

Patrícia Ioschpe Gus1; Bruno Schneider de Araújo1; Samira Zelanis2; Tiago Ribeiro Schmalfuss3; Diane Ruschel Marinho2
DOI: 10.5935/0004-2749.20190014
ABSTRACT
The authors describe an unusual association between posterior keratoconus and iris atrophy, confirmed by a complete ocular evaluation, scheimpflug imaging and pachymetric curve. A hypothesis for concomitant findings is discussed.
Keywords: Keratoconus; Iris; Atrophy; Iridocorneal endothelial syndrome; Humans; Case reports
RESUMO
Os autores descrevem a rara associação entre ceratocone posterior e atrofia de íris, confirmada por avaliação oftalmológica completa, imagens de scheimpflug e curva paquimétrica. Sugere-se uma hipótese que explique a concomitância de ambas as alterações.
Descritores: Ceratocone; Iris; Atrofia; Síndrome endotelial iridocorneana; Humanos; Relatos de casos
INTRODUCTION
Posterior keratoconus is a rare corneal disease with no relation to anterior keratoconus(1). First described in 1930, the disease is characterized by a sporadic, unilateral, rounded, central, and nonprogressive abnormality(2). It is characterized by conical protrusion of the posterior curvature and stromal thinning, affecting the anterior curvature in some cases(3). The etiology and pathogenesis of the disease are unknown. Posterior keratoconus is thought to represent a slight variation of Peters anomaly or an abnormal migration or differentiation of secondary mesenchyme cells(4), and embryologic similarities may explain the reduced iris thickness in keratoconus patients(5). In addition to stromal thinning and irregularities, the affected area may exhibit excrescences or thinning of the Descemet’s membrane, as well as endothelium abnormalities. Vision can be compromised by refractive error, stromal opacification, or amblyopia but is sometimes unaffected(6). Both keratoconus and subclinical keratoconus can be diagnosed with the Pentacam system(7).
There is no clear association between posterior keratoconus and other ocular comorbidities. We report a case of unilateral posterior keratoconus, high refractive myopic astigmatism, severe amblyopia, and mild iris atrophy. The patient was carefully evaluated using Scheimpflug tomography.
CASE REPORT
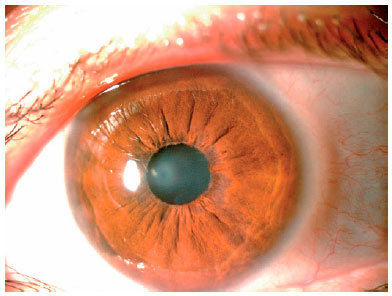
We describe a case of posterior keratoconus in a 47-year-old female patient. The best-corrected visual acuity measured using Snellen notation was 20/40 with -9.00 sph in the right eye and hand motion perception with correction of -14.00 × -10,00 115 in the left eye. Slit lamp biomicroscopy showed remarkable corneal thinning with anterior protrusion and posterior corneal surface curving, central leucoma, and peripupillary iris atrophy (Figure 1). No abnormalities were observed in the anterior chamber architecture. An intraocular pressure of 13 mmHg in the right eye and 19 mmHg in the left eye was recorded with Goldman applanation tonometry, with a maximum pressure of 22 mmHg in the left eye when measured on a different day. Gonioscopy was normal. Peripapillary atrophy and tilted optic cups were found during fundus examination. Glaucoma evaluation with optical coherence tomography and automated perimetry did not yield a diagnosis because there was no loss of optic nerve fibers, and perimetric evaluation was not useful because of severe amblyopia and poor light sensitivity in the left eye. The results of Scheimpflug tomography Pentacam® central 4 mm keratometry were 41 @ 116.5 and 48 @ 26.5. A Holladay map revealed a delimited, nummular, posterior protrusion corresponding to pachymetry thinning, very high posterior elevation, and anterior sagittal astigmatism. Belin-Ambrósio software for keratoconus detection showed an inverse curve compared with anterior keratoconus, starting with very low central pachymetry values (248 M), which normalized toward the periphery (Figure 2). The anterior elevation map was also abnormal, with irregular astigmatism of 7D (Figure 3). Fundoscopy was compatible with high myopia and revealed rarefaction of the retinal pigment epithelium and peripapillary atrophy in both eyes. Slit lamp and Scheimpflug examinations were normal in the left eye.
DISCUSSION
We describe an infrequent association between posterior keratoconus and iris atrophy with high myopic astigmatism that resulted in high refractive amblyopia. Scheimpflug images with Belin-Ambrósio software evaluation are described first, and we will attempt to establish a relationship between the cornea and iris alterations in one eye.
Endothelial cells, iris stromal cells, and corneal stromal keratocytes are embryologically derived from migrating neural crest cells. We propose an adaptation of the hypothesis of Blair et al.(8) to explain concurrent mild iris atrophy as a “forme frustre” of iridocorneal endothelial (ICE) syndrome in a posterior keratoconic eye. Predisposition for each condition may be inherited as an inactive germline allele, the so-called first hit, which is similar to the genetic mechanisms proposed for retinoblastoma. Inactivation of the second allele, or the second hit, which can occur at any time before or during embryogenesis, may be the product of background mutation or an environmental trigger. The source of the second hit or trigger remains unclear. Alvarado et al. first postulated a viral etiology for the pathogenesis of ICE syndrome, specifically herpes zoster or herpes simplex, since these viruses are known to affect Descemet’s membrane and are primarily unilateral(9).
We agree that unilateral abnormalities are more amblyogenic than rare bilateral conditions. In this patient, proximity to the visual axis, corneal haze, and the degree of corneal astigmatism may have contributed to amblyopia. Contrary to earlier beliefs, anterior corneal surface changes do occur in posterior keratoconus and can contribute to poor visual development in the affected eye, even if the lesion does not directly affect the visual axis.
Only two articles in the literature describe changes in the posterior keratoconus identified through Pentacam® analysis(10), but the Belin-Ambrósio software was not utilized in either study. Evaluation with Pentacam® adds greater accuracy to the findings already described, providing better detail and reliability in elevation and pachymetry maps. The curve in the “Corneal Thickness Spatial Profile” of the Belin-Ambrósio software for ectasia detection showed important central thinning, followed by normalization of thickness at the periphery. Likewise, with “Percentage Thickness Increase” analysis, a large increase in thickness percentage was observed at the periphery. These findings have not yet been described in the literature and may be of importance in creating a pattern for posterior ectasia diagnosis.
In conclusion, posterior keratoconus is a rare entity, and its association with high myopia and high refractive astigmatism due to the anterior irregular elevation map is fairly well described; its association with iris atrophy is also rare. We propose that alterations in mesenchymal and neural crest development, with or without a viral stimulus, may contribute to the genesis of both concomitant disorders.
REFERENCES
1. Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28(4):293-322.
2. Haney WP, Falls HF. The occurrence of congenital keratoconus posticus circumscriptus in two siblings presenting a previously unrecognized syndrome. Am J Ophthalmol. 1961;52:53-7.
3. Krachmer JH, Rodrigues MM. Posterior keratoconus. Arch Ophthalmol. 1978;96(10):1867-73.
4. Al-Hazzaa SA, Specht CS, McLean IW, Harris DJ Jr. Posterior keratoconus. Case report with scanning electron microscopy. Cornea. 1995;14(3):316-20.
5. Bonfadini G, Arora K, Vianna LM, Campos M, Friedman D, Muñoz B, Jun AS. Quantitative analysis of iris parameters in keratoconus patients using optical coherence tomography. Arq Bras Oftalmol. 2015;78(5):305-9.
6. Mannis MJ, Lightman J, Plotnik RD. Corneal topography of posterior keratoconus. Cornea. 1992;11(4):351-4.
7. Muftuoglu O, Ayar O, Ozulken K, Ozyol E, Akıncı A. Posterior corneal elevation and back difference corneal elevation in diagnosing forme fruste keratoconus in the fellow eyes of unilateral keratoconus patients. J Cataract Refract Surg. 2013;39(9):1348-57.
8. Blair SD, Seabrooks D, Shields WJ, Pillai S, Cavanagh HD. Bilateral progressive essential iris atrophy and keratoconus with coincident features of posterior polymorphous dystrophy: a case report and proposed pathogenesis. Cornea. 1992;11(3):255-61.
9. Sacchetti M, Mantelli F, Marenco M, Macchi I, Ambrosio O, Rama P. Diagnosis and management of iridocorneal endothelial syndrome. BioMed Res Int. 2015;2015:763093.
10. Abdala-Figuerola A, Navas A, Ramirez-Miranda A, Lichtinger A, Hernandez-Bogantes E, et al. Scheimpflug and optical coherence tomography analysis of posterior keratoconus. Cornea. 2016;35(10): 1368-71.
Submitted for publication:
October 10, 2017.
Accepted for publication:
June 22, 2018.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose