

Priscila C. Correa1; Felipe A. Medeiros2; Ricardo Y. Abe3; Alberto Diniz-Filho4; Carolina P. B. Gracitelli1
DOI: 10.5935/0004-2749.20190046
ABSTRACT
Glaucoma is the leading cause of irreversible blindness worldwide and can affect a broad array of daily activities, including driving. Recently, studies investigating the relationship between driving performance and glaucoma have received a great deal of interest. Assessment of driving behavior is not straightforward because driving is a complex skill involving significant multi-tasking ability. In this review, we summarize recent work from clinical studies investigating how glaucoma can affect driving performance. Patients with glaucoma are more likely to be involved in motor vehicle collisions when compared to healthy subjects. Here we describe how conventional functional tests performed in glaucoma patients, such as visual field measurements via standard automatic perimetry, are associated with driving performance. However, the risk of motor vehicle collisions is not entirely attributable to visual field impairment in glaucoma, suggesting that other factors also account for both driving safety and performance. Finally, we show different studies suggesting that parameters from driving simulators can be helpful because they can identify the impact of visual loss on complex situations.
Keywords: Glaucoma; Automobile driving; Quality of life; Visual field; Motor vehicle; Accidents, traffic
RESUMO
O glaucoma é a principal causa de cegueira irreversível em todo o mundo e pode afetar uma ampla gama de atividades diárias, incluindo a direção veicular. Recentemente, estudos que investigam a relação entre o desempenho na condução veicular e o glaucoma têm recebido grande interesse. A avaliação do comportamento de dirigir não é direta porque dirigir é uma habilidade complexa que envolve habilidade multitarefa significativa. Nesta revisão, resumimos trabalhos recentes de estudos clínicos que investigam como o glaucoma pode afetar o desempenho na direção. Pacientes com glaucoma têm maior probabilidade de se envolverem em colisões de veículos motorizados quando comparados a indivíduos saudáveis. Descrevemos aqui como os testes funcionais convencionais realizados em pacientes com glaucoma, como as medições de campo visual por meio de perimetria automática padrão, estão associados ao desempenho na direção. No entanto, o risco de colisão de veículo motorizado não é totalmente atribuível ao comprometimento do campo visual no glaucoma, sugerindo que outros fatores também são responsáveis pela segurança e pelo desempenho. Finalmente, mostramos diferentes estudos sugerindo que os parâmetros dos simuladores de direção podem ser úteis porque eles podem identificar o impacto da perda visual em situações de complexas.
Descritores: Glaucoma; Condução de veículo; Qualidade de vida; Campo visual; Veículos automotores; Acidentes de trânsito
INTRODUCTION
Glaucoma is the leading cause of irreversible blindness worldwide(1). In 2013, the number of people with glaucoma worldwide was estimated to be 64.3 million and was expected to increase to 111.8 million in 2040(1). Furthermore, studies have reported that 50% of cases remain undiagnosed in developed countries, although the figure could be as high as 90% in developing nations(2,3). The disease is characterized by progressive optic nerve damage that may result in irreversible loss of visual function and a significant decline in quality of life (QoL)(4).
Visual impairment from glaucoma can affect several aspects of one's QoL and impair performance on a broad array of activities of daily living, such as reading, walking, and driving. Inability to drive is a significant concern for patients with glaucoma, especially in regions where driving is fundamental for maintaining independent living and one's QoL. Several studies have reported that patients who stop driving may experience a higher number of depression symptoms, social isolation and reduced access to healthcare services, which can negatively affect their QoL(5-8). Although adequate vision is essential for driving, it is not clear which tests would be more accurate in predicting driving risk in subjects with visual disorders such as glaucoma. Although visual acuity is the most commonly performed visual parameter assessed by motor vehicle regulatory agencies for obtaining a driver's license, several studies have found little or no association between visual acuity and motor vehicle collisions (MVCs), clearly indicating the need for a more comprehensive assessment of visual performance concerning fitness to drive(9-13).
The gold standard test to evaluate functional damage in glaucoma is the visual field exam, most frequently performed with standard automated perimetry (SAP). However, previous studies have shown only a relatively weak association between SAP results in patients with glaucoma and risk of MVCs(14-20). Hypothetically, this weak association results from the artificial conditions in which visual field tests are performed, as they seek to minimize potential distractions to obtain reliable exams. However, this strategy provides unrealistic estimates of the amount of useful vision available when evaluating a multi-tasking ability such as driving(14-20). This suggest that other tests may, therefore, be better suited to assess the impact of glaucoma on driving fitness, including tests assessing visual processing under divided attention or more complex tests such as driving simulators.
This review analyze various methods of assessing the ability to drive in patients with glaucoma. Additionally, this review discusses the impact of visual disability on driving performance.
Glaucoma and MVCs
Traffic collisions caused by motor vehicles pose a significant public health problem(21). In 2009, the United States reported more than 10,000,000 traffic accidents with 35,000 deaths(21). A study of 10,000 drivers in California showed that individuals with severe bilateral visual field loss, primarily due to glaucoma, were twice more likely to be involved in MVCs than those with normal visual fields(22). Another study showed that drivers with glaucoma had a 65% higher risk of involvement in crashes in the first five years of follow-up than did patients without the disease(23).
In objective tests, studies with driving simulators showed that patients with glaucoma had worse driving performance than control individuals, which may suggest a relationship between visual function loss and MVCs. Results showed that a 90-degree binocular visual field restriction drastically reduced the ability to properly identify road signs and avoid obstacles, and increased the reaction time to visual stimuli(24,25). Several other studies which also sought to establish a link between MVCs and glaucoma reported a positive relationship between the disease and the risk of MVCs, thus corroborating the importance of establishing functional assessment criteria for glaucoma and its impact on the ability to drive(13,14,17,22).
In a subjective evaluation using self-reported questionnaires, patients with glaucoma reported greater difficulty driving than control individuals(26,27). Furthermore, the perceived difficulty increases with the worsening of the visual field in their better eye(28). The Salisbury Eye Evaluation (SEE) study revealed that individuals with binocular disease had the worst self-reported scores for night driving, suggesting that the disability may occur mainly in individuals with bilateral disease(29). Another study showed that self-reported ability to drive was worse in patients with a mean deviation from visual field lower than 12 dB in the worst eye (e.g. advanced glaucoma in the worst eye). However, the same study reported significant differences in the perceived ability to drive between individuals with treated and untreated ocular hypertension, suggesting that the difficulty may be more closely related to the perceived than actual disease severity(27). In a recent study, Correa and colleagues showed a weak relationship between subjective tests of the ability to drive and objective tests of driving performance in patients with glaucoma(30). In their study, only one-third of 76 glaucoma patients who were deemed unfit to drive on simulator testing had no concerns about their ability to drive. Moreover, in 17 patients with significant driving concerns, only 4 (24%) had clear evidence of unsatisfactory objective driving performance(30). This behavior poses a high risk to both the affected individual and society. Furthermore, many drivers lose awareness and perception of their driving performance because they slowly adapt to their declining abilities.
Conventional driving assessment methods
Functional impairment in glaucoma is traditionally measured using SAP and visual acuity measurement. In the United States, obtaining a driver's license from the responsible agency (Department of Motor Vehicles) is primarily based on visual acuity in most states and, in some cases, on visual field assessment(31).
The current Brazilian traffic legislation (Supplement 1) demands the evaluation of intrinsic and extrinsic ocular mobility, visual acuity, visual field, color vision, stereoscopic vision, glare test and night vision in the eye exam(32). In Brazil, visual acuity equal to or better than 0.50 (Snellen Table) in each eye or equal to or better than 0.66 in one eye, with horizontal isopter equal to or larger than 60º in each eye or equal to or larger than 120º in one eye, is required for a class "A" and "B" driver's license(32). Furthermore, a minimum visual acuity of 0.66 in each eye or equal to or better than 0.5 in the other eye, with a minimal binocular vision of 0.8, with 120º horizontal isopter in both eyes, is required for driving class "C," "D," and "E" vehicles(32). Each of these classes has exceptions (see Supplemental Material I).
Visual acuity and ability to drive
In a large study of 17,500 Californian drivers, visual acuity weakly correlated with the risk of MVCs, suggesting that poor visual acuity could not be used as a causal factor in crashes(33). In another cohort study of 3,158 individuals, a visual acuity of 20/40 or worse was not associated with the risk of a motor vehicle collision(12).
Recently, a prospective, multicenter study showed that the visual acuity of the worst eye is a significant risk factor for MVCs in patients with primary open-angle glaucoma(34). Conversely, Gracitelli and colleagues found in a prospective study that the visual acuities of both best and worst eye were not predictive factors of MVCs(35). One of the reasons that visual acuity may not be a significant predictive factor for MVCs in previous studies is that people with poor visual acuity are not licensed to drive. Additionally, people with poor visual acuity usually quit driving, therefore, most studies were likely biased by these facts.
Visual field and ability to drive
Although the presence of bilateral visual field defects has been associated with an increased risk of MVCs, some studies have failed to report a clear association between visual field loss and rates of MVCs(10,36). Moreover, there is no agreement on the type or severity of the visual field defect that would be associated with an increased risk of MVCs. Indeed, the specific visual field requirements for a driver's license are highly variable in different countries. Interestingly, Haymes et al., showed a higher rate of MVCs among individuals with glaucoma, even after adjusting for visual field loss(14). Therefore, it is plausible to suggest that the risk of MVCs may not be fully attributed to visual field defects, suggesting that other factors could also account for increased rates of collisions in these patients.
In another study, Haymes et al., investigated driving behaviors from 20 glaucoma patients, with visual acuity, contrast sensitivity and SAP. They found that patients with mild-to-moderate glaucoma performed driving maneuvers safely, although they were six times more likely to require driving instructor intervention, due to difficulty in detecting peripheral obstacles and in responding to unexpected events(37). Furthermore, although with a limited sample size and limited patients profile (general relatively mild/moderate disease), the aforementioned study conducted by Gracitelli and colleagues showed that visual field loss was not a predictive factor for the risk of traffic collision among patients with glaucoma(35). These findings indicate that the ability to drive is a complex task involving the simultaneous use of central and peripheral vision, attention shift, dynamic spatial orientation, kinetic depth perception and assessment of dangerous occurrences(31). Conventional tests, including the Snellen chart or visual field assessment, seek to minimize the distractions and demands of secondary tasks. Therefore, unsurprisingly, these tests are not strong predictors for safe driving.
Useful field of view (UFOV)
Driving involves simultaneous use of central and peripheral vision while performing primary and secondary tasks, both visual and nonvisual(31). When a vehicle is in motion, the perception of the environment changes rapidly, and the driver has to maintain awareness as to when and where a critical event might occur(31). This fact has led several researchers to study the relationships between safe driving, performance and attention-related abilities(31). The ability to divide attention requires the ability to respond to information from one task while simultaneously performing another, such as monitoring information from the roadway to control the vehicle, while simultaneously maintaining awareness of potential hazards surrounding the vehicle(38).
The useful field of view (UFOV - Visual Awareness, Inc., Chicago, IL, USA) is a computerized test developed by Ball et al.(39). In brief, the subtests include processing speed, divided attention, and selective visual attention. Visual processing speed is initially evaluated by instructing the subject, using both eyes, to discriminate a foveal or central vision target (image of a car or truck) located in the center of a 17-inch touchscreen (subtending a 3 x 5 degree visual angle). Recognition of the target is then registered by asking the subject to touch the screen to indicate which target was shown. During the test, the presentation time is increased following an incorrect response and decreased following a correct response so that the test results can be presented as the time needed to achieve a stable 75% accuracy for detection. The processing speed test is followed by a second test called divided attention test. The participants are asked to identify a silhouette of a 2 cm by 1.5 cm truck or car (2 choices) that appears in a box in the center of a 17-inch touchscreen monitor, in addition to a concurrent peripheral localization task consisting of an image of a car presented on one of eight radial spokes at a fixed eccentricity of approximately 11 degrees. The subject is then asked to identify the central target and identify on which spoke the peripheral object was located. The test proceeds with decreasing presentation times, ranging from 500 ms to 17 ms, until the presentation time that results in a 75% accurate response can be recorded. Finally, in the selective visual attention subtest, the subject indicates the radial direction of the peripheral target even though it is embedded in other distracting stimuli in the periphery. Figure 1 shows one of the steps of the UFOV test.
Different studies have observed an association between MVCs and the results of the UFOV test(10,12,13). For example, Bentley et al., found that the UFOV may be adequate in terms of validation and reliability in assessing normal subjects and patients with visual field changes; however, they also found a moderate degree of variability and significant learning effects in the test(40). A meta-analysis demonstrated the importance of this test for driving performance and safety, due to the relationship between UFOV performance and future MVCs, suggesting the use of this tool as a potential screening method for elderly drivers(41).
Driving simulators
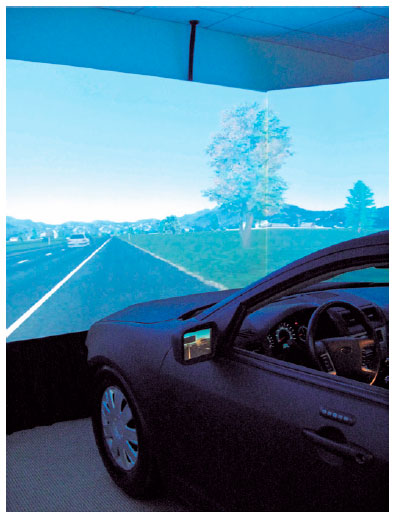
The applicability of the use of driving simulators has been studied in a wide variety of situations, including traumatic brain injury, Alzheimer's disease, Parkinson's disease and attention deficit disorders, as well as to assess the effects of distracting situations, such as cell phone, alcohol or drug use on driving behavior(42-52). Specifically, for glaucoma, different studies have found good applicability for driving simulators. For example, Medeiros and colleagues developed a driving simulator for the functional assessment of drivers with different eye conditions(53) (Figure 2).
Driving simulators can measure different tasks with or without divided attention. In summary, divided attention requires processing and responding to information about one task while conducting another. Specifically, in driving, divided attention involves continuously monitoring information from the roadway to control the vehicle, while simultaneously keep awareness of potential hazards surrounding the vehicle. As the cognitive system has a limited amount of attentional resources, the efficiency of performance of a task may be compromised if performed under a divided attention situation. Therefore, the ability to divide attention is related to the ability to drive(54).
The ability to divide attention between the central driving task and the peripheral detection task is assessed by measuring reaction times to the distraction stimuli presented peripherally. The peripheral stimuli are presented at about 20-degrees of visual angle in the upper right and upper left of the driving simulator screen and at three different contrasts (low, medium and high). The contrast of the stimulus is randomly altered. There are many different tests such as car following, curve negotiation (Figure 3) or stop signs that can be done on the simulator the measure divided attention.

Based on the divided attention test, Tatham and colleagues assessed the relationship between glaucomatous structural damage and the divided attention ability in a driving simulator. They found that in 82 patients with glaucoma and 76 similarly aged controls, the retinal nerve fiber layer measured by optical coherence tomography provides information in addition to functional tests, such as visual field, suggesting that structural measurements also have the potential to assess whether patients may have problems in daily activities, such as driving(55).
Another study compared the relationships between MVCs, SAP, UFOV and the driving simulator in assessing divided attention ability. They concluded that the reaction times in low-contrast conditions in divided attention tasks are more strongly related to MVCs in the driving simulator than in conventional perimetry tests and the UFOV(20). Moreover, Gracitelli and colleagues conducted a longitudinal study that showed the capacity of the UFOV and the driving simulator to predict the occurrence of traffic collisions extracted from DMV records among patients with glaucoma(35). These two tests were more strongly correlated with the risk of traffic collision among patients with glaucoma than conventional tests, including visual acuity and visual field. These findings may help to understand factors related to MVCs and glaucoma. A further longitudinal study with driving by Diniz-Filho et al. evaluated the relationship between driving performance and rates of progressive visual field loss in patients with glaucoma(56). They showed that fast visual field progression was correlated with worsening performance on a divided attention task in driving simulators. Therefore, patients who presented faster visual field progression may be at greater risk of decline in driving performance(56).
Several scenarios may also be recreated in the simulator to test different tasks including modifying and adjusting the vehicle direction and speed. Position on the road, interaction with traffic stimuli, changes in weather and light conditions, merging into traffic, negotiating curves, passing into oncoming traffic, maintaining safe following distance, and response to errors by others (e.g., sudden appearance of pedestrians or cars in the central or peripheral field of view). These scenarios may be customized depending on the driving behavior that is under investigation(53). This tool also has the advantage of making it possible to perform controlled experiments that are repeated numerous times in different types of scenarios with standardized results to assess a specific behavior or task separately(53). For example, using repeated scenarios Adler and colleagues showed that drivers with glaucoma are more susceptible to changing their night driving habits on roads in unknown areas, indicating that the simulator may resemble reality(57). In another recent study, Diniz-Filho and colleagues found that patients with glaucoma had a higher risk of MVCs during foggy conditions than healthy individuals from the control group in a driving simulator, with a higher risk in patients with a mean deviation from visual field lower than -9 dB(58).
Driving simulators still have some limitations, despite their potential for creating realistic and standardized scenarios. For example, study subjects may behave differently in real life than when they are exposed to artificial scenarios. Furthermore, these tools may have a relatively long learning curve, and can sometimes create discomfort during the test(35).
CONCLUSION
Glaucoma is a progressive optic neuropathy that leads to significant losses in visual function and the ability to perform activities of daily living, such as driving. The tests currently available for assessing the risk of vision-related disabilities such as visual acuity or SAP are still limited. Certainly, on-road driving assessment is the best test of ability to drive, but such tests can be challenging to standardize and difficult to evaluate regarding how drivers safely deal with hazards. In this context, although they are not widely available to clinicians, driving simulations may be an excellent tool to assess an individual's actual ability to drive. In addition, other tests such as UFOV may present a good association with MVCs.
REFERENCES
1. Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081-90.
2. Wensor MD, McCarty CA, Stanislavsky YL, Livingston PM, Taylor HR. The prevalence of glaucoma in the Melbourne Visual Impairment Project. Ophthalmology. 1998;105(4):733-9.
3. Coffey M, Reidy A, Wormald R, Xian WX, Wright L, Courtney P. Prevalence of glaucoma in the west of Ireland. Br J Ophthalmol. 1993;77(1):17-21.
4. Medeiros FA, Gracitelli CP, Boer ER, Weinreb RN, Zangwill LM, Rosen PN. Longitudinal changes in quality of life and rates of progressive visual field loss in glaucoma patients. Ophthalmology. 2015;122(2):293-301.
5. DeCarlo DK, Scilley K, Wells J, Owsley C. Driving habits and health-related quality of life in patients with age-related maculopathy. Optom Vis Sci. 2003;80(3):207-13.
6. Ragland DR, Satariano WA, MacLeod KE. Driving cessation and increased depressive symptoms. J Gerontol A Biol Sci Med Sci. 2005;60(3):399-403.
7. Fonda SJ, Wallace RB, Herzog AR. Changes in driving patterns and worsening depressive symptoms among older adults. J Gerontol B Psychol Sci Soc Sci. 2001;56(6):S343-51.
8. Marottoli RA, Mendes de Leon CF, Glass TA, Williams CS, Cooney LM Jr, Berkman LF, et al. Driving cessation and increased depressive symptoms: prospective evidence from the New Haven EPESE. Established Populations for Epidemiologic Studies of the Elderly. J Am Geriatr Soc. 1997;45(2):202-6.
9. Owsley C, Stalvey BT, Wells J, Sloane ME, McGwin G Jr. Visual risk factors for crash involvement in older drivers with cataract. Arch Ophthalmol. 2001;119(6):881-7.
10. Owsley C, Ball K, McGwin G Jr, Sloane ME, Roenker DL, White MF, et al. Visual processing impairment and risk of motor vehicle crash among older adults. JAMA. 1998;279(14):1083-8.
11. McCloskey LW, Koepsell TD, Wolf ME, Buchner DM. Motor vehicle collision injuries and sensory impairments of older drivers. Age Ageing. 1994;23(4):267-73.
12. Cross JM, McGwin G Jr, Rubin GS, Ball KK, West SK, Roenker DL, et al. Visual and medical risk factors for motor vehicle collision involvement among older drivers. Br J Ophthalmol. 2009;93(3):400-4.
13. Rubin GS, Ng ES, Bandeen-Roche K, Keyl PM, Freeman EE, West SK. A prospective, population-based study of the role of visual impairment in motor vehicle crashes among older drivers: the SEE study. Invest Ophthalmol Vis Sci. 2007;48(4):1483-91.
14. Haymes SA, Leblanc RP, Nicolela MT, Chiasson LA, Chauhan BC. Risk of falls and motor vehicle collisions in glaucoma. Invest Ophthalmol Vis Sci. 2007;48(3):1149-55.
15. Jampel HD. Glaucoma patients' assessment of their visual function and quality of life. Trans Am Ophthalmol Soc. 2001;99:301-17.
16. Tanabe S, Yuki K, Ozeki N, Shiba D, Abe T, Kouyama K, et al. The association between primary open-angle glaucoma and motor vehicle collisions. Invest Ophthalmol Vis Sci. 2011;52(7):4177-81.
17. McGwin G Jr, Xie A, Mays A, Joiner W, DeCarlo DK, Hall TA, et al. Visual field defects and the risk of motor vehicle collisions among patients with glaucoma. Invest Ophthalmol Vis Sci. 2005; 46(12):4437-41.
18. Owsley C, Stalvey B, Wells J, Sloane ME. Older drivers and cataract: driving habits and crash risk. J Gerontol A Biol Sci Med Sci. 1999;54(4):M203-11.
19. Richman J, Lorenzana LL, Lankaranian D, Dugar J, Mayer JR, Wizov SS, et al. Relationships in glaucoma patients between standard vision tests, quality of life, and ability to perform daily activities. Ophthalmic Epidemiol. 2010;17(3):144-51.
20. Tatham AJ, Boer ER, Gracitelli CP, Rosen PN, Medeiros FA. Relationship Between Motor Vehicle Collisions and Results of Perimetry, Useful Field of View, and Driving Simulation in Drivers With Glaucoma. Transl Vis Sci Technol. 2015;4(3):5.
21. Transporation: Motor Vehicle Accidents and Fatalities. Table 1103. Motor Vehicle Accidents-Number and Deaths: 1990-2009. In: commerce Do, ed. http://www.census.gov/compendia/statab/2012/tables/12s1103.pdf
22. Johnson CA, Keltner JL. Incidence of visual field loss in 20,000 eyes and its relationship to driving performance. Arch Ophthalmol. 1983;101(3):371-5.s
23. Kwon M, Huisingh C, Rhodes LA, McGwin G Jr, Wood JM, Owsley C. Association between Glaucoma and At-fault Motor Vehicle Collision Involvement among Older Drivers: A Population-based Study. Ophthalmology. 2016;123(1):109-16.
24. Wood JM, Troutbeck R. Effect of restriction of the binocular visual field on driving performance. Ophthalmic Physiol Opt. 1992;12(3):291-8.
25. J. WM. R. T. The effect of artificial visual impairment on functional visual fields and driving performance. Clin Vis Sci. 1993;8:563-75.
26. Gutierrez P, Wilson MR, Johnson C, Gordon M, Cioffi GA, Ritch R, et al. Influence of glaucomatous visual field loss on health-related quality of life. Arch Ophthalmol. 1997;115(6):777-84.
27. Béchetoille A, Arnould B, Bron A, Baudouin C, Renard JP, Sellem E, et al. Measurement of health-related quality of life with glaucoma: validation of the Glau-QoL 36-item questionnaire. Acta Ophthalmol. 2008;86(1):71-80.
28. Parrish RK 2nd, Gedde SJ, Scott IU, Feuer WJ, Schiffman JC, Mangione CM, et al. Visual function and quality of life among patients with glaucoma. Arch Ophthalmol. 1997;115(11):1447-55.
29. Freeman EE, Muñoz B, West SK, Jampel HD, Friedman DS. Glaucoma and quality of life: the Salisbury Eye Evaluation. Ophthalmology. 2008;115(2):233-8.
30. Correa PC, Gracitelli CP, Boer E, et al. Relationship between Subjective Driving Concerns and Objective Driving Performance on a Simulator in Patients with Glaucomatous Visual Field Loss. ARVO Annual Meeting. Denver, CO, USA; 2016.
31. Owsley C, McGwin G Jr. Vision and driving. Vision Res. 2010;50(23):2348-61.
32. Conselho Nacional de Trânsito - CONTRAN CNdT-. Artigo 147, I e §§ 1º a 4º e o artigo 148 do Código de Trânsito Brasileiro. Lei 9503/97, de 23 de Setembro de 1997. Brasília (DF): CONTRAN; 1997.
33. Hills BL, Burg A. A reanalysis of California driver vision data: General findings. Crowthorn, England: Transport and Road Research Laboratory; 1977.
34. Yuki K, Awano-Tanabe S, Ono T, Shiba D, Murata H, Asaoka R, et al. Risk factors for motor vehicle collisions in patients with primary open-angle glaucoma: a multicenter prospective cohort study. PLoS One. 2016;11(11):e0166943.
35. Gracitelli CP, Tatham AJ, Boer ER, Abe RY, Diniz-Filho A, Rosen PN, et al. Predicting Risk of Motor Vehicle Collisions in Patients with Glaucoma: A Longitudinal Study. PLoS One. 2015; 10(10):e0138288.
36. Decina LE, Staplin L. Retrospective evaluation of alternative vision screening criteria for older and younger drivers. Accid Anal Prev. 1993;25(3):267-75.
37. Haymes SA, LeBlanc RP, Nicolela MT, Chiasson LA, Chauhan BC. Glaucoma and on-road driving performance. Invest Ophthalmol Vis Sci. 2008;49(7):3035-41.
38. Lee HC, Lee AH, Cameron D, Li-Tsang C. Using a driving simulator to identify older drivers at inflated risk of motor vehicle crashes. J Safety Res. 2003;34(4):453-9.
39. Ball K, Owsley C. The useful field of view test: a new technique for evaluating age-related declines in visual function. J Am Optom Assoc. 1993;64(1):71-9.
40. Bentley SA, LeBlanc RP, Nicolela MT, Chauhan BC. Validity, reliability, and repeatability of the useful field of view test in persons with normal vision and patients with glaucoma. Invest Ophthalmol Vis Sci. 2012;53(11):6763-9.
41. Clay OJ, Wadley VG, Edwards JD, Roth DL, Roenker DL, Ball KK. Cumulative meta-analysis of the relationship between useful field of view and driving performance in older adults: current and future implications. Optom Vis Sci. 2005;82(8):724-31.
42. Lew HL, Rosen PN, Thomander D, Poole JH. The potential utility of driving simulators in the cognitive rehabilitation of combat-returnees with traumatic brain injury. J Head Trauma Rehabil. 2009;24(1):51-6.
43. Rizzo M, McGehee DV, Dawson JD, Anderson SN. Simulated car crashes at intersections in drivers with Alzheimer disease. Alzheimer Dis Assoc Disord. 2001;15(1):10-20.
44. Rizzo M, Reinach S, McGehee D, Dawson J. Simulated car crashes and crash predictors in drivers with Alzheimer disease. Arch Neurol. 1997;54(5):545-51.
45. Reinach SJ, Rizzo M, McGehee DV. Driving with Alzheimer disease: the anatomy of a crash. Alzheimer Dis Assoc Disord. 1997;11 Suppl 1:21-7.
46. Klimkeit EI, Bradshaw JL, Charlton J, Stolwyk R, Georgiou-Karistianis N. Driving ability in Parkinson's disease: current status of research. Neurosci Biobehav Rev. 2009;33(3):223-31.
47. Uc EY, Rizzo M, Anderson SW, Dastrup E, Sparks JD, Dawson JD. Driving under low-contrast visibility conditions in Parkinson disease. Neurology. 2009;73(14):1103-10.
48. Devos H, Vandenberghe W, Nieuwboer A, Tant M, Baten G, De Weerdt W. Predictors of fitness to drive in people with Parkinson disease. Neurology. 2007;69(14):1434-41.
49. Biederman J, Fried R, Monuteaux MC, Reimer B, Coughlin JF, Surman CB, et al. A laboratory driving simulation for assessment of driving behavior in adults with ADHD: a controlled study. Ann Gen Psychiatry. 2007;6(1):4.
50. Strayer DL, Drews FA, Crouch DJ. A comparison of the cell phone driver and the drunk driver. Hum Factors. 2006;48(2): 381-91.
51. Hughes DT, Cramer F, Knight GJ. Use of a racing car simulator for medical research the effects of marzine and alcohol on driving performance. Med Sci Law. 1967;7(4):200-4.
52. Gawron VJ, Ranney TA. The effects of alcohol dosing on driving performance on a closed course and in a driving simulator. Ergonomics. 1988;31(9):1219-44.
53. Medeiros FA, Weinreb RN, R Boer E, Rosen PN. Driving simulation as a performance-based test of visual impairment in glaucoma. J Glaucoma. 2012;21(4):221-7.
54. Ball K, Owsley C, Sloane ME, Roenker DL, Bruni JR. Visual attention problems as a predictor of vehicle crashes in older drivers. Invest Ophthalmol Vis Sci. 1993;34(11):3110-23.
55. Tatham AJ, Boer ER, Rosen PN, Della Penna M, Meira-Freitas D, Weinreb RN, et al. Glaucomatous retinal nerve fiber layer thickness loss is associated with slower reaction times under a divided attention task. Am J Ophthalmol. 2014;158(5):1008-17.
56. Diniz-Filho A, Tatham AJ, Boer ER, Gracitelli CP, Abe RY, Medeiros FA. Rates of progressive visual field loss and driving performance in glaucoma. ARVO paper presentation 2018.
57. Adler G, Bauer MJ, Rottunda S, Kuskowski M. Driving habits and patterns in older men with glaucoma. Soc Work Health Care. 2005;40(3):75-87.
58. Diniz-Filho A, Boer ER, Elhosseiny A, Wu Z, Nakanishi M, Medeiros FA. Glaucoma and Driving Risk under Simulated Fog Conditions. Transl Vis Sci Technol. 2016;5(6):15.
SUPPLEMENT 1
Ophthalmologic evaluation
1. Visual acuity and camp test:
1.1. The requirement for vehicle direction candidates of category C, D, E
1.1.1. Central visual acuity similar or higher than 20/30 (equivalent of 0.66) in each eye; or similar or upper than 20/30 (equivalent of 0.66) in one eye and similar or upper than 20/40 (equivalent of 0.50) on the other eye, with 20/25 as minimum binocular eyesight (equivalent of 0.80);
1.1.2. Peripheral eyesight in horizontal isoptera similar or higher than 120º in each eye.
1.2. The requirement for ACC candidates and vehicles direction of category A and B.
1.2.1. Central visual acuity similar or higher than 20/40 (equivalent of 0.50) in each eye; or similar or higher than 20/30 (equivalent of 0.66) in one eye with at least bright perception in the other eye.
1.2.2. Peripheral eyesight in horizontal isoptera similar or upper than 60º in each eye; or similar or upper than 120º in one eye.
1.3. Candidates with no bright perception in one eye can be approved in ACC, A and B categories, since observed the following parameters and provisos:
1.3.1. Central visual acuity similar or upper than 20/30 (equivalent of 0,66);
1.3.2. Peripheral eyesight in horizontal isoptera similar or upper than 120º;
1.3.3. After at least ninety days of loss eyesight, the medical report have to indicate the use of safety helmet and visors with no visual camp limitation.
1.4. The required acuity can be achieved with or without optical correction. In this case, it must have the observation "it is mandatory the use of corrective lenses" on the driver license. Intraocular lenses are not included on this obligation.
2. Ocular motility, tropia:
2.1. The person who has strabismus can be approved only in ACC and A and B categories, according to the following parameters:
2.1.1. Central visual acuity similar or upper than 20/30 (equivalent of 0,66) in the lower eye;
2.1.2. Peripheral eyesight in horizontal isoptera similar or upper than 120º in at least one eye.
3. Color vision test:
3.1. Vehicles direction candidates have to be able to recognize the standing position traffic lights, according to the Brazilian Traffic Code.
4. The threshold night vision and glare reaction test:
4.1. The candidate have to have vision on low light and recuperation after direct threshold.
Submitted for publication:
July 27, 2018.
Accepted for publication:
October 19, 2018.
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: Priscila C. Correa, None; Felipe A. Medeiros, F (Financial Support) Alcon Laboratories Inc.; Allergan Inc.; Bausch & Lomb; Carl Zeiss Meditec Inc.; Heidelberg Engineering Inc.; Merck Inc.; National Eye Institute; Sensimed AG; Topcon Inc.; R (Recipient) Alcon Laboratories Inc.; Allergan Inc.; Carl Zeiss Meditec Inc.; Reichert Inc.; C (Consultant) Allergan Inc.; Carl Zeiss Meditec Inc.; Novartis; Ricardo Y. Abe, None; Alberto Diniz-Filho