

Frederico França Marques1,2; Daniel Filipe Oliveira Rabelo1; Daniela Meira Villano Marques1,2; Glauco Sérgio Avelino de Aquino1; Daniel Diniz da Gama1; Bernardo Kaplan Moscovici1,3
DOI: 10.5935/0004-2749.2023-0221
ABSTRACT
We present a case of a patient complaining of monocular diplopia due to a decentered ablation after LASIK. The patient underwent a wavefront-guided retreatment, which resulted in an epithelial ingrowth complication. Additionally, the patient developed cataract, with cataract surgery requiring reliable biometric measurements. Therefore, we opted for corneal treatment and corneal surface regularization. Although we attempted to lift the flap and wash the interface initially, the procedure proved unsuccessful, thereby necessitating immediate flap amputation. Once the corneal surface was regularized in the seventh postoperative month, transepithelial photorefractive keratectomy was successfully performed to homogenize the ocular surface, thereby significantly improving the patient's corrected visual acuity and resolving monocular diplopia. The surface and corneal curvature stabilized by the fifth month after the procedure. Phacoemulsification was then performed along with the implantation of a toric monofocal lens, which was selected using an appropriate formula, resulting in an excellent uncorrected visual acuity.
Keywords: Refractive surgical procedures; Surgical flap/surgery; Keratomileusis laser In situ/methods; Biometry; Corneal topography; Lasers, Excimer/adverse effects; Dipoplia/etiologia; Visual acuity; Humans; Case reports
INTRODUCTION
Refractive procedures are generally safe, but they are associated with some risks. The risk rate reported for refractive procedures is <2%. LASIK-related postoperative complications include those related to the interface, such as fluid or cell accumulation. This accumulation promotes inflammatory and infectious processes, including epithelial growth and flap necrosis(1-10).
We here present the treatment of a patient who developed monocular diplopia due to decentered ablation, interface epithelialization, and flap edge necrosis combined with cataract after an unsuccessful LASIK.
CASE REPORT
A 55-year-old man presented to our service in 2016 complaining of monocular diplopia in the right eye (OD), which persisted since 2002 after the patient underwent LASIK in both eyes to correct myopic astigmatism. The patient reported that the treatment was not perfectly centralized. Wavefront-guided enhancement was performed 2 months later with no success.
The corrected distance visual acuity (CDVA) was 20/60 for his right eye (OD) (+4.00 −2.00 150) and 20/20 in the left eye (OS). During slit-lamp examination, epithelial growth was noted in the OD temporal interface (Figure 1A).
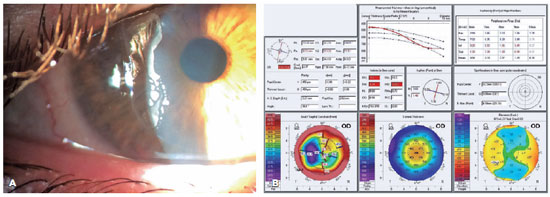
Pentacam corneal tomography (Oculus, Germany) was performed in both eyes. This procedure revealed OD with a flat and irregular cornea with astigmatism ranging from 28D to 38D at the pupil area, which explains the development of monocular diplopia (Figure 1B).
On discussing the procedure for removing epithelial growth with the patient, the patient preferred to wait. Five years later (2021), he returned with a worsening visual acuity (VA) in the OD because of the presence of a subcapsular cataract along with monocular diplopia. Considering that phacoemulsification was required in the OD, we first addressed the cornea to regularize its surface and obtain reliable biometry. We were aware that we may have to amputate the lamella if any extremely friable tissue was found.
During surgery, we aimed to lift the lamella and remove the epithelial cells. However, the lamella was extremely friable and irregular. Therefore, the amputation of the lamella was planned, followed by the application of 0.02% mitomycin for 2 min and exhaustive washing for preventing haze development.
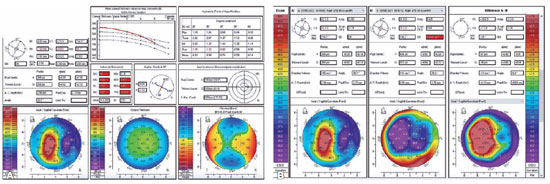
After 9 months, the patient presented a CDVA of 20/30 with a rigid contact lens and stable topography (Figure 2A and B).
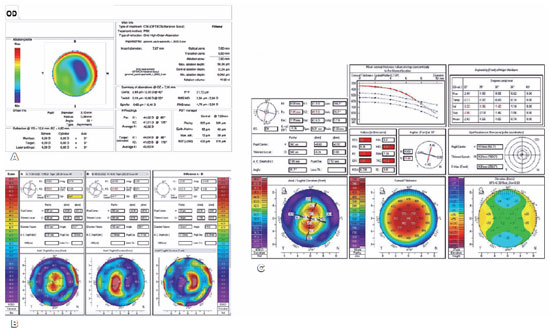
In June 2022, transepithelial photorefractive keratectomy (TransPRK) topography-guided surgery was performed using the Amaris 1050 platform (Schwind, Kleinotheim, Germany) (Figure 3A) to regularize the corneal surface. At the second and third months after operation, the patient's CDVA remained at 20/25 with −3.50 DS −3.50 DC 150 with a topographic central symmetrical astigmatism of 3.7D, consistent with his manifest refraction. For the first time, the patient experienced a huge improvement in monocular diplopia because of the central regularity of the cornea (Figure 3B and C).
We then finally decided to resolve the cataract. Biometry was performed comparing several formulas such as Haigis L, Barrett True K, and Double K. Despite the patient being initially subjected to laser ablation for myopia, all formulas were used with a hyperopic correction because of the final prolate aspect of the cornea evidenced through topography.
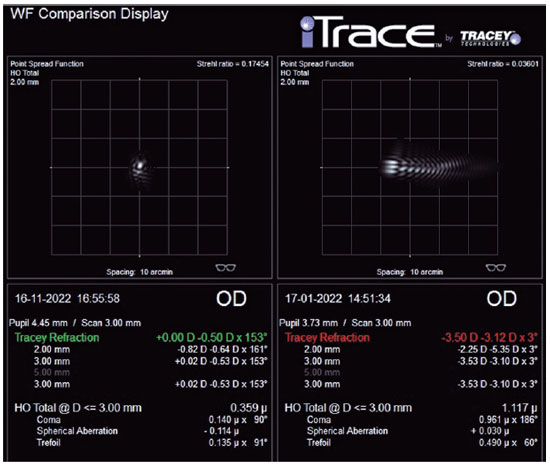
Therefore, in the fifth month after TransPRK, the patient was subjected to an uneventful phacoemulsification with implantation of a toric monofocal IOL, thereby resulting in an uncorrected VA (UCVA) of 20/20p with minimal monocular diplopia and comfortable binocular VA. Aberrometry using the point spread function (high-order) was used to confirm improvement after all treatments (Figure 4).
DISCUSSION
Monocular diplopia is a rare postoperative complication of LASIK. Our patient presented with monocular diplopia in the OD due to decentered ablation, interface epithelialization, and flap edge necrosis combined with cataracts.
In patients developing monocular diplopia after LASIK, other potential causes of monocular diplopia, such as corneal irregularities or ocular misalignment, should be ruled out first.
Once the diagnosis is confirmed, treatment options vary depending on the etiology of the condition. In our patient, monocular diplopia was developed by two main causes: decentered ablation and epithelial ingrowth.
Decentered ablation is a rare complication that occurs nowadays because of an improvement in eye trackers. However, the incidence of the complication ranges between 0.2% and 4%, which results in high-order aberrations and low VA. Some authors have suggested that decentered or irregular flaps, head misalignment, or patient failure to fixate in the excimer laser-guiding light and high kappa angle are the leading causes of this complication(1-3,9).
The gold standard for correcting decentered ablations is total wavefront-guided or corneal wavefront-guided treatments (topography-guided)(4,5,9).
Several factors can contribute to epithelial ingrowth development, such as incomplete flap adherence, trauma, epithelial proliferation, greater ablations and hyperopic treatments, debris accumulation at the flap edge, and especially retreatments. The incidence of epithelial ingrowth after LASIK is 0.2%-2.0% in primary cases and 10%-20% in retreatments. Epithelial ingrowth is often asymptomatic or minimally symptomatic. However, it can lead to severe vision loss in some patients and require intervention(1-6).
Epithelial ingrowth management can be challenging. As part of its typical treatment, the affected interface is mechanically dibridged. However, additional interventions such as alcohol, mitomycin C, fibrin glue, ND Yag laser, sutures, amniotic membrane grafts, or even flap amputation may be necessary for recurrent or refractory cases(1-6).
In the present case, flap amputation was necessary because epithelial ingrowth was severe and irregular, which was followed by mitomycin C for preventing haze development. In cases with severe flap edge necrosis, closing the pathway for epithelial ingrowth is challenging, and using sutures and fibrin glue can be attempted. However, we could not achieve an acceptable outcome because of necrosis, as observed in some published cases. When amputation of the LASIK flap is decided, mitomycin C must be applied to avoid haze formation, and we must be prepared for irregular topography in the postoperative period(6-8).
The patient presented a stable topography after the procedure was completed, but corneal irregularity persisted. Therefore, a TransPRK topography-guided procedure was performed. Topography-guided ablation allows to precisely correct corneal irregularities and can significantly improve VA, as observed in our case. Both waveguided and topography-guided treatments exhibit excellent results in treating irregular corneas. One among the two approaches should be chosen based on the surgeon's expertise with the technology and availability(4,5,9).
Because the cornea was irregular, some devices that perform wavefront-guided surgeries could not capture reliable images. Topography-guided surgeries aim to correct the cornea's shape without considering the patient's ametropia. Residual ametropia was not a concern in our patient because the patient had to undergo cataract surgery after topographical regularization(4,5,9).
In the present case, the formula used for biometry was essential in achieving the desired outcome. Several formulas were considered, but because of the final prolate aspect of the cornea observed through topography, all formulas were used with hyperopic correction(10).
In conclusion, the present case revealed that even after some postoperative excimer laser complications, the patient may still achieve excellent functional vision through the application of correct treatments.
REFERENCES
1. dos Santos AM, Torricelli AA, Marino GK, Garcia R, Netto MV, Bechara SJ, et al. Femtosecond laser-assisted LASIK flap complications. J Refract Surg. 2016 ;32(1):52-9.
2. Estopinal CB, Mian SI. LASIK Flap: Postoperative complications. Int Ophthalmol Clin. 2016 ;56(2):67-81.
3. Saito MS, Soares PV, Barboza GN, Barboza MN, Torricelli AA, Moscovici BK. Ablação personalizada guiada por frente de onda após complicação na dissecção lamelar de FemtoLasik. Rev Bras Oftalmol [Internet]. 2023[citado 2023 Jun 21];82:e0021 Avaiable from:. SciELO - Brasil - Ablação personalizada guiada por frente de onda após complicação na dissecção lamelar de FemtoLasik Ablação personalizada guiada por frente de onda após complicação na dissecção lamelar de FemtoLasik
4. Mrochen M, Krueger RR, Bueeler M, Seiler T. Aberration-sensing and wavefront-guided laser in situ keratomileusis: management of decentered ablation. J Refract Surg. 2002;18(4):418-29.
5. Kymionis GD, Panagopoulou SI, Aslanides IM, Plainis S, Astyrakakis N, Pallikaris IG. Topographically supported customized ablation for the management of decentered laser in situ keratomileusis. Am J Ophthalmol. 2004;137(5):806-11.
6. Ting DS, Srinivasan S, Danjoux JP. Epithelial ingrowth following laser in situ keratomileusis (LASIK): prevalence, risk factors, management and visual outcomes. BMJ Open Ophthalmol [Internet]l. 2018[cited 2023 Jan 21];3(1):e000133.Available from: Epithelial ingrowth following laser in situ keratomileusis (LASIK): prevalence, risk factors, management and visual outcomes - PMC (nih.gov)
7. Chhadva P, Cabot F, Galor A, Karp CL, Yoo SH. Long-term outcomes of flap amputation after LASIK. J Refract Surg. 2016;32(2):136-7.
8. Kymionis G, Ide T, Yoo S. Flap amputation with phototherapeutic keratectomy (PTK) and adjuvant mitomycin C for severe post-LASIK epithelial ingrowth. Eur J Ophthalmol. 2009;19(2):301-3.
9. Rios LC, Silva PG, Canamary Junior AM, Rodrigues P, Regatieri CV, Campos M, et al. Centration in refractive surgery. Arq Bras Oftalmol [Internet]. 2020[cited May 21];83(1):76-81. Available from: SciELO - Brasil - Centration in refractive surgery Centration in refractive surgery
10. Wang L, Koch DD. Intraocular lens power calculations in eyes with previous corneal refractive surgery: review and expert opinion. Ophthalmology. 2021;128(11):e121-e131.
Authors' contribution:
Substantial contribution to conception and design: Frederico França Marques , Daniel Filipe Oliveira Rabelo, Bernardo Kaplan Moscovici. Acquisition of data: Frederico França Marques, Daniela Meire Villano Marques, Glauco Sergio Avelino de Aquino, Bernardo Kaplan Moscovici. Analysis and interpretation of data: Frederico França Marques, Bernardo Kaplan Moscovici, Daniel Diniz da Gama. Drafting of the manuscript: Frederico França Marques, Glauco Sergio Avelino de Aquino, Daniel Filipe Oliveira Rabelo, Bernardo Kaplan Moscovici. Critical revision of the manuscript for important intellectual content: Frederico França Marques, Daniela Meire Villano Marques, Bernardo Kaplan Moscovici, Daniel Diniz da Gama. Have given final approval of the submitted manuscript (mandatory participation for all authors): Frederico França Marques, Daniel Filipe Oliveira Rabelo, Daniela Meire Villano Marques, Bernardo Kaplan Moscovici, Glauco Sergio Avelino de Aquino, Daniel Diniz da Gama
Statistical analysis:
Obtaining funding:
Administrative, technical, or material support supervision: Frederico França Marques, Bernardo Kaplan Moscovici, Daniel Diniz da Gama. Research group leadership: Frederico França Marques, Bernardo Kaplan Moscovici.
Submitted for publication:
July 27, 2023.
Accepted for publication:
October 5, 2023.
Approved by the following research ethics committee: Instituto Suel Abujamra (CAAE: 71211023.7.0000.5477).
Funding: This study received no specific financial support.
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose.