

Renato Bezerra Kitahara; Fernando Henrique Flores Teixeira; Fernando Moreira dos Santos; Flavio Mac Cord Medina; Mário Martins dos Santos Motta
DOI: 10.5935/0004-2749.2022-0121
Dear Editor,
Angioid streaks (AS) are breaks that occur in a calcified and weakened Bruch’s membrane(1,2). Approximately 50% of the cases are idiopathic, whereas other cases present with an associated systemic conditions, most frequently pseudoxanthoma elasticum, Paget’s disease, hemoglobinopathies, and Ehlers-Danlos syndrome(1,2). Generally, they emerge between the second and fifth decades of life, depending on the associated systemic diseases(2). Fundoscopic examination identifies AS bilaterally as reddish-brown, jagged, subretinal lines, with variable caliber, which radiate from the peripapillary region toward the peripheral retina. AS become darker as they develop and may increase in number, diameter, and extent(1,2). Initially, AS are usually asymptomatic. Visual impairment occurs because of foveal involvement or with choroidal neovascularization (CNV)(1,2).
By contrast, pattern dystrophies (PD) are a heterogeneous group of disorders that present changes in the pigment epithelium of the macular region(3,4). Gass divided PD into five forms according to the pigment distribution pattern, namely, adult-onset foveomacular vitelliform dystrophy, butterfly pattern dystrophy, multifocal pattern dystrophy simulating fundus flavimaculatus, reticular dystrophy of the pigment epithelium, and fundus pulverulentus(3,4). Occasionally, different patterns can coexist in the same individual. In some cases, transformations occur, and one pattern develops into another(4). This case report described a case of PD-associated AS.
A 61-year-old man with hypertension and a pituitary adenoma diagnosed 3 years ago visited the ophthalmology outpatient clinic for a routine appointment. He had no systemic or ophthalmologic complaints. However, his corrected visual acuity was 20/80 in the right eye and 20/40 in the left eye. The right and left intraocular pressures were 13 and 15 mmHg, respectively. No changes in the anterior segment were noted. Fundoscopic examination showed linear, darkened, and deep lesions in both eyes, starting from the optic disc toward the periphery, compatible with the diagnosis of AS. He also presented yellowish, round, and confluent lesions at the posterior pole, suggesting the appearance of multifocal vitelliform lesions (Figure 1).
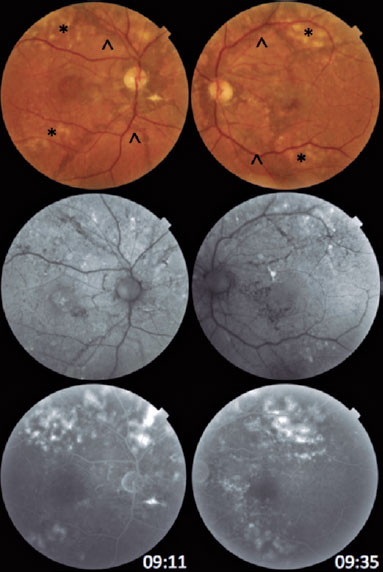
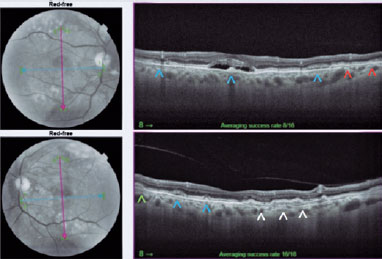
Fundus autofluorescence (FAF) showed hypoautofluorescent lines starting from the optic disc in both eyes and small, sparse hyperautofluorescent lesions in the posterior pole (Figure 1). Optical coherence tomography (OCT) of the right eye detected a subfoveal hyporeflective space containing hyperreflective materials. In the left eye, a double-layer sign was seen, but without signs of exudation (Figure 2).
OCT angiography (OCT-A) and fundus fluorescein angiography (FFA) were performed in both eyes. No flow or leakage compatible with the diagnosis of subretinal neovascular membrane was detected. Areas of hyperfluorescence near the temporal arcades were visualized bilaterally (Figure 1).
Multimodal evaluation of the posterior segment confirmed that the case was an association of two ophthalmological diseases, AS and adult-onset foveomacular vitelliform dystrophy of the multifocal type. The concomitant presence of AS and PD has been established in the literature and commonly described in patients with pseudoxanthoma elasticum(1). This diagnosis was excluded for our patient by the medical clinic and dermatology teams. This PD subtype presents with central or paracentral subretinal deposits, yellowish and round, which appear as hyperautofluorescent lesions in the FAF and hyperreflective lesions between the retinal pigment epithelium (RPE) and inner segment/outer segment (IS/OS) layer of photoreceptors in the OCT(3,4). Druses, large or small, are an important differential diagnosis of vitelliform lesions, but they are located between the RPE and Bruch’s membrane(4,5).
PD usually shows a slow and progressive course. A slight decrease in visual acuity and mild metamorphopsia which start around the fifth decade are the most common complaints. However, severe visual impairment can occur in up to 50% of patients after age 70 years because of geographic macular atrophy or CNV(4).
The patient had two entities that were potentially progressing to CNV. In the OCT of the right eye, changes observed may lead to the erroneous diagnosis of active CNV. Through multimodal analysis using OCT-A and FFA, the changes indicated a resorbing vitelliform deposit. Owing to the possible emergence of a neovascular membrane, the patient was followed with serial tests.
REFERENCES
1. Korol AR, Rostel VV. Angioid streaks of the retina. J Ophthalmol (Ukraine). 2021(2):499.
2. Chatziralli I, Saitakis G, Dimitriou E, Chatzirallis A, Stoungioti S, Theodossiadis G, et al. Angioid streaks: a comprehensive review from pathophysiology to treatment. Retina. 2019;39(1):1-11.
3. Hanif AM, Yan J, Jain N. Pattern dystrophy: an imprecise diagnosis in the age of precision medicine. Int Ophthalmol Clin. 2019; 59(1):173-94.
4. Ozkaya A, Garip R, Nur Tarakcioglu H, Alkin Z, Taskapili M. Clinical and imaging findings of pattern dystrophy subtypes; Diagnostic errors and unnecessary treatment in clinical practice. J Fr Ophtalmol. 2018;41(1):21-9.
5. Lima LH, Laud K, Freund KB, Yannuzzi LA, Spaide RF. Acquired vitelliform lesion associated with large drusen. Retina. 2012; 32(4):647-51.
Submitted for publication:
October 5, 2022.
Accepted for publication:
October 28, 2022.
Funding: This study received no specific financial support.
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose.