

Gökhan Pekel1; Murat Taşçı2; Alperen Bahar3; Evre Pekel4; Ebru Nevin Çetin1; Çiğdem Martin1; Veli Çobankara2
DOI: 10.5935/0004-2749.20190054
ABSTRACT
Purpose: We aimed to compare the thickness of anterior sclera, corneal layers, and pre-ocular tear film between patients with primary Sjögren’s syndrome and healthy individuals.
Methods: Fifty-one patients with primary Sjögren’s syndrome and 41 healthy control participants were recruited in this cross-sectional and comparative study. The thickness of the pre-ocular tear film, corneal epithelium, Bowman’s layer, stroma, Descemet’s membrane, and endothelium were measured on the corneal apex. Anterior scleral thickness was measured at distances of 1 mm and 3 mm from the limbus. The anterior segment module of spectral-domain optical coherence tomography was used to measure thicknesses of pre-ocular tear film, corneal layers, and anterior sclera.
Results: Tear film thickness, Schirmer’s test, and tear break up time values were significantly lower in the Sjögren’s disease group than in the healthy controls (p<0.05). The thickness measurements of corneal layers and sclera were similar between the groups. Tear film thickness was moderately correlated with the Schirmer’s test results (r=0.34, p=0.001), but there was no correlation between the Schirmer’s test results and tear break up time (r=0.18, p=0.09).
Conclusions: Pre-ocular tear film, as measured by anterior segment optical coherence tomography, was thinner in patients with primary Sjögren’s syndrome than in the healthy controls. The thicknesses of corneal layers and anterior sclera were similar between the groups.
Keywords: Sclera; Sjögren-Larsson syndrome; Anterior eye segment; Tomography, optical coherence; Comparative study
RESUMO
Propósito: Nosso objetivo foi comparar a espessura da esclera anterior, camadas da córnea e do filme lacrimal pré-ocular entre pacientes com síndrome de Sjögren primária e indivíduos saudáveis.
Métodos: Cinquenta e um pacientes com síndrome de Sjögren primária e 41 controles saudáveis foram recrutados neste estudo comparativo e transversal. A espessura do filme lacrimal pré-ocular, epitélio corneal, camada de Bowman, estroma, membrana de Descemet e endotélio foram medidos no ápice corneal. A espessura da esclera anterior foi medida às distâncias de 1 mm e 3 mm do limbo. O módulo do segmento anterior da tomografia de coerência óptica de domínio espectral foi utilizado para mensurar as espessuras do filme lacrimal pré-ocular, camadas da córnea e esclera anterior.
Resultados: A espessura do filme lacrimal, o teste de Schirmer e os valores do tempo de ruptura do filme lacrimal foram significativamente menores no grupo com síndrome de Sjögren do que nos controles saudáveis (p<0,05). As medidas de espessura das camadas corneais e da esclera foram similares entre os grupos. A espessura do filme lacrimal foi moderadamente correlacionada com os resultados do teste de Schirmer (r=0,34, p=0,001), mas não houve correlação entre os resultados do teste de Schirmer e tempo de ruptura (r=0,18, p=0,09).
Conclusões: O filme lacrimal pré-ocular, medido pela tomografia de coerência óptica de segmento anterior, foi mais fino em pacientes com síndrome de Sjögren primária do que nos controles saudáveis. As espessuras das camadas da córnea e da esclera anterior foram semelhantes entre os grupos.
Descritores: Esclera; Síndrome de Sjogren-Larsson; Segmento anterior do olho; Tomografia de coerência óptica; Estudo comparativo
INTRODUCTION
Primary Sjögren’s syndrome is a systemic autoimmune disease of the secretory glands that primarily affects middle-aged (age range 40-65 years) women(1). Lacrimal glands are involved; these serve as the source of dry-eye disease. The pathogenesis of primary Sjögren’s syndrome is not well-understood, but lymphocytic infiltration of the secretory glands is suspected to play an important role(2). In addition to dry-eye disease, primary Sjögren’s syndrome may cause dryness of the oral cavity and abnormalities of the cutaneous, musculoskeletal, pulmonary, and renal systems, as well as disorders in any organ system(3).
Pre-ocular tear film, as well as the cornea and conjunctiva, are the most affected ocular structures in patients with primary Sjögren’s syndrome(3,4). Previous studies have shown that corneal nerve density is reduced in patients with primary Sjögren’s syndrome(5). Tear osmolarity, which is an indicator of dry-eye disease, is higher in patients with primary Sjögren’s syndrome than in healthy individuals(6). Conjunctival impression cytology examinations revealed squamous metaplasia, including goblet cell loss, in patients with Sjögren’s syndrome(7). However, the effects of primary Sjögren’s syndrome on the thickness of the anterior sclera, corneal layers, and tear film were not investigated yet.
The present study aimed to evaluate the thickness of tear film, corneal layers, and anterior sclera in patients with primary Sjögren’s syndrome via anterior segment optical coherence tomography (AS-OCT). Additionally, this study assessed correlations between pre-ocular tear film thickness and standard dry-eye disease tests (i.e., Schirmer’s test and tear breakup time (TBUT)). We hypothesized that tear film thickness, corneal epithelial thickness, and anterior scleral thickness may be altered in patients with primary Sjögren’s syndrome due to the close relationships of these structures with proper functioning of the lacrimal glands. We believe that the present paper is the first study on this topic in the literature.
METHODS
Fifty-one eyes of 51 patients with primary Sjögren’s syndrome and 41 eyes of 41 healthy individuals were recruited for this cross-sectional study, which was conducted in a tertiary setting upon the approval of the institutional ethical committee; the study adhered to the principles of the Declaration of Helsinki, and all the participants provided informed consent.
Study population
Patients with primary Sjögren’s syndrome were first evaluated in the Rheumatology Division and, then, were referred to the Eye Clinic. Patients were selected in accordance with the 2016 American College of Rheumatology/European League Against Rheumatism classification criteria for primary Sjögren’s syndrome.(8) Each patient in the study group had a history of dry-eye symptoms, but exhibited no other systemic or ocular diseases. All the participants received a standardized ophthalmological examination consisting of refractive error assessment, visual acuity examination with a Snellen chart, biomicroscopy, air-puff tonometry, Schirmer’s test, TBUT measurement, retinal examination, and AS-OCT measurements. Visual acuity values were 20/20 or better for all the participants. The exclusion criteria were a history of ocular surgery, systemic disease other than primary Sjögren’s syndrome, and any ocular disease except mild refractive errors. In addition, contact lens wearers, participants with a refractive error >2 diopters, and those with intraocular pressure >21 mmHg were excluded.
Ocular examination techniques
Only one eye from each participant was randomly selected for this analysis. We used the anterior segment module of the spectral-domain OCT (Spectralis software, version 6.0, Heidelberg, Germany) to measure tear film thickness, corneal layer thickness, and anterior scleral thickness. For viewing and analyzing the anterior segment structures, the Spectralis uses an add-on lens and software with an 8-16-mm scanning width and 3.9-µm axial resolution.
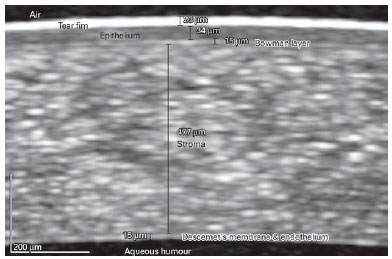
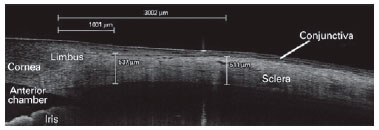
Figure 1 shows an example of the method by which we measured the thicknesses of the tear film and the layers of the cornea. Thickness measurements for the cornea and sclera were performed manually using caliber tools provided within the Spectralis software. We used a 600-800% zoom to analyze the images and recorded measurements of the pre-ocular tear film and corneal layers at the center of the cornea. Anterior scleral thickness measurements were performed at 1 mm and 3 mm from the limbus (Figure 2). The conjunctiva was eliminated to precisely measure the scleral thickness. The scleral curve was considered while drawing a measurement line for examinations at 3 mm; to maintain standardization only the temporal sclera was chosen in the analysis for all the participants.
All corneal and scleral thickness measurements were performed by a single investigator (GP), and all examinations were performed by a single experienced OCT technician. Both OCT examinations and manual measurements were repeated at least three times; the highest quality images were selected for statistical analysis.
Schirmer’s test was performed using 35 × 5-mm filter paper that was curved at one end for placement in the lower conjunctival sac, following application of a drop of topical anesthetic. We measured TBUT by applying a fluorescent drop to the eye; after a few blinks to spread the fluorescein diffusely over the cornea, we examined the pre-ocular tear film with the aid of blue light from a biomicroscope. The appearance of a dark area indicated a ruptured tear film; the time that had passed since the last blink was recorded as TBUT.
Statistical analysis
The Statistical Package for the Social Sciences (SPSS, version 17.0, Chicago, IL, USA) was used for statistical analysis. “p” values less than 0.05 were considered statistically significant. An independent-samples t-test was used to compare the analysis parameters between study and control groups. Pearson’s correlation analysis was used to detect associations between tear film and anterior segment variables. Confidence intervals for the Pearson’s correlation test were also calculated. The chi-squared test was used for the analysis of categorical values.
RESULTS
The mean age of patients in the Sjögren’s disease group (study group) was 51.6 ± 9.6 (range: 32-72) years, while the mean age of participants in the control group was 51.0 ± 6.5 (range: 39-69) years (p=0.74). There were 49 females and two males in the study group, and 39 females and two males in the control group (p=0.82). The mean refractive error (spherical equivalent) values of the study and control groups were -0.01 ± 0.95 diopters (D) and 0.21 ± 0.76 D, respectively (p=0.23). The mean intraocular pressure values of the study and control groups were 14.7 ± 2.5 mmHg and 14.1 ± 2.6 mmHg, respectively (p=0.27).
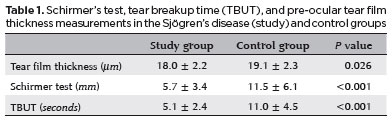
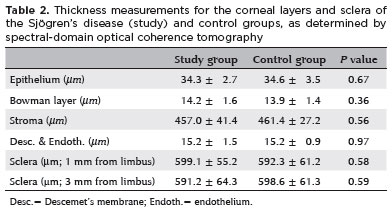
Table 1 shows Schirmer’s test, TBUT, and pre-ocular tear film thickness measurements in the study and control groups. Tear film thickness, Schirmer’s test, and TBUT values were significantly lower in the study group than in the control group (p<0.05). Table 2 demonstrates the measurements of corneal layer thickness and scleral thickness in the participants. The corneal layer thicknesses and scleral thicknesses were similar between the groups (p>0.05).
Age was not correlated with the corneal layer thickness or scleral thickness, as well as with the Schirmer’s test results, tear film thickness, and TBUT, when all of the participants were included in the analysis (p>0.05). Tear film thickness was moderately correlated with Schirmer’s test results (r=0.34, p=0.001; 95% confidence interval lower bound 0.14, upper bound 0.54), but was not correlated with TBUT (r=0.18, p=0.09; 95% confidence interval lower bound -0.03, upper bound 0.39). Tear film thickness was moderately negatively correlated with corneal epithelial thickness in the study group (r=-0.37, p=0.007; 95% confidence interval lower bound -0.62, upper bound -0.10), but not in the control group (r=-0.13, p=0.41; 95% confidence interval lower bound -0.52, upper bound 0.22). Scleral thickness measurements were not correlated with any of the analyzed parameters (p>0.05).
DISCUSSION
The present study’s outcomes showed that pre-ocular tear film, as measured by AS-OCT, was thinner in the patients with primary Sjögren’s syndrome than in the healthy control participants. Because tear film thickness measurement via AS-OCT is a non-invasive technique, it has the potential for more frequent use in dry-eye detection. Notably, Sjögren’s syndrome may affect the cornea and conjunctiva, in addition to the tear film; moreover, AS-OCT provides data regarding the cornea, conjunctiva, and sclera. Reduced tear production in patients with primary Sjogren’s syndrome has been documented frequently, but decreased pre-ocular tear film thickness on the corneal apex has not been reported previously.
Similar to previous reports(9-12), our study showed that Schirmer’s test results and TBUT scores were significantly lower in the patients with primary Sjögren’s syndrome than in the healthy control participants. As expected, the pre-ocular tear film was significantly thinner in patients with primary Sjögren’s syndrome; this finding also correlated with the Schirmer’s test results. Qiu et al. reported that tear meniscus height, as measured by OCT, was significantly lower in patients with primary Sjögren’s syndrome than in control participants(9). Utine et al. found that tear osmolarity values were higher in patients with primary Sjögren’s syndrome than in healthy individuals(11).
The cornea can be affected by primary Sjögren’s syndrome(13-22). However, the present study found that the corneal layer thickness in patients with primary Sjögren’s syndrome was similar to that in the healthy control participants. Villani et al. reported that central corneal thickness was significantly thinner in patients with primary Sjögren’s syndrome than in healthy individuals(14). Long et al. found that the corneas of patients with primary Sjögren’s syndrome tended to show less stiffness than those of dry-eye patients without primary Sjögren’s syndrome(15).
We measured anterior scleral thickness by using AS-OCT(23). Anterior scleral thickness measurements were similar between patients with primary Sjögren’s syndrome and healthy control participants in our study. In normal eyes, the sclera is thicker near the limbus than at the equator(24). The posterior sclera is thinner in eyes with greater axial length than in normal eyes(25). Vurgese et al. found that anterior scleral measurements did not correlate with corneal thickness measurements in healthy eyes(25).
Our study has several limitations. First, additional tear film examinations were not used, such as tear osmolarity, tear meniscus height, and Keratograph 5M. Second, we did not measure the peripheral cornea. Third, calculating palpebral fissure height and correlating it with the parameters studied here might provide more definitive conclusions, because tear film may be affected by palpebral fissure height. Finally, the spectral-domain OCT device used in this study had a 3.9-µm axial resolution, which may be insufficient to detect finer details of ocular structures. Werkmeister et al. found that central tear film thickness was approximately 5 µm when measured with an ultra-high-resolution spectral-domain OCT (i.e., a 1.2-µm axial resolution)(26).
In conclusion, measurements of corneal layer thickness and scleral thickness were similar between patients with primary Sjögren’s syndrome and healthy control participants. Tear film thickness, as measured by AS-OCT, was associated with the Schirmer’s test results, but not with TBUT. Further studies are needed to investigate the associations between tear film thickness and tear film meniscus height, as well as osmolarity, to gain a better understanding of this topic.
▪ Cornea/metabolism;
▪ Cornea/pathology*;
▪ Dry-eye syndromes/diagnosis*;
▪ Dry-eye syndromes/etiology;
▪ Female;
▪ Follow-Up studies;
▪ Humans;
▪ Male;
▪ Microscopy, confocal/methods*;
▪ Middle aged;
▪ Reproducibility of results;
▪ Retrospective studies;
▪ Sjogren’s syndrome/complications*;
▪ Sjogren’s syndrome/diagnosis;
▪ Sjogren’s syndrome/metabolism.
REFERENCES
1. Kuklinski E, Asbell PA. Sjogren’s syndrome from the perspective of ophthalmology. Clin Immunol. 2017;182:55-61.
2. Mavragani CP. Mechanisms and new strategies for primary Sjögren’s Syndrome. Annu Rev Med. 2017;68:331-43.
3. Both T, Dalm VA, van Hagen PM, van Daele PL. Reviewing primary Sjögren’s syndrome: beyond the dryness - From pathophysiology to diagnosis and treatment. Int J Med Sci. 2017;14(3):191-200.
4. Generali E, Costanzo A, Mainetti C, Selmi C. Cutaneous and mucosal manifestations of Sjögren’s Syndrome. Clin Rev Allergy Immunol. 2017;53(3):357-70.
5. Tepelus TC, Chiu GB, Huang J, Huang P Sadda SR, Irvine J, et al. Correlation between corneal innervation and inflammation evaluated with confocal microscopy and symptomatology in patients with dry eye syndromes: a preliminary study. Graefes Arch Clin Exp Ophthalmol. 2017;255(9):1771-8.
6. Kim M, Kim HS, Na KS. Correlation between tear osmolarity and other ocular surface parameters in primary Sjögren’s Syndrome. Korean J Ophthalmol. 2017;31(1):25-31.
7. Mocanu CL, Jurja S, Deca AG, Birjovanu F, Popa DG, Stefanescu-Dima AS, et al. Impression conjunctival cytology in sicca syndrome - correlations between clinical and histological findings related to dry eye severity. Rom J Morphol Embryol. 2016;57(1):197-203.
8. Franceschini F, Cavazzana I, Andreoli L, Tincani A. The 2016 classification criteria for primary Sjogren’s syndrome: what’s new? BMC Med. 2017;15(1):69.
9. Qiu X, Gong L, Lu Y, Jin H, Robitaille M. The diagnostic significance of Fourier-domain optical coherence tomography in Sjögren syndrome, aqueous tear deficiency and lipid tear deficiency patients. Acta Ophthalmol. 2012;90(5):e359-66.
10. Chen Q, Zhang X, Cui L, Huang Q, Chen W, Ma H, et al. Upper and lower tear menisci in Sjögren’s syndrome dry eye. Invest Ophthalmol Vis Sci. 2011;52(13):9373-8.
11. Utine CA, Bıçakçıgil M, Yavuz S, Çiftçi F. Tear osmolarity measurements in dry eye related to primary Sjögren’s syndrome. Curr Eye Res. 2011;36(8):683-90.
12. Denoyer A, Rabut G, Baudouin C. Tear film aberration dynamics and vision-related quality of life in patients with dry eye disease. Ophthalmology. 2012;119(9):1811-8.
13. Chen FY, Lee A, Ge S, Nathan S, Knox SM, McNamara NA. Aire-deficient mice provide a model of corneal and lacrimal gland neuropathy in Sjögren’s syndrome. PLoS One. 2017;12(9): e0184916.
14. Villani E, Galimberti D, Viola F, Mapelli C, Ratiglia R. The cornea in Sjogren’s syndrome: an in vivo confocal study. Invest Ophthalmol Vis Sci. 2007;48(5):2017-22.
15. Long Q, Wang JY, Xu D, Li Y. Comparison of corneal biomechanics in Sjögren’s syndrome and non-Sjögren’s syndrome dry eyes by Scheimpflug based device. Int J Ophthalmol. 2017;10(5):711-6.
16. Levy O, Labbé A, Borderie V, Hamiche T, Dupas B, Laroche L, et al. Increased corneal sub-basal nerve density in patients with Sjögren syndrome treated with topical cyclosporine A. Clin Exp Ophthalmol. 2017;45(5):455-63.
17. Lanza M, Iaccarino S, Varricchi G, D’Errico T, Gironi Carnevale UA, Bifani M. Corneal confocal microscopy alterations in Sjögren’s syndrome dry eye. Acta Ophthalmol. 2017;95(5):e366-e372.
18. McNamara NA, Ge S, Lee SM, Enghauser AM, Kuehl L, Chen FY, et al. Reduced levels of tear lacritin are associated with corneal neuropathy in patients with the ocular component of Sjögren’s Syndrome. Invest Ophthalmol Vis Sci. 2016;57(13):5237-43.
19. Mahelkova G, Jirsova K, Seidler Stangova P, Palos M, Vesela V, Fales I, et al. Using corneal confocal microscopy to track changes in the corneal layers of dry eye patients after autologous serum treatment. Clin Exp Optom. 2017;100(3):243-9.
20. Kheirkhah A, Rahimi Darabad R, Cruzat A, Hajrasouliha AR, Wikin D, Wong N, et al. Corneal epithelial immune dendritic cell alterations in subtypes of dry eye disease: a pilot in Vivo Confocal Microscopic Study. Invest Ophthalmol Vis Sci. 2015;56(12):7179-85.
21. Bianciardi G, Latronico ME, Traversi C. Entropy of corneal nerve fibers distribution observed by laser scanning confocal microscopy: A noninvasive quantitative method to characterize the corneal innervation in Sjogren’s syndrome patients. Microsc Res Tech. 2015;78(12):1069-74.
22. Machetta F, Fea AM, Actis AG, de Sanctis U, Dalmasso P, Grignolo FM. In vivo confocal microscopic evaluation of corneal langerhans cells in dry eye patients. Open Ophthalmol J. 2014;8:51-9.
23. Pekel G, Yağcı R, Acer S, Ongun GT, Çetin EN, Simavli H. Comparison of corneal layers and anterior sclera in emmetropic and myopic eyes. Cornea. 2015;34(7):786-90. Comment in: Cornea. 2015;34(9):e25-6.
24. Olsen TW, Aaberg SY, Geroski DH, Edelhauser HF. Human sclera: thickness and surface area. Am J Ophthalmol. 1998;125(2):237-41.
25. Vurgese S, Panda-Jonas S, Jonas JB. Scleral thickness in human eyes. PLoS One. 2012;7(1):e29692.
26. Werkmeister RM, Alex A, Kaya S, Unterhuber A, Hofer B, Riedl J, et al. Measurement of tear film thickness using ultrahigh-resolution optical coherence tomography. Invest Ophthalmol Vis Sci. 2013; 54(8):5578-83.
Submitted for publication:
May 18, 2018.
Accepted for publication:
November 22, 2018.
Approved by the following research ethics committee: Pamukkale University (# 60116787-020/21097).
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose