

Li Dai1; Ai-Ling Li2; Ling Yu1,3; Jian Ye3
DOI: 10.5935/0004-2749.202100111
Dear Editor,
Glaucoma is one of the major causes of blindness worldwide and seriously affects patients’ visual quality and daily life. The most effective measure to prevent glaucomatous damage is to reduce intraocular pressure (IOP) through anti-glaucoma medication, laser treatment, or surgery. CO2 laser-assisted sclerectomy surgery (CLASS) is a promising, newly developed surgical treatment applied mainly to the treatment of open-angle glaucoma (OAG). Compared with other filtration surgery, CLASS has unique advantages: requiring only a relatively short learning curve for the surgeon, preventing penetration of the sclera and trabecular meshwork through precise control of laser energy and range, keeping the inner wall of the Schlemm tube intact, and preserving functional trabecular meshwork(1).
As it has been used successfully to treat OAG, related clinical studies on CLASS are increasing year by year. However, most of these are small sample, non-randomized controlled trials (RCT). Further, although most studies argue that CLASS is safe and effective at treating glaucoma, some suggest that CLASS is less potent than trabeculectomy (TRAB) in reducing IOP(2). At present, there is no consensus on whether CLASS is better than TRAB or other filtration surgery.
We evaluated the effectiveness and safety of CLASS for treating glaucoma by systematically reviewing and meta-analyzing related studies as described in table 1. Nine studies were included, three of which compared CLASS with TRAB. Stata15.0 software was used for the statistical analysis.
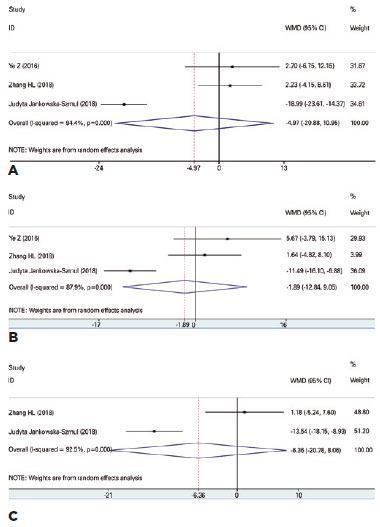
The meta-analysis showed a statistically significant difference between postoperative and preoperative IOP at 3, 6 and 12 months (MD=-10.95, 95%CI -14.66 ± -7.24, p<0.001, MD=-11.29, 95%CI -16.09 ± -6.50, p<0.001, and MD=-11.14, 95%CI -14.56 ± -7.73, p<0.001, respectively). Three articles compared IOPR% at 1, 3, and 6 months after CLASS and TRAB (Figure 1), and there was no difference at any of these timepoints (MD=-4.97, 95%CI -20.88 ± 10.95, p=0.54, MD= -1.89, 95%CI -12.84 ± 9.05, p=0.74, MD=-6.36, 95%CI -20.78 ± 8.06, p=0.39, respectively). In other words, there was no difference between CLASS and TRAB in the reduction of IOP.
Four studies recorded the average use of anti-glaucoma medication 12 months after CLASS, and the meta-analysis showed that this was reduced compared with preoperative medication use (MD=-1.48, 95%CI -1.95 ± -1.02, p<0.00001). Regarding safety, nine articles reported postoperative complications of CLASS, including shallow anterior chamber, choroidal detachment, hyphema, and iris incarceration. There was a statistically significant difference between CLASS and TRAB in the above postoperative complications, and TRAB group had a higher rate, but no difference in the incidence of iris incarceration (RR=2.40, 95%CI 0.57 ± 10.11, p=0.23). It may be due to the limited data and relatively short follow-up period in this study, or the surgeon’s technique. CLASS was reported to have both high postoperative complete success rate and qualified success rate(4,7). However, as the different definitions in the included studies, we failed to compare it with TRAB.
CLASS is increasingly preferred by ophthalmologists for glaucoma treatment. It can effectively reduce the IOP and the use of anti-glaucoma medications and has a good safety profile (Figure 2). However, most of the current studies on CLASS treatment for glaucoma are not RCT. To more accurately assess the effectiveness and safety of CLASS for treating glaucoma, these findings need to be verified by more high-quality RCT with long-term observation and various evaluation indices such as visual acuity and retinal nerve fiber layer thickness.

Since CLASS was introduced into China in 2015, it has been promoted and developed continuously to observe its efficacy combined with other surgical methods in the treatment of glaucoma or glaucoma with cataract. According to Yu et al.(11), CLASS with phacoemulsification may become a safe and effective intervention for patients with primary open-angle glaucoma (POAG) and visually significant cataracts. Zhang et al.(12) also achieved precise treatment for POAG patients in China through the combination of modified CLASS and preventive laser iris management; their findings suggested that this was an effective and safe long-term treatment for POAG. Finally, this meta-analysis showed that CLASS can significantly reduce IOP and has higher safety. We believe that more high-quality RCT studies will confirm the efficacy of CLASS in the future.
ACKNOWLEDGMENTS
This research is financed by the National Nature Science Foundation of China (No.82070962).
REFERENCES
1. Ton Y, Assia EI, Geffen N. Performing accurate CO2 laser-assisted sclerectomy surgery. Expert Rev Ophthalmol. 2015;10(1):5-11.
2. Ye Z, Wang D, Li Z. The short-term of clinical safety and efficiency of CO2 laser-assisted sclerectomy surgery (CLASS)[J]. Yan Ke Xue Bao. 2016;31(4):259-65.
3. Liu C, Lin X, Lihong L, Murui Z, Shaoshan L. Clinical observation of CO2 laser-assisted deep sclerectomy in the treatment of open-angle glaucoma. Southwestern National Defense Medicine. 2017; 27(10):1110-2.
4. Zhang HL, Tang GX, Li F, Yan XW, Ma LH, Geng YL. Efficacy of laser-assisted deep sclerectomy for open angle glaucoma. Chin J Ocul Traum Occup Eye Dis. 2018;40(3):203-7. doi.org/10.3760/cma.j.issn.2095-1477.2018.03.011
5. Geffen N, Mimouni M, Sherwood M, Assia EI. Mid-term Clinical Results of CO2 Laser-assisted Sclerectomy Surgery (CLASS) for Open-Angle Glaucoma Treatment. J Glaucoma. 2016;25(12):946-51.
6. Greifner G, Roy S, Mermoud A. Results of CO2 Laser-assisted Deep Sclerectomy as Compared with Conventional Deep Sclerectomy. J Glaucoma. 2016;25(7):e630-8.
7. Jankowska-Szmul J, Dobrowolski D, Wylegala E. CO2 laser-assisted sclerectomy surgery compared with trabeculectomy in primary open-angle glaucoma and exfoliative glaucoma. A 1-year follow-up. Acta Ophthalmol. 2018;96(5):e582-91.
8. Sohajda Z, Káldi I, Kiss M, Facskó A. [Experiences with CO2 laser-assisted sclerectomy surgery]. Orv Hetil. 2017;158(18):701-5. Hungarian.
9. Yick DWF, Lee JWY, Tsang S, Yeung BYM, Yuen CYF. Preliminary results of CO2 laser-assisted sclerectomy surgery (CLASS) in the treatment of advanced glaucoma in a Chinese population, Medicine. 2016;95(45):e5294.
10. Sohajda Z, Széll N, Revák Á, Papp J, Tóth-Molnár E. Retinal Nerve Fibre Layer Thickness Change After CO2 Laser-Assisted Deep Sclerectomy Surgery. Clin Ophthalmol. 2020 Jun 25;14:1749-57.
11. Yu X, Chen C, Sun M, Dong D, Zhang S, Liu P, et al. CO2 Laser-assisted deep sclerectomy combined with phacoemulsification in patients with primary open-angle glaucoma and cataract. J Glaucoma. 2018;27(10):906-9.
12. Zhang Y, Cheng G. Modified CO2 Laser-assisted sclerectomy surgery in chinese patients with primary open-angle glaucoma and pseudoexfoliative glaucoma: a 2-year follow-up study. J Glaucoma. 2020;29(5):367-73.
Submitted for publication:
April 17, 2021.
Accepted for publication:
May 3, 2021.
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose