

Diana Silveira Silva1; Izabela Almeida2; Camila F. Netto2; Bruno L.B. Esporcatte2; Christiane Rolim-de-Moura2
DOI: 10.5935/0004-2749.20180101
ABSTRACT
Trichothiodystrophy belongs to a group of rare genetic diseases characterized by DNA repair anomalies. Ocular manifestations can occur in 50% of cases, including cataract, refractive errors, strabismus, microcornea, microphthalmia, dry eye, and pigmentary macular changes. We report a case of childhood glaucoma in a patient with trichothiodystrophy who underwent trabeculectomy in the left eye. To our knowledge, this is the first clinical report of childhood glaucoma associated with trichothiodystrophy.
Keywords: Trichothiodystrophy syndromes; Glaucoma; Xeroderma pigmentosum; DNA repair-deficiency disorders; Ocular manifestations; Humans; Case reports
RESUMO
A tricotiodistrofia pertence a um grupo de doenças genéticas raras caracterizadas por anomalias da reparação do DNA. Manifestações oculares podem ocorrer em 50% dos casos, incluindo catarata, erros refrativos, estrabismo, microcórnea, microftalmia, olho seco e alterações maculares pigmentares. Relatamos um caso de glaucoma infantil em um paciente com tricotiodistrofia submetido à trabeculectomia no olho esquerdo. No nosso conhecimento, este é o primeiro caso descrito de glaucoma infantil associado à tricotiodistrofia.
Descritores: Síndromes de tricotiodistrofia; Glaucoma; Xeroderma pigmentoso; Distúrbios no reparo do DNA; Manifestações oculares; Humanos; Relatos de casos
INTRODUCTION
Childhood glaucoma is an uncommon disorder characterized by two of the following symptoms: intraocular pressure (IOP) higher than 21 mmHg, progressive optic disc cupping, characteristic corneal findings, progressive myopia, increased ocular axial length, or reproducible visual field defects(1-5). Childhood glaucoma associated with non-acquired systemic disease corresponds to approximately 11% of childhood glaucoma cases(2).
Trichothiodystrophy (TTD) is an autosomal recessive disorder(4-7), with a reported incidence of 1.2/1,000,000 births in a Western European population(4). Although ocular manifestations have been described previously(7,8), to our knowledge, this is the first clinical report of childhood glaucoma associated with trichothiodystrophy.
CASE REPORT
A 6-year-old male child was referred for ophthalmological examination by our hospital’s dermatology section, to help with syndromic diagnosis. He presented malar erythema associated with telangiectasia (Figure 1A) from birth. His mother reported the absence of cilia and toenails at birth, and very sparse hair, which started growing 2 years later. General physical examination revealed uncharacteristic facies, slight low ear implantation with normal stature, and weight development. Hair, cilia, and nails were normal at this presentation. He presented two café-au-lait spots on his skin.
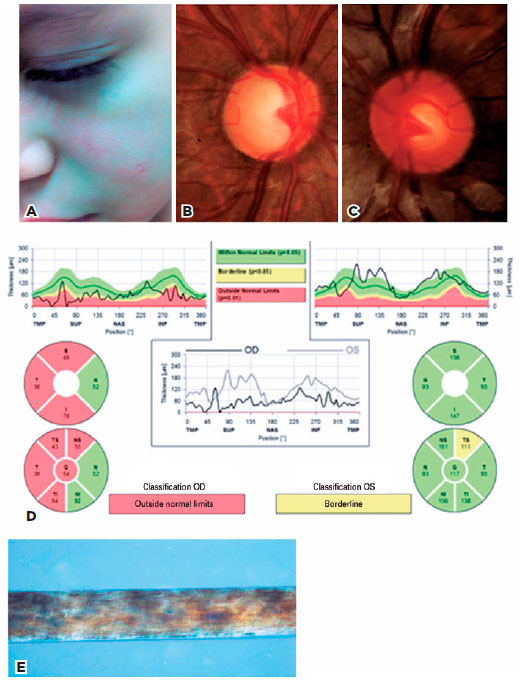
There were no ocular or visual complaints. Past and familial ocular histories were unremarkable. His mother denied systemic and ocular medication use. Routine ophthalmological evaluation presented a best-corrected visual acuity of 20/30 in his right eye (RE) and 20/20 in his left eye (LE). IOP measurements obtained with the Goldmann tonometer were elevated in both eyes (RE: 31 mmHg/LE: 44 mmHg). Biomicroscopy was unremarkable bilaterally, and corneal diameter was 12 mm in both eyes.
Upon gonioscopy of both eyes, all structures of the camerular angle were visualized up to the ciliary body band and showed normal development, without iris strands or peripheral synechiae. Fundoscopy showed a 0.9 × 0.9 cup-to-disc ratio, with nasal deviation of the retinal vessels in the RE (Figure 1B). In the LE, a pink-colored optic disc was observed, with a 0.6 × 0.6 cup-to-disc ratio and normal emergence of the retinal vessels (Figure 1C). No retinal lesions were visible in either eye.
The corneal thickness was RE: 590 µm and LE: 585 µm. Axial length was normal (RE: 23.58 mm; LE: 23.03 mm). Optical coherence tomography indicated a reduction of the peripapillary fiber layer thickness in the superior, temporal, and inferior quadrants in OD (Quality score: 23) and a borderline defect on the superior temporal sector in OS (Quality score: 18). Visual field testing was unreliable for both eyes because of a lack of cooperation (Figure 1D).
A skin biopsy on the erythematous facial lesions (Figure 1A) revealed they were chronic actinic lesions. No etiological diagnosis was determined at this point.
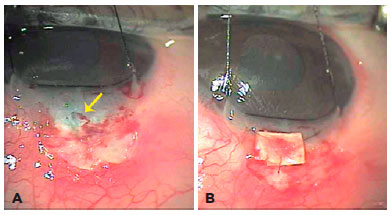
The patient was initially medicated with topical timolol maleate and dorzolamide in both eyes. Latanoprost was further added, but IOP remained at 24 mmHg RE and 18 mmHg LE. Because of advanced glaucomatous damage in RE, a mitomycin-augmented trabeculectomy was indicated. There were no surgical complications, and the first postoperative days were uneventful. He developed seidel on the 18th postoperative day associated with conjunctival wound dehiscence. Suture revision was performed the next week; however, wound dehiscence and conjunctival thinning was observed again 3 weeks later. On second observation under general anesthesia, we found melting of the scleral flap; thus, a scleral patch and conjunctival advancement was necessary (Figure 2A and B). No further complications were observed. The hypotony was controlled successfully and IOP stabilized at 15 mmHg RE.
Concurrent dermatological investigation led to examination of the hair under light microscopy, which revealed characteristic tiger tail banding highly suggestive of trichothiodystrophy (Figure 1E). A diagnosis of secondary glaucoma associated with trichothiodystrophy was thus established.
Two years after surgery, IOP is 15 mmHg RE without drugs and 16 mmHg LE, with latanoprost, timolol maleate, and dorzolamide. Visual acuity and optic disc cupping remain stable in both eyes.
DISCUSSION
Incidental findings of elevated IOP, raised cup-to-disc ratio for the optic nerve in both eyes, and characteristic defects in the nerve fiber layer optical coherence tomography, along with normal gonioscopy, axial length, corneal diameter, and anterior segment examination led us to the potential diagnoses of primary juvenile glaucoma, secondary glaucoma associated with systemic diseases, and corticosteroid-induced glaucoma. The latter was excluded on the basis of the absence of corticosteroid use.
The hallmark of trichothiodystrophy is congenital hair dysplasia characterized by hair deficient in sulfur and cystine content, as well as an alternating light banding pattern (tiger tail banding) when visualized microscopically, associated with multisystemic abnormalities(8). The spectrum of clinical manifestations is broad, with some patients presenting only mild hair and nail changes, but commonly consists of photosensitivity, ichtyosis, brittle hair, intellectual impairment, short stature, and predisposition to infectious diseases(8).
The diagnosis is established on the basis of observation of the characteristic microscopic changes of the hair. Genetic changes typically include mutations in DNA repair genes xeroderma pigmentosum type B, xeroderma pigmentosum D, or trichothiodystrophy group A (TTDA) (also involved in xeroderma pigmentosum pathogenesis), as well as in TTDN1, a gene of unknown function(6-8). Our patient’s presentation with malar rash associated with telangiectasia present from birth, photosensitivity, and a history of nail and hair changes led to the consideration of genetic photodermatoses, namely, Bloom syndrome, which was excluded after normal comparative genomic hybridization testing. Further investigation revealed, through hair microscopy analysis, a characteristic tiger tail banding pattern, which is highly suggestive of trichothiodystrophy. The absence of mental impairment, short stature, and repeated infections led us to believe that this could be a milder case of trichothiodystrophy(9).
Regarding postoperative scleral flap melting, we believe that although mitomycin is indicated frequently in pediatric trabeculectomy surgeries, this complication possibly arose because of a synergistic effect between the antimetabolite action of mitomycin and a trichothiodystrophy-related DNA repair anomaly, unknown when surgery was indicated. Although no records of scleral flap melting associated with systemic diseases are reported in the literature, in our opinion, prior knowledge of the diagnosis would have contraindicated mitomycin use(10).
To the best of our knowledge, this the first case of childhood glaucoma associated with trichothiodystrophy. We conducted a search in the MEDLINE/PUBMED, EBSCO, EMBASE, Ophthalmic Literature, and Zentralblatt für die gesamte Ophthalmologie und ihre Grenzgebiete databases, which produced zero results.
Thorough investigation is important to establish the diagnosis of this disorder, and, when glaucoma surgery is indicated, we believe that mitomycin use should be carefully evaluated.
ACKNOWLEDGMENTS
The authors thank the Dermatology Department of the Federal University of São Paulo and Dr. Ken K. Nischal, for helping in diagnosis elucidation.
REFERENCES
1. Weinreb RN, Grajewski A, Papadopoulos M, Grigg J, Freedman S. Childhood Glaucoma. Amsterdam: Kugler; 2013. (WGA Consensus Series - 9).
2. Hoguet A, Grajewski A, Hodapp E, Chang TC. A retrospective survey of childhood glaucoma prevalence according to Childhood Glaucoma Research Network classification. Ind J Ophthalmol. 2016;64(2):118-23.
3. Kwun Y, Lee EJ, Han JC, Kee C. Clinical characteristics of juvenile-onset open angle glaucoma. Korean J Ophthalmol. 2016;30(2):127-33.
4. Aponte EP, Diehl N, Mohney BG. Incidence and clinical characteristics of childhood glaucoma: a population-based study. Arch Ophthalmol. 2010;128(4):478-82.
5. Gupta V, Somarajan BI, Gupta S, Chaurasia AK, Kumar S, Dutta P, et al. The inheritance of juvenile onset primary open angle glaucoma. Clin Genet. 2017;92(2):134-42.
6. Kraemer KH, Patronas NJ, Schiffmann R, Brooks BP, Tamura D, DiGiovanna JJ. Xeroderma pigmentosum, trichothiodystrophy and Cockayne syndrome: A complex genotype-phenotype relationship. Neuroscience. 2007;145(4):1388-96.
7. Kleijer WJ, Laugel V, Berneburg M, Nardo T, Fawcet H, Gratchev A, Jaspers NG, et al. Incidence of DNA repair deficiency disorders in western Europe: Xeroderma pigmentosum, Cockayne syndrome and trichothiodystrophy. DNA Repair. 2008;7(5):744-50
8. Faghri S, Tamura D, Kraemer KH, DiGiovanna JJ. Trichothiodystrophy: a systematic review of 112 published cases characterises a wide spectrum of clinical manifestations. J Med Genet. 2008;45(10):609-21.
9. Lambert WC, Gagna CE, Lambert MW. Trichothiodystrophy: photosensitive, TTD-P, TTD, Tay syndrome. Adv Exp Med Biol. 2010; 685:106-10.
10. Brooks BP, Thompson AH, Clayton JA, Chan CC, Tamura D, Zein WM, et al. Ocular manifestations of trichothiodystrophy. Ophthalmology. 2011;118(12):2335-42.
Submitted for publication:
March 7, 2018.
Accepted for publication:
May 27, 2018.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose