

Galina Dimitrova1; Ana Gjorgjioska1; Tatjana Ilievska2; Emilija Grkova-Mishkovska2; Antonela Ljubic3; Merjem Purelku4; Dragan Andonovski1; Sasho Stojcev5
DOI: 10.5935/0004-2749.20190017
INTRODUCTION
The therapeutic effect of infra-red light (IRL) to the human body was attributed to both its heating and biomodulating properties(1). Temperature was reported to affect intra-ocular pressure (IOP). Increased body temperature decreased IOP(2) and in summer, mean IOP was lower than during winter season(3). In this original, controlled and masked within-participant pilot study we aim to study the effect of IRL on intraocular pressure.
METHODS
The ethics committee of our hospital approved our study and the study was in accordance with the tenets of the Declaration of Helsinki. Initially the study included 34 healthy subjects (age 24-59) who all signed informed consent before participation. Exclusion criteria were: systemic diseases, ametropia >6D, IOP >21 mmHg, ocular acute or chronic pathology and any intraocular surgery. Best corrected visual acuity, auto-referactometry, slit-lamp biomicroscopy, blood pressure (automated sphygmomanometer-Sanitas) and IOP (Goldman applanation tonometry (AT)) was performed in all participants. The IOP measurement was recorded after averaging at least two measurements with the AT. Two subjects were excluded because of IOP >21 mmhg. One (right) eye per patient was included in the study. After the initial examinations, subjects were assigned to either group A (n=17) subjected to IRL radiation or group B (n=17) not subjected to IRL radiation. The IRL radiation involved 15 minutes of continuous effect of a 150 W IRL bulb (General Electric E27 that emits mixed IRL with mainly shorter wavelengths (mid IRL, near IRL and visible red light)) on a distance of 40 cm. Participants who did not receive any IRL radiation spent equal time in the same conditions as participants in group A. Immediately after the procedure subjects had their IOP measured again by Goldman AP by a masked examiner (GD). We used unpaired t-test to analyze statistical differences between group A and group B and paired t-test to analyze the differences between the first and the second IOP measurement in each patient group. P values <0.05 were considered as statistically significant.
RESULTS
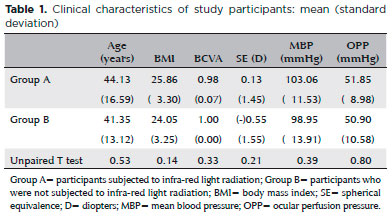
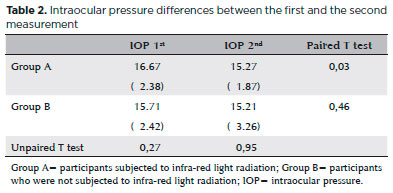
Table 1 shows data from subjects’ clinical characteristics. There were no significant differences between the groups in terms of demographic and clinical characteristics. IOP was not significantly different between the two groups (p=0.27). In Group A IOP from the second measurement (mean 15.27 mmHg; SD 1.87 mmHg) was significantly decreased than the IOP from the first measurement (mean 16.67 mmHg; SD 2.38 mmHg; p=0.03). In Group B IOP from the second measurement (mean 15.21 mmHg; SD 3.26 mmHg) was not significantly different than the IOP from the first measurement (mean 15.71 mmHg; SD 2.42 mmHg; p=0.46) (Table 2).
DISCUSSION
The results from this study suggest that after exposition to 15 minutes of IRL radiation the IOP decreases in healthy subjects. There may be two causes for such an outcome – heating effect of IRL and/or photobiomodulatory effect of IRL.
The effect of heat on IOP has not been studied in detail. A significant decrease of IOP was detected after 20 minutes of immersion of whole body in hot water (39 degrees C)(2). Locally applied eyelid warming device tended to decrease IOP in patients with meibomian gland dysfunction(4). Changes of IOP with season have also been reported, with increased IOP during winter season in healthy subjects and in patients with ocular hypertension(3,5). In the current study the decrease of IOP may have been caused by the dissipated heat from the IRL bulb that may have increased body temperature in the head and shoulder region where the IRL radiation was applied. The effect may have also been caused by a local increase in ocular and orbital temperature that may have changed ocular hemodynamic and/or corneal/sclera stiffness. Except for the heating effect, IRL was also shown to have an effect on the biological tissue by absorption of light rays by mitochondrial chromophores that may have affected the IOP(1).
Limitations of this study include small number of participants and lack of corneal pachymetry and corneal hysteresis measurements in order to study the possible effect of IRL to the corneal tissue. We also did not measure body temperature before and after IRL radiation in order to discern the effect of body temperature to IOP. However, to our knowledge this is the first study on the effect of IRL to IOP. Further studies are necessary to confirm our results and to study the long-term effect of IRL to IOP.
REFERENCES
1. Vatansever F, Hamblin M. Far infrared radiation (FIR): its biological effects and medical applications Photonics Lasers Med. 2012;4: 255-66.
2. Findikoglu G, Cetin EN, Sarsan A, Senol H, Yildirim C, Ardic F. Arterial and intraocular pressure changes after a single-session hot-water immersion. UnderseaHyperb Med. 2015;42(1):65-73.
3. Cheng J, Xiao M, Xu H, Fang S, Chen X, Kong X, Sun X. Seasonal changes of 24-hour intraocular pressure rhythm in healthy Shanghai population. Medicine (Baltimore).2016;95(31):e4453.
4. Purslow C. Evaluation of the ocular tolerance of a novel eyelid warming device used for meibomian gland dysfunction. ContLens Anterior Eye. 2013;36(5):226-31.
5. Qureshi IA, Xiao RX, Yang BH, Zhang J, Xiang DW, Hui JL. Seasonal and diurnal variations of ocular pressure in ocular hypertensive subjects in Pakistan. Singapore Med J. 1999;40(5):345-8.
Submitted for publication:
May 15, 2018.
Accepted for publication:
September 20, 2018.
Approved by the following research ethics committee: City General Hospital “8th September”, Skopje, Republic of Macedonia (# 248/2016).
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose