplasmosis]. The European form of the presumed American histoplasmosis. J Fr Ophthalmol. 1986;9(10):645-51. French.
18. Edwards LB, Acquaviva FA, Livesay VT, Cross FW, Palmer CE. An atlas of sensitivity to tuberculin, PPD-B, and histoplasmin in the United States. Am Rev Respir Dis. 1969;99(4 suppl):1-132.
19. Watzke RC, Klein ML, Wener MH. Histoplasmosis-like choroiditis in a nonendemic area: the northwest United States. Retina. 1998;18(3):204-12.
20. Centers for Disease control and prevention (CDC). Update. Recommendations on prophylaxis and therapy for disseminated mycobacterium avium complex for adults and adolescents infected with human immunodeficiency virus. U.S. Public Health Service Task Force on Prophylaxis and Therapy for Mycobacterium avium Complex. MMWR Recomm Rep. 1993;42(RR 9):14-20.
21. Holland GN, Pepose JS, Pettit TH, Gottlieb MS, Yee RD, Foos RY. Acquired immunodeficiency syndrome: ocular manifestations. Ophthalmology. 1983;90(8):859-73.
 Corresponding Author:
Corresponding Author:
Miguel Hage Amaro
Rua Quintino Bocaiuva, 516
Belém (PA) - CEP 66053-240
E-mail: [email protected]
Recebido para publicação em 29.10.2005
Aprovado em 22.04.2007
Trabalho realizado no Departamento de Oftalmologia da Universidade Federal de São Paulo - UNIFESP.