

Manuel José Justiniano1; Juan José Mura2; Jair Giampani Junior3; Marcelo Jordão Lopes Silva4; Guillermo Barreto Fong5
DOI: 10.5935/0004-2749.2025-0109
ABSTRACT
PURPOSE: To evaluate the preferred surgical practice patterns for glaucoma among members of the Latin American Glaucoma Society.
METHODS: A cross-sectional study was conducted using an electronic survey distributed in July 2023 via email to members of the Latin American Glaucoma Society. The questionnaire comprised four sections addressing the specialists' profiles, preferred surgical procedures for open-angle glaucoma, and choices in 10 different clinical scenarios, including congenital glaucoma.
RESULTS: Of the 63 members, 49 physicians (77.7%) responded – 13 women and 36 men – from nine Latin American countries. Thirty-one respondents (63.26%) had more than 20 yr of professional experience. For the surgical management of open-angle glaucoma, trabeculectomy was the most preferred procedure (48 physicians), followed closely by glaucoma drainage devices (47 physicians) and minimally invasive glaucoma surgery (29 physicians). Across the 10 clinical scenarios, glaucoma drainage devices were selected most frequently (203 preferences), followed by trabeculectomy (118), ciliary body laser procedures (107), and minimally invasive glaucoma surgery (40). However, minimally invasive glaucoma surgery was the preferred option for primary open-angle glaucoma with mild-to-moderate cataracts.
CONCLUSION: Among specialists of the Latin American Glaucoma Society, trabeculectomy and glaucoma drainage devices remain the most commonly performed surgical procedures. Minimally invasive glaucoma surgery is primarily used in combination with cataract surgery, while ciliary body laser procedures are generally reserved for cases of previous glaucoma drainage device failure or as an initial option for newly diagnosed glaucoma cases.
Keywords: Glaucoma; Ophthalmologic surgical procedures; Latin America; Practice patterns, physicians; Surveys and questionnaires
INTRODUCTION
A physician's practice is shaped by multiple factors, including academic education, personal attributes, and broader life experiences. Clinical guidelines and medical consensus documents, prepared by experts and endorsed by academic institutions, also play a crucial role in standardizing medical practice. This structured approach to knowledge dissemination has gained prominence since the 1990s, aligning with the evolution of evidence-based medicine, which emphasizes empirical evidence over anecdotal experience and opinion(1).
In the field of glaucoma, for example, the American Academy of Ophthalmology regularly reviews and updates its practice guidelines every 5 yr(2).
The Latin American Glaucoma Society (SLAG), established in 1998, functions as a scientific and academic platform that brings together leading subspecialists from across the region. Its mission is to assess various aspects of glaucoma management, taking into account the demographic, socioeconomic, cultural, and ethnic characteristics of the population as well as the healthcare limitations faced in certain countries. Despite having advanced scientific knowledge, practitioners in the region may encounter challenges in translating evidence-based medicine into routine clinical practice(3).
Over the past decade, there has been a significant expansion in surgical options for glaucoma treatment, driven by the introduction of new techniques and a wide range of medical devices(4–8). This diversity allows for more individualized treatment planning, enabling clinicians to select the most appropriate procedure for each patient. However, the rapid proliferation of new technologies and techniques can also lead to differences of opinion or controversy regarding their main indications, risks, and benefits. Moreover, beyond clinical considerations, socioeconomic and regulatory factors unique to each country can affect the validation, adoption, and utilization of novel surgical devices. Such factors may include importation delays, approval processes by health agencies with competing priorities, and complex post-market surveillance regulations(9–12). Therefore, the present study aims to identify and analyze the preferred surgical practices among glaucoma specialists who are members of SLAG, focusing on the procedures they most commonly perform.
METHODS
A cross-sectional, survey-based study was conducted following evaluation and approval by the SLAG Scientific Committee. All participating physicians complied with the principles of the Declaration of Helsinki, and participant data were handled with strict confidentiality.
In July 2023, an email invitation was sent to the 63 SLAG members, all of whom are glaucoma subspecialists, inviting them to participate in the survey. The questionnaire was created using the Jotform platform (San Francisco, CA). The collected data were securely stored by a SLAG Scientific Committee member (M.J.J.) and subsequently transferred to an external and independent data processing service (ROMAT Creator Center). This procedure was designed to minimize potential bias in data handling, as no SLAG member was involved in processing the survey results. The authors were responsible for reviewing and interpreting the final data.
The questionnaire comprised four sections. The first section collected information on each specialist's professional profile, including years of experience, practice setting, and the proportion of patients with open-angle versus angle-closure glaucoma (ACG). The second section explored surgical management preferences for primary open-angle glaucoma (OAG). The third section presented 10 clinical scenarios, such as neovascular glaucoma, uveitis-associated glaucoma, and combined phacoemulsification with glaucoma procedures, to assess preferred practices in each situation. The fourth section focused on congenital glaucoma and its surgical management. Finally, participants were invited to suggest research topics of interest to SLAG.
The processed data were analyzed using descriptive statistics. The complete dataset and individual responses to all questionnaire items are available from the corresponding author upon request.
RESULTS
Of the 63 SLAG members, 49 physicians (77.7%) responded to the survey, comprising 13 women (26.5%) and 36 men (73.5%) from nine countries. Sixteen respondents were from Brazil, eight from Argentina, seven each from Mexico and Colombia, four from Peru, two each from Bolivia, Chile, and Ecuador, and one from Venezuela.
Regarding the demographic profile and professional experience of the participating glaucomatologists, most had more than 20 yr of experience (31 physicians; 63.3%), while 15 had between 10 and 20 yr (30.6%). Two had between 5 and 10 yr (4.1%), and one had less than 5 yr (2%). Concerning their professional environment, all 49 participants reported involvement in private practice, dedicating between 50% and 100% of their time to it. Additionally, 31 participants (63.2%) reported working in public healthcare institutions, allocating 10%–33% of their professional time to these settings. Forty-two participants (85.7%) were also active in university environments, dedicating 10%–50% of their professional time to academic activities.
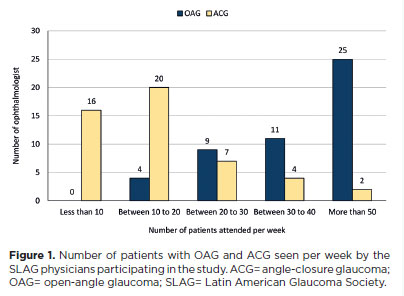
With respect to research involvement in glaucoma, 16 physicians (32.6%) reported exclusive participation in surgical research, 13 (26.5%) in clinical research, and 20 (40.9%) in both clinical and surgical research. When asked about the most frequently encountered type of glaucoma, most physicians indicated that they see more patients with OAG than with ACG every week (Figure 1).
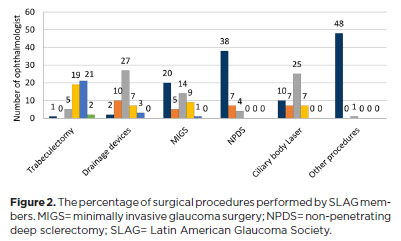
Regarding preferred practices for OAG cases, Figure 2 presents the surgical procedure options and the percentage preferences among SLAG physicians. Trabeculectomy was the most frequently performed procedure, with only one physician not utilizing it. Aqueous humor drainage devices were the second most common, not used by only two respondents. Approximately 20 out of 49 physicians did not employ minimally invasive glaucoma surgery (MIGS), whereas 59.1% did. The least performed procedure was non-penetrating deep sclerectomy (NPDS), carried out by 11 physicians (seven performed NPDS in <10% of cases and four in 10%–24% of cases). Cyclophotocoagulation was also reported as a frequently used procedure.
Trabeculectomy
When asked about the use of wound-healing modulators in trabeculectomy, all respondents reported using mitomycin C (MMC) – 29 physicians by injection and 20 subconjunctivally. Among the 48 physicians performing trabeculectomy, 35 occasionally used 5-fluorouracil, eight used Ologen, and five administered bevacizumab.
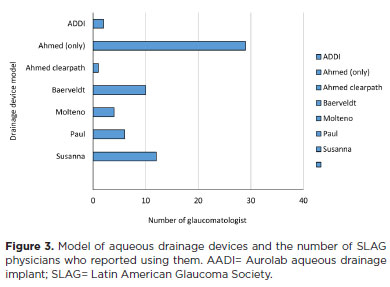
Drainage devices
Among the 47 physicians utilizing glaucoma drainage devices (GDDs), the majority reported using the Ahmed device in addition to other implants (Figure 3). The Susanna device was the second most frequently chosen, used by 12 participants. Regarding the use of MMC during GDD implantation, eight physicians reported using it, while 39 did not.
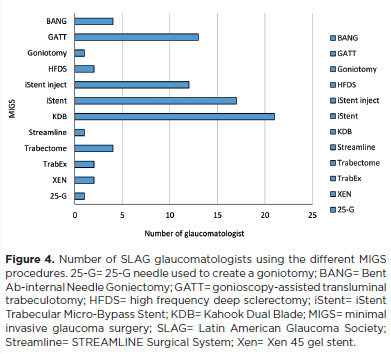
Minimally invasive glaucoma surgery
Of the 29 glaucomatologists who reported performing MIGS, 27 indicated that they routinely used more than one MIGS technique. Figure 4 illustrates the various MIGS procedures preferred by SLAG members, with the Kahook Dual Blade (KDB; New World Medical Inc., Rancho Cucamonga, CA, USA) being the most frequently performed, followed by the iStent (iStent Trabecular Micro-Bypass Stent; Glaukos Corp., Laguna Hills, CA, USA).
Non-surgical treatment of glaucoma: selective laser trabeculoplasty (SLT) versus medical therapy
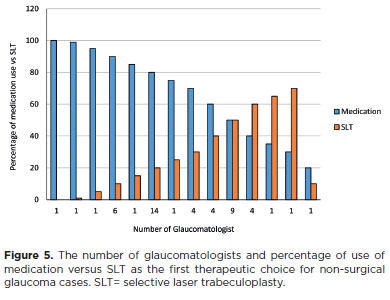
When asked about their primary therapeutic approach for non-surgical patients, 33 physicians (using medication in 60%–100% of cases) preferred initiating treatment with topical medication (Figure 5). Nine physicians used medication and SLT equally in about 50% of cases, while only six physicians preferred SLT as the initial treatment option.
Clinical scenarios
Responses regarding the 10 clinical scenarios are summarized in table 1. GDD implantation was most commonly preferred in cases with previous failed trabeculectomy and after extracapsular or intracapsular cataract surgery. For eyes with previous uncomplicated phacoemulsification, trabeculectomy was the preferred procedure, followed by MIGS. In cases with previous keratoplasty, scleral buckle, or pars plana vitrectomy, drainage implants were favored. Similarly, GDDs were the preferred approach for patients with prior uveitis or neovascular glaucoma. Laser procedures were chosen mainly for cases with failed drainage devices. Most physicians preferred combined cataract surgery and MIGS for patients with OAG and mild-to-moderate cataracts. Overall, GDDs were the most commonly selected procedure, followed by trabeculectomy and ciliary body laser, as shown in figure 2.
Childhood glaucoma
Thirty-six participants (69.4%) reported managing pediatric glaucoma cases, including congenital glaucoma. Regarding surgical management, 21 physicians indicated that they performed only trabeculectomies, nine performed both trabeculectomies and trabeculotomies, two reported using drainage devices, five occasionally performed goniotomy, four performed gonioscopy-assisted transluminal trabeculotomy, and one physician reported using ciliary body laser treatment in congenital glaucoma cases.
Research proposals from SLAG members
In the final, optional question, physicians were invited to propose topics or areas of interest for future SLAG research. Nine members did not respond, and seven expressed general interest in research without specifying topics. The remaining 33 glaucomatologists suggested various subjects. In non-surgical research, interest focused on imaging in glaucoma, diagnostic and follow-up strategies, epidemiological studies, telemedicine, and artificial intelligence. Regarding surgical research, ciliary body laser procedures were the most frequently suggested topic, followed by MIGS. Several members also expressed interest in studies assessing cost-effectiveness.
DISCUSSION
The SLAG was founded to represent the scientific perspectives of ophthalmologists across the region – from Mexico to the southernmost areas of South America. Its mission involves a continuous intellectual and scientific effort to examine the characteristics of the Latin American population and compare them with scientific evidence from other regions. Although the principles of the scientific method and evidence-based medicine are universal, there remains a need for contextual adaptation of medical practices – a process often referred to as the tropicalization of medicine(13). This approach requires particular attention to the unique needs of each country and region.
In this way, regional medical situations are analyzed and compared with findings from other parts of the world, based on literature reviews that prioritize levels of evidence and existing consensus(14). One previous study compared the level of consensus in the management of primary OAG between the United States and Latin America. Although agreement was high – 111 out of 148 statements (75%) – certain areas of controversy related to diagnosis and treatment were identified. This highlights that even when clinical cases appear similar worldwide, management may vary considerably due to local variables such as resource availability (human, material, and economic), geographical conditions, lifestyle, nutrition, and genetic factors.
Between 2009 and 2010, and again in 2013, a study was conducted to assess the level of consensus among glaucoma specialists in Latin America regarding specific aspects of diagnosis and medical management(15). Forty-eight physicians from 11 Latin American countries, along with two from the United States and Puerto Rico, participated. Similar to the present study, an electronic questionnaire was used, and the participant demographics were comparable, including 31 SLAG members and 19 non-members. A key distinction, however, is that the present study focuses on surgical procedures – many of which were either unavailable or rarely used in Latin America 15 yr ago.
When comparing our results with those from other regions, the American Glaucoma Society (AGS) published a similar report in 2017, based on an electronic survey conducted among its members in 2016(16). Like our study, it explored surgical practices and included comparable questions. The AGS also compared its 2016 data with results from earlier surveys (1996, 2002, and 2008) to identify temporal trends. The AGS survey achieved a participation rate of 23% (251 out of 1,091 members). In their sample, 33% of respondents had more than 20 yr of experience, while 29% had less than 5 yr.
In our study, most participants had over 20 yr of experience in the specialty (63.3%), while a considerable proportion had between 10 and 20 yr (30.6%). Only one participant reported less than 5 yr of experience (2%). Before analyzing and comparing the other results between the two studies, it is important to note that this difference in experience levels among the two groups of glaucomatologists may be relevant, as it could have influenced their responses.
A notable difference between both studies relates to surgical choices. In the AGS survey(16), drainage devices were preferred over trabeculectomy – opposite to our findings – with the Baerveldt implant being the most commonly used device. In contrast, SLAG members reported more frequent use of the Ahmed device. Regarding MIGS, AGS specialists most commonly used the iStent, while in our study, the KDB ranked first, followed by the iStent – a device unavailable at the time of the 2016 AGS survey.
In Japan, the Glaucoma Specialists Society conducted a similar survey in 2019, comparing responses with data from 2009 and 2014(17). Fifty glaucomatologists participated, six of whom did not perform surgery. Among the remaining 44 respondents, trabeculectomy remained the most commonly performed procedure, though its frequency had declined over time, corresponding with increased use of drainage devices – mainly the Ahmed and Baerveldt implants.
A comparable study in India, conducted during the 2013 national glaucoma congress, surveyed 146 specialists through 35 questions covering diagnostic and therapeutic practices(18). Among participants, 33% had over 15 yr of experience, and 18.4% had less than 5 yr. Trabeculectomy emerged as the most frequently performed surgery, consistent with our findings. The use of MMC was reported as the most common adjunct, while only one-third of respondents utilized drainage devices.
When deciding on initial treatment – whether SLT or medication – most physicians preferred pharmacologic therapy. However, the 6-yr results of the LIGHT study demonstrated that initiating treatment with SLT provides superior long-term intraocular pressure control and reduces the need for incisional surgery(19). This discrepancy between evidence-based recommendations and clinical practice reinforces the importance of studies like ours and exemplifies the concept of "tropicalization of medicine". Although SLT has been shown to be more cost-effective than medication in other regions(20,21), its limited use in Latin America may stem from barriers such as accessibility, healthcare system organization, and economic disparities. Furthermore, our survey did not explore whether physicians discussed SLT as an alternative with their patients – an aspect worth investigating in future studies(20,21).
With respect to MIGS procedures, our results align with international clinical guidelines regarding indications and applications(22,23). Notably, the higher frequency of MIGS use in our study was associated with its combination with cataract surgery. This finding concurs with evidence from a systematic review demonstrating the efficacy of MIGS in mild-to-moderate glaucoma cases(24). In that review, the iStent was the most frequently used device, whereas in our study, the KDB ranked first, followed by the iStent.
The final, optional question on research interests revealed several key areas of potential investigation. These suggestions highlight unmet research needs and may guide future studies. They also offer valuable insights for both the scientific community and the ophthalmic industry, reflecting current priorities and expectations. Particular emphasis was placed on cost-effectiveness studies, given the substantial economic variability across Latin American countries and its influence on clinical decision-making.
Identifying preferred practice patterns within a specific population, when conducted systematically, generates valuable insights and provides a foundation for longitudinal analyses of evolving trends. This approach has been effectively implemented by the American Academy of Ophthalmology across various subspecialties, including glaucoma(25). In the present study, our goal was to determine the preferences of glaucoma specialists in Latin America, who serve as academic leaders and mentors in their respective regions. Nevertheless, certain considerations apply to our sample. Due to their level of expertise and academic involvement, respondents may have introduced positive bias, as they represent a highly experienced subgroup of practitioners. Although our sample size may appear limited, the responses of 49 ophthalmologists from nine countries represent approximately 80% of SLAG members. While our findings cannot be generalized to all Latin American glaucoma specialists, they provide a valuable initial reference point for future research.
Despite these limitations, our study presents several strengths. It reflects real-world practice patterns as reported by leading experts and offers essential insights into the frequency, selection, and rationale behind various surgical and laser procedures. Ultimately, we hope this study contributes to the ongoing improvement of glaucoma care in the region and serves as a foundation for future comparative studies, both within Latin America and globally.
In conclusion, SLAG specialists demonstrated a preference for trabeculectomy in the surgical management of OAG and for GDDs in specific cases. MIGS procedures were primarily reserved for combination with cataract surgery. Additionally, ciliary body laser treatment was preferred in cases of failed drainage device surgery and may also be considered a potential first-line surgical option for newly diagnosed glaucoma cases.
ACKNOWLEDGMENTS
We would like to acknowledge Rodrigo M. Torres from ROMAT Creator Center for his scientific guidance.
We also extend our gratitude to all the SLAG members who participated by responding to the survey in the present study. Argentina: Arturo Burchakchi, Javier Casiraghi, Hector Fontana, Daniel Grigera, María Angélica Moussalli, Tomas Grippo, Fabian Lerner, Alejo Peyret. Brazil: Heloisa Helena Abil Russ, Paulo Augusto Arruda Mello, Wilma Lelis Barboza, Sebastião Cronemberger, Alberto Diniz-Filho, Renato Germano, Jaír Giampani Jr, Ricardo Guedes, Nuvia Vanessa Lima, Nara Ogata, Della Paolera Mauricio, Lisandro Sakata, Marcelo Jordão Lopes da Silva, Remo Susanna Jr, Emilio Suzuki, Roberto Vessani. Bolivia: Denisse Aliaga, Manuel José Justiniano. Chile: Juan Jose Mura, Leonidas Traipe. Colombia: John Aristizabal, Sandra Belalcazar, Maria Fernanda Delgado, Fernando Gomez, Juan Camilo Parra Restrepo, Juan Rueda, Omar Salamanca. Ecuador: Carlos Luis Chacón, Ana Maria Vasquez. México: Carlos Alvarez, María Magdalena García Huerta, Felix Gil-Carrasco, Curt Hartleben México, Gabriel Lazcano, Jasbeth Ledesma, Marina Ramirez. Perú: Guillermo Barreto Fong, Vania Castro Tamanaja, Alberto Dios Aleman, Rodolfo Perez. Venezuela: Marcos Boissiere.
AUTHORS' CONTRIBUTIONS:
Significant contribution to conception and design: Manuel José Justiniano, Juan José Agustín Mura Castro, Guillermo Barreto Fong. Data acquisition: Manuel José Justiniano, Juan José Agustín Mura Castro, Jair Giampani Junior, Marcelo Jordão Lopes Silva. Data analysis and interpretation: Manuel José Justiniano, Juan José Agustín Mura Castro, Jair Giampani Junior. Manuscript drafting: Manuel José Justiniano, Juan José Agustín Mura Castro, Marcelo Jordão Lopes Silva, Guillermo Barreto Fong. Significant intellectual content revision of the manuscript: Manuel José Justiniano, Juan José Agustín Mura Castro, Guillermo Barreto Fong. Final approval of the submitted manuscript: Manuel José Justiniano, Juan José Agustín Mura Castro, Jair Giampani Junior, Marcelo Jordão Lopes Silva, Guillermo Barreto Fong. Statistical analysis: Juan José Agustín Mura Castro, Marcelo Jordão Lopes Silva. Obtaining funding: not applicable. Supervision of administrative, technical, or material support: Jair Giampani Junior, Marcelo Jordão Lopes Silva, Guillermo Barreto Fong. Research group leadership: Manuel José Justiniano, Guillermo Barreto Fong.
REFERENCES
1. Oxman AD, Sackett DL, Guyatt GH; The Evidence-Based Medicine Working Group. Users' guides to the medical literature. I. How to get started. JAMA. 1993;270(17):2093-5.
2. American Academy of Ophthalmology. About Preferred Practice Patterns (PPPs). AAP; [cited 2023 Mar 24]. Available from: https://www.aao.org/education/about-preferred-practice-patterns
3. Marques AP, Ramke J, Cairns J, Butt T, Zhang JH, Jones I, et al. The economics of vision impairment and its leading causes: A systematic review. EClinicalMedicine. 2022;46:101354.
4. Fellman RL, Mattox C, Singh K, Flowers B, Francis BA, Robin AL, et al. American Glaucoma Society Position Paper: Microinvasive Glaucoma Surgery. Ophthalmol Glaucoma. 2020;3(1):1-6.
5. Wong YL, Walkden A, Mercieca K. Surgical advancement in glaucoma during the past 10 years. Ophthalmologie. 2022;119(S2 Suppl 2):140-6.
6. Gold FE, Yadollahikhales M, Dersu II. National utilization of glaucoma laser and surgical management in medicare beneficiaries: disparities and Accessibility. J Glaucoma. 2023;32(12):1038-43.
7. Chan PP, Larson MD, Dickerson JE Jr, Mercieca K, Koh VT, Lim R, et al. Minimally invasive glaucoma surgery: latest developments and future challenges. Asia Pac J Ophthalmol (Phila). 2023;12(6):537-64.
8. Levin AM, Sheybani A. Glaucoma surgical procedures under development. Curr Opin Ophthalmol. 2024;35(2):111-5.
9. Marcus HJ, Payne CJ, Hughes-Hallett A, Marcus AP, Yang GZ, Darzi A, et al. Regulatory approval of new medical devices: cross sectional study. BMJ. 2016 May;353:i2587.
10. Aronson JK, Heneghan C, Ferner RE. Medical devices: definition, classification, and regulatory implications. Drug Saf. 2020;43(2):83-93.
11. Matovu B, Takuwa M, Mpaata CN, Denison F, Kiwanuka N, Lewis S, et al. Review of investigational medical devices' clinical trials and regulations in Africa as a benchmark for new innovations. Front Med Technol. 2022;4:952767.
12. Argotti U, Leyens L, Lisbona C, López P, Alonso-Orgaz S, Nevado A, et al. Comparison of the Latin America Regulation Landscape and International Reference Health Authorities to Hasten Drug Registration and Clinical Research Applications. Ther Innov Regul Sci. 2023;57(6):1287-97.
13. Torres RM. Tropicalization of medicine in clinical and research. Oftal Clin Exp. 2024;17(1):e1-3.
14. Lerner SF, Singh K, Susanna R Jr, Wilson MR, Lee BL, Maul E; Latin America Glaucoma Rand Study Group. RAND-like appropriateness methodology consensus for primary open-angle glaucoma in Latin America. Am J Ophthalmol. 2012;154(3):460-465.e7.
15. Grigera DE, Mello PA, Barbosa WL, Casiraghi JF, Grossmann RP, Peyret A. Level of agreement among Latin American glaucoma subspecialists on the diagnosis and treatment of glaucoma: results of an online survey. Arq Bras Oftalmol. 2013;76(3):163-9.
16. Vinod K, Gedde SJ, Feuer WJ, Panarelli JF, Chang TC, Chen PP, et al. Practice Preferences for Glaucoma Surgery: A survey of the American Glaucoma Society. J Glaucoma. 2017;26(8):687-93.
17. Iwasaki K, Arimura S, Takamura Y, Inatani M. Clinical practice preferences for glaucoma surgery in Japan: a survey of Japan Glaucoma Society specialists. Jpn J Ophthalmol. 2020;64(4):385-91.
18. Choudhari NS, Pathak-Ray V, Kaushik S, Vyas P, George R. Understanding practice patterns of glaucoma sub-specialists in India. Int J Ophthalmol. 2017;10(10):1580-5.
19. Gazzard G, Konstantakopoulou E, Garway-Heath D, Adeleke M, Vickerstaff V, Ambler G, et al.; LiGHT Trial Study Group. Laser in Glaucoma and Ocular Hypertension (LiGHT) Trial: six-year results of primary selective laser trabeculoplasty versus eye drops for the treatment of glaucoma and ocular hypertension. Ophthalmology. 2023;130(2):139-51.
20. Gazzard G, Konstantakopoulou E, Garway-Heath D, Garg A, Vickerstaff V, Hunter R, et al. Selective laser trabeculoplasty versus drops for newly diagnosed ocular hypertension and glaucoma: the LiGHT RCT. Health Technol Assess. 2019;23(31):1-102.
21. Rolim-de-Moura CR, Paranhos A Jr, Loutfi M, Burton D, Wormald R, Evans JR. Laser trabeculoplasty for open-angle glaucoma and ocular hypertension. Cochrane Database Syst Rev. 2022 Aug;8(8):CD003919.
22. Michaelov E, Armstrong JJ, Nguyen M, Instrum B, Lam T, Denstedt J, et al. Assessing the methodological quality of glaucoma clinical practice guidelines and their recommendations on microinvasive glaucoma surgery: a systematic review. J Glaucoma. 2018;27(2):e44-9.
23. Kansal V, Armstrong JJ, Hutnik CM. trends in glaucoma filtration procedures: a retrospective administrative health records analysis over a 13-year period in canada. Clin Ophthalmol. 2020 Feb;14:501-8.
24. Cantor L, Lindfield D, Ghinelli F, Świder AW, Torelli F, Steeds C, et al. Systematic literature review of clinical, economic, and humanistic outcomes following minimally invasive glaucoma surgery or selective laser trabeculoplasty for the treatment of open-angle glaucoma with or without cataract extraction. Clin Ophthalmol. 2023;17:85-101.
25. Song A, Lusk JB, Kuo AN, Muir KW, Stinnett SS, Borkar DS. Systematic analysis of levels of evidence supporting American Academy of Ophthalmology Preferred Practice Pattern guidelines, 2012-2021. BMC Ophthalmol. 2023;23(1):132.
Submitted for publication:
April 23, 2025.
Accepted for publication:
October 8, 2025.
Data Availability Statement: The datasets generated and/or analyzed during the current study are included in the manuscript.
Edited by
Editor-in-Chief: Newton Kara-Júnior Associate Editor: Tiago S. Prata
Funding: This study received no specific financial support.
Disclosure of potential conflicts of interest: The authors declare no potential conflicts of interest.