

Maria Auxiliadora M. Frazão Sibinelli1; Ralph Cohen1; Antônio Murilo Ramalho1; Charles Peter Tilbery3; Jonathan C. Lake1
DOI: 10.1590/S0004-27492000000400009
RESUMO
Objetivo: O objetivo deste trabalho foi estudar a freqüência e características das alterações oculares em pacientes portadores de esclerose múltipla (EM), no estado de São Paulo. Métodos: Durante o período de março de 1996 a novembro de 1998, 64 pacientes, 48 mulheres e 16 homens com idades entre 17 e 59 anos, portadores de EM foram submetidos a exame ocular e exame de campimetria computadorizada. Resultados: Dos 64 pacientes examinados, 44 (68,75%) apresentaram alguma manifestação ocular. A manifestação ocular mais freqüente foi a neurite óptica, acometendo 28 (43,75%) dos pacientes. Em 18 casos (28,1%) foi o primeiro sintoma da doença. Alterações da motilidade extrínseca ocular foram a segunda manifestação mais freqüentemente observadas. A diplopia acometeu 8 pacientes (12,5%) sendo em 6 (9,37%), a primeira manifestação da doença. A paralisia do reto lateral acometeu 2 pacientes (3,1%), sendo o estrabismo convergente o primeiro sinal da doença. Outras alterações observadas foram: uveítes em 4 pacientes (6,25%) e alteração do relevo iriano com pigmentação da cápsula anterior do cristalino em 3 pacientes (4,6%). Nenhum paciente apresentou nistagmo. O defeito de campo visual mais comumente observado nos pacientes que desenvolveram neurite óptica foi escotoma arqueado com defeito paracentral em 46,4% dos pacientes. Dois pacientes (7,1%) apresentaram escotoma central e alterações periféricas. Conclusões: Alterações oculares são freqüentes na EM e muitas vezes são a primeira manifestação clínica da doença. Embora a neurite óptica tenha sido o achado mais freqüente, devemos ressaltar a possibilidade de outras alterações oculares precederem ou acompanharem o curso da doença.
Descritores: Esclerose múltipla; Manifestações oculares; Características
ABSTRACT
Purpose: To study frequency and characteristics of ocular manifestations in patients with multiple sclerosis (MS) in the State of São Paulo. Methods: From March, 1996 to November, 1998, 64 patients (48 female, 16 male, age 17 - 59) with MS underwent ophthalmologic examination and computerized visual field perimeter testing. Results: Forty-four (68.75%) of 64 examined patients presented some kind of ocular manifestation. The most frequent manifestation was optic neuritis (28 patients - 43.75%). It was the first manifestation of MS in 18 (28.1%) patients. Alterations of ocular motility were the second most frequent finding. Eight (12.5%) patients suffered from diplopia, of which 6 (9.37%) presented this as their first manifestation of MS. Sixth nerve palsy occurred in 2 patients (3.1%), with esotropia as a first sign of the disease. Other findings can be listed: uveitis (4 patients - 6.25%), changes in iridian topography with anterior lens capsule pigmentation (3 patients - 4.6%). The most frequent visual field defect in the patients who presented optic neuritis was arcuate scotoma with paracentral defects (46.4%). Two patients presented central scotomas and peripheral changes. None of the patients presented nystagmus. Conclusion: Our data shows that ocular findings in MS are frequent and many times are the initial manifestation of this disease. Although optic neuritis was the most frequent finding, we must emphasize the possibility of other ocular manifestations to be either preceding or occuring at the same time as this disease.
Keywords: Multiple sclerosis; Ocular manifestations; Features
Ocular manifestations in patients with multiple sclerosis in São Paulo
Maria Auxiliadora M. Frazão Sibinelli1, 2
Ralph Cohen3
Antônio Murilo Ramalho1
Charles Peter Tilbery4
Jonathan C. Lake5
INTRODUCTION
Multiple sclerosis (MS) is a chronic inflammatory disease of the central nervous system (CNS) of unknown etiology in which there occurs loss of neurological functions due to an autoimmune demyelinization 1. It is spread throughout the world among Caucasian populations in Europe, Canada, the south of Australia and northern regions of the United States of America; some ethnic groups such as Bantus, Inuit, Mongols and Hungarians present a rare incidence of MS and optic neuritis 2. Frequency varies from 6-14/ 100,000 in southern USA and 30-80/100,000 in northern USA and Canada. Seventy-five percent of the cases involve young adults between 15-50 years. Women are more affected than men with a 1.7/1 ratio. There are no studies of its prevalence in Latin-American countries.
Genetic factors have been associated to development of MS 3,4 due to a significant incidence among family members and a higher frequency of class I (HLA-A and HLA-B) and class II (HLA-D) major histocompatibility complex antigens, which correlate to some ocular manifestations found in this disease 5, 6. Past clinical trials researched antibody titers in cerebrospinal fluid and circulation. Recent development in laboratory techniques has allowed research for a possible viral agent. Other hypotheses suggest an autoimmune process triggered by genetic and environmental factors.
Multiple sclerosis presents several clinical manifestations such as impaired motor and sensory functions, which may be associated to brainstem, cognitive, urogenital, mental, and visual disorders that may alternate periods of remission and exacerbation. Many of the first symptoms in MS are either imperceptible or manifested by sudden low vision, although MS may affect any part of the CNS. Ocular findings in MS include: optic neuritis, retinitis, peripheral vasculitis, ocular motility dysfunction, which is manifested as nystagmus or diplopia, and pars planitis. All of these should be diagnosed by the ophthalmologist. Optic neuritis is the most important condition due to its correlation with MS and high frequency of association with this disease; it occurs many times as the first ocular manifestation.
Visual field defects vary considerably with no typical presentation. Some defects such as arcuate quadrant defects may maintain visual acuity; and other defects such as cecocentral scotoma are found in a minority of patients. Diagnosis is essentially clinical, although MRI, cerebrospinal fluid measurements, and evoked potential studies are often useful for confirmation. Our objective was to study frequency and characteristics of ocular manifestations in MS patients in the city of São Paulo, Brazil, and compare them to other populations.
PATIENTS AND METHODS
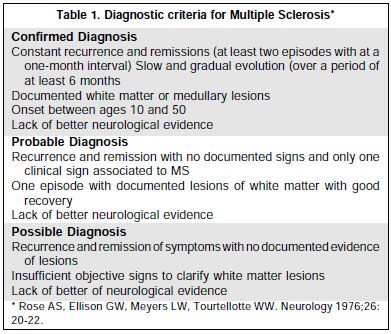
Sixty-four patients with MS from the state of São Paulo, Brazil, were recruited from the CATEM (Multiple Sclerosis Clinical Center) and were followed from March, 1996, to November, 1998. All patients were part of a trial for ß-interferon treatment and all diagnoses had been confirmed after cerebrospinal fluid analysis and evidence of demyelinization in the MRI. Diagnostic criteria for MS are presented on table 1. All patients with other underlying neurologic or systemic diseases with possible ocular manifestations were excluded from this trial. Forty-eight (75%) patients were female and 16 (25%) were male. Ages varied between 17 – 59 years (mean, sd: 34.67 + 8.68). Sixty-three patients (98.46%) were Caucasian and one patient (1.56%) was Afro-Brazilian.
After neurological diagnosis of MS, each patient had his/her history taken and was examined by two ophthalmologists for best corrected visual acuity using Snellen and Jaegar charts as well as ocular motility, pupillary reflexes, slit-lamp examination of the anterior segment and fundus with a 3-mirror Goldmann lens, aplanation tonometry, direct and indirect ophthalmoscopy, computerized visual field testing with the Humphrey 360, using the 24-2 central threshold. All results have been taken from findings in the ocular examinations and history-taking.
RESULTS
Forty-four (68.75%) patients presented some kind of ocular manifestation; 26 (40.6%) patients presented ocular involvement as the first manifestation of MS. Optic neuritis occurred in 28 (43.75%) patients, which represented 63.3% of all patients with ocular involvement. Ages of these patients varied between 17-45 years. Seven patients were male and 21 were female. Four male patients (age 21-32 years) presented bilateral involvement in which one was simultaneous (interval between involvement of both eyes = one week) and in three the interval varied between 6 months and four years. Twenty-four patients presented unilateral eye involvement. Optic neuritis was the first manifestation in 18 cases (28.1%), of which two presented bilateral involvement and two presented other neurologic symptoms. Six cases were diagnosed during the crisis. In the remaining 12 cases intervals between the crisis and its diagnosis varied between 3 months and 12 years (mean, sd - 53.75±45,55), usually at the second or third onset of the crisis. Ocular manifestations in the 10 patients who did not present optic neuritis as the first symptom occurred between 6 months and 13 years after MS diagnosis, 8 of which presented unilateral involvement.
Ninety-five percent of the patients with optic neuritis complained of pain which preceded the disease.
Visual acuity (VA) was 20/20 in 13 of 28 patients who presented optic neuritis on the date of the interview. Visual recovery after the crisis varied from 7 days to 4 weeks and was spontaneous in 11 cases. In 13 patients VA was 20/40 and in 2 patients VA was hand motion (HM). These patients presented afferent pupil defect (APD) and papillary atrophy. All remaining patients presented normal pupillary reflexes.
Ocular motility dysfunctions, diplopia, and palsy of the lateral rectus were the second most frequent ocular findings. Horizontal diplopia was found in 8 patients (12.5%); 6 of these presented it as their first manifestation. Crisis duration varied from 5 days to 2 months (mean 29 days). Diagnosis was immediate in 2 cases. In the remaining cases, intervals between the first onset and diagnosis of MS varied from 5 days to 4 months (mean=86 days). Four cases presented spontaneous remission of the diplopia. Paralysis of the lateral rectus was observed in 2 (3.1%) patients, it was the first manifestation in one of these. In the other patient it appeared 6 months after the first crisis of the disease. The former remained strabic. Nystagmus was not observed in any patient.
Slit-lamp examination of the anterior segment detected ocular inflammation in 4 patients (6.25%). One patient presented anterior granulomatous uveitis; one patient presented pars planitis with a 2+ vitreous cell reaction; one patient presented peripheral vasculitis and 2+ vitreous cell reaction; the remaining patient presented anterior non-granulomatous uveitis with cystoid macular edema. Three patients presented fine iridian pigmented deposits on the lens anterior capsule with a decrease in the number of iridian crypts. There were no signs of inflammatory activity or any signs that might suggest any other ocular disease.
Other findings can be cited: iris nevus (1), temporal corioretinitis scarring (1), unilateral ptosis associated to ambliopia (1). One patient complained of proptosis, which was not confirmed by exophthalmometry. All patients presented normal IOP levels. Visual field defects in 13 (46.4%) patients with VA>20/40 were an arcuate scotoma and a paracentral defect. In the 2 patients with HM VA the visual field showed a central scotoma and peripheral changes. All the remaining patients presented normal visual fields.
DISCUSSION
Multiple Sclerosis in Brazil is presumedly rare, although there are no epidemiologic studies at present. Studies of ocular manifestations in MS are not common in Latin-American countries, and they are limited to neuroophthalmological findings such as optic neuritis 8, 9. We were able to study 64 patients due to our involvement with a multidisciplinary study of MS.
As in other trials, the female proportion was higher in comparison to the male with a 3:1 ratio; the age group in our study ranged between 17 and 59 years. Most of the subjects were Caucasian.
Optic neuritis was the most frequent ocular manifestation in our study, and in 28.1% of these patients it was their first manifestation of MS, which shows a higher risk of a patient with optic neuritis to develop MS. According to the literature, the age group of patients who develop optic neuritis varies from 15 to 45 years with a female:male ratio of 3:1. In our study the age group varied from 17 to 45 years with a higher prevalence in the fourth decade age group; our female:male ratio was exactly 3:1. Peixoto et al 8, in a trial of 88 patients with idiopathic optic neuritis (ION), reported that 9 patients developed MS after a period that varied from one month to 5 years (mean 26 months). Alvarez et al 9, in a similar trial, reported that one in 23 patients with ION developed MS in a mean period of 9.7 years. In our study, the interval for the 18 patients who presented ION varied between 3 months and 12 years (mean 50 months). This reinforces the need for a constant follow-up consisting of ophthalmologic investigations of patients presenting neuritis, since a longer follow-up might show more manifestations of MS. A prospective trial of 84 patients with ION in Japan 10 showed a conversion rate of 8.3% during a 5.2 year follow-up. This is similar to what has been published in Brazil and other oriental countries such as: China 11, India 12, and Korea 13, where the prevalence of MS is low and a higher rate of visual symptoms in the beginning of the disease occur along with an involvement of the optic nerve. Environmental and genetic factors influence the prevalence of MS 8. It may be possible that Latin-American and Asian countries share common factors that influence the diseases manifestation and the progression of ION.
Ocular pain was a complaint of 95% of our patients who presented optic neuritis, which is similar to what is found in literature. Although recurrence and bilateral involvement are considered risk factors for MS by some authors, our data does not support this theory, since only one patient that developed MS presented recurrent optic neuritis.
Internuclear oculoplegia is the most common disorder of motility and diplopia in MS, ocurring in approximately 53% of the cases 14. In our study, diplopia was the second most common manifestation (12.5%). This may be due to the fact that the follow-up period for our patients was shorter; since we will continue to observe these patients, this manifestation may appear more frequently in later phases. It is important to note that in 6 patients of 8 diplopia was the first ocular manifestation, which can be used as an alert to the ophthalmologist that diplopia may be an early sign for MS.
Although MS is not a common cause of cranial nerve palsies, the frequency of sixth nerve palsy increases in younger patients 15. Two of our patients (3.1%) presented sixth nerve palsy; their ages were 28 and 39 years, and the latter presented an untreatable palsy - in this case strabismus was the first sign of MS.
Nistagmus has been reported in more than 67% of the patients with MS; we did not observe any patients who presented nystagmus.
Several reports associate MS to uveitis and retinal vasculitis, with frequencies that varied from 2.4 to 27% 16-20. These differences are probably due to the different populations, examination techniques, and diagnostic criteria. Intermediate uveitis is the most common form of inflammation, with the pars planitis inflammation varying from mild to severe. Anterior granulomatous or nongranulomatous uveitis also has been described. Most cases present a moderate uveitis that did not present cystoid macular edema and, therefore, did not require treatment. Two of the patients that presented intraocular inflammation presented an intermediate uveitis without macular edema. One of these patients presented peripheral retinal vasculitis. Both patients visual acuity was 20/30 and they were treated. The remaining two patients presented anterior uveitis, of which one case was granulomatous and the other was non-granulomatous with cystoid macular edema. This patient complained of a similar episode one year before diagnosis of MS, which could have been the first possible sign of MS. All patients with diagnosis of uveitis underwent clinical and laboratorial investigation for other probable causes of uveitis; since none were found, an association with MS becomes more likely. Two recent reports 19 document uveitis as an important finding prior to neurological symptoms and diagnosis of MS. Associations between intraocular inflammation activity and MS exacerbation are not well established; however, many authors have noticed a more frequent association between uveitis and a more active CNS disease. The four patients who presented uveitis did not show any manifestations of MS at the moment of examination.
All remaining findings such as iris nevus, corioretinitis scarring, and ptosis were considered unrelated to the disease. Although nothing was found in literature, three of our patients did show changes in iris topography with mild to moderate anterior capsule pigmentation. Visual field defects in this kind of patient present many variations, with no established pattern. Cecocentral scotoma is an infrequent finding, and only two of our patients presented this pattern in the visual field. A large trial reported in 1991, the Optic Neuritis Trial 7, found a diffuse visual field defect in 44.8% of their cases and focal defects in 55,12%, although they were not necessarily central defects. Arcuate scotoma with paracentral defects were the most common finding (46.4%) in our study among patients with optic neuritis.
CONCLUSION
Our data show that ocular findings in MS are frequent and many times are the initial manifestation of this disease. Although optic neuritis was the most frequent finding, we must emphasize the possibility of other ocular manifestations to be either preceding or occuring at the same time as this disease.
REFERENCES
1. Whitaker JN, Mitchell GW. Clinical Features of Multiple Sclerosis.In: Raine C, McFarland HF, Tourtellotte WW. Multiple Sclerosis: Clinical and pathogenetic basis.London, Chapman and Hall 1997.
2. Sergott RC, Beck WR, Lisak PR et al. Multiple Sclerosis. In: Pepose JS, HollandGN, Wilhelmus KR: Ocular Infection and Immunity. Baltimore. Mosby,1996.
3. Haegert DG, Marrossu MG. Genetic susceptibility to Multiple Sclerosis. Ann Neurol 1994;36(suppl 2):206-10.
4. Sadovinick AD. Genetic epidemiology of Multiple Sclerosis. A Survey. Ann Neurol 1994;36(suppl 2):194-203.
5. Ests ML, Rudick NA, Barnett GH et al. Stereotactic biopsy of an active multiple sclerosis lesion. Arch Neurol 1990;47:1299-303.
6. Malinovisky SM, Pulido JS, Goeken NE et al. The Association of HLA B8, B51, DR2 and Multiple Sclerosis in Pars Planitis. Ophthalmol 1993;100(8):1199-205.
7. Keltner J, Spurr J. Quality Control Functions of the visual field reading center for the optic neuritis treatment trial. In : Ophthalmology Clinics of North America. Philadelphia. W B Saunders Company, 1992.
8. Lana-Peixoto MA, Lana-Peixoto M. The Risk of Multiple Sclerosis Developing in Patients with Isolated Idiopathic Optic Neuritis in Brazil. Arq Neuro Psiquiat 1991;49(4):377-83.
9. Alvarez G, Cardenas M. Multiple Sclerosis following optic neuritis in Chile. J neurol Neurosurg Psichiat 1989;52:115.
10. Isayama Y, Takahashi T, Shimoyoma et al. Acute optic neuritis and multiple sclerosis. Neurology 1982;32:73.
11. Baoxum Z, Xiuqin L, Yupu G it al. Muliple Sclerosis: a clinical study of 70 cases. Clin Med J 1980;93:260.
12. Chopra JS, Radhakrishnan K, Sawhney BB et al. Multiple Sclerosis in North West India. Acta Neurol Scand 1980;62:312.
13. Kurtze JF, Park CS, Oh SJ. Multiple sclerosis in Korea: clinical features and prevalence. J Neurol Sci 1968;6:462.
14. Rullen JPH, Sanders EACM, Hogenheis LAH. Eye Movement Disorders in Multiple Sclerosis and Optic Neuritis. Brain 1983;106:121-40.
15. Rush JA, Yonge BR. Paralysis of cranial nerves III, IV and VI: causes and prognosis in 1000 cases. Arch Ophthalmol 1981;99:77-9.
16. Warner J, Lessel S. Neuro Ophthalmology of Multiple Sclerosis.Clin Neurosc 1994;2(3-4):180-8.
17. Arnold AC, Pepose JS, Helpler RS et al. Retinal periphlebitis and retinitis in multiple sclerosis: Pathologic Characteristics. Ophthalmology 1984;91:255-62.
18. Kenison JB, Flynn T, Green WR. Retinal pathologic changes in Multiple Sclerosis. Retina 1994;14:445-51.
19. Lim JI, Tessler HH, Goodwin JA. Anterior granulomatous uveitis in patients with multiple sclerosis. Ophthalmol 1991;98:142-5.
20. Palimeris G, Marcomichelakis N, Konstantinidou V et al. Intermediate uveitis what is the natural course of the disease and its relationship with other systemic disease? Eur J Ophthalmol 1994;4(4):223-7.
This study was carried out at the Department of Ophthalmology, Santa Casa de São Paulo.
Presented as Free Communication at the Brazilian Congress of Ophthalmology in Recife and at the Panamerican Congress of Ophthalmology and AAO in Orlando, FL, 1999.
1 Assistant Physician of
the Department of Ophthalmology, Santa Casa de São Paulo.
2 Postgraduate Student, PhD, University of São
Paulo.
3 Diretctor of the Department of Ophthalmology,
Santa Casa de São Paulo
4 Assistant of the Department of Neurology, Santa
Casa de São Paulo
5 Intern of the Department of Ophthalmology,
Satna Casa de São Paulo.
Correspondence: Maria Auxiliadora M. Frazão Sibinelli. R. Dr. Guilherme Cristoffel, 250/191. São Paulo (SP) Brasil. CEP 02406-010. E-mail: [email protected]