

Rubens N. Belfort1; Monica Santos Müller1; Jordan Isenberg2; Patricia Ferraz1; Denis Szejnfeld3
DOI: 10.5935/0004-2749.20180099
ABSTRACT
Uveal melanoma is the most common adult primary intraocular cancer. Although liver metastasis is common to the natural history of the disease, metastasis to the fellow eye is extremely rare. Here we report the case of a 59-year-old man with choroidal melanoma in his right eye who underwent enucleation at a different center. The patient was referred to our service 21 months postoperatively, complaining of decreased vision. He was found to have a new pigmented choroidal tumor in his left eye associated with liver disease. Ocular ultrasonography and liver biopsy with histopathological and immunohistochemical analysis were performed and confirmed the diagnosis. Few similar cases have been described in the literature. The differential diagnosis included primary bilateral choroidal melanoma and metastatic choroidal tumor from a primary skin melanoma.
Keywords: Choroid neoplasms/secondary; Melanoma; Neoplasms metastasis; Diagnosis, differential
RESUMO
O melanoma uveal é o câncer intraocular primário mais frequente em adultos. Embora a metástase hepática seja comum à história natural da doença, a metástase para o outro olho é extremamente rara. Aqui relatamos o caso de um homem de 59 anos com melanoma de coroide em seu olho direito que foi submetido à enucleação em um centro diferente. O paciente foi encaminhado ao nosso serviço 21 meses após a cirurgia, com queixa de diminuição da visão. Foi encontrado um novo tumor de coróide pigmentado em seu olho esquerdo associado com doença hepática. Ultrassonografia ocular e biópsia hepática com exame histopatológico e imuno-histoquímico foram realizadas e confirmaram o diagnóstico. Poucos casos semelhantes foram descritos na literatura. O diagnóstico diferencial incluiu melanoma de coróide bilateral orimário e tumor coroidal metastático de um melanoma primário da pele.
Descritores: Neoplasias da coroide/secundário; Melanoma; Metástase neoplásica; Diagnóstico diferencial
INTRODUCTION
Choroidal melanoma is the most common primary intraocular malignancy in adults and the second most common site for melanoma, after the skin. The tumor is usually identified after causing visual symptoms but can also be found with a routine fundus exam. It can be treated by enucleation or plaque brachytherapy depending on the size and location. These techniques are extremely effective for local tumor control; however, patients present risk of developing metastatic disease. Liver is the most common metastatic site. We present a patient treated for choroidal melanoma with enucleation that presented melanoma in the other eye after 21 months.
CASE REPORT
A 59-year-old Caucasian man with no significant past medical history or prior history of ocular disease presented in March 2012 for a routine ophthalmic examination. At that time, an elevated pigmented choroidal mass in his right eye was noted, while his left eye was unremarkable. Diagnosis of presumed choroidal melanoma was made, and the right globe was enucleated immediately thereafter. Pathological examination confirmed an epithelioid melanoma that was 17 mm in its largest diameter.
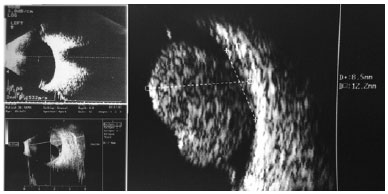
At his 17-month post-operative follow-up, the patient presented to his treating physician complaining of progressive left eye vision loss and retrobulbar pain over the past six months. Left eye ultrasonography was performed at that time. The results were normal. After three months, a second ultrasound revealed a mushroom-shaped choroidal mass with low internal reflectivity and thickness of 7.4 mm. Serous retinal detachment was noted.
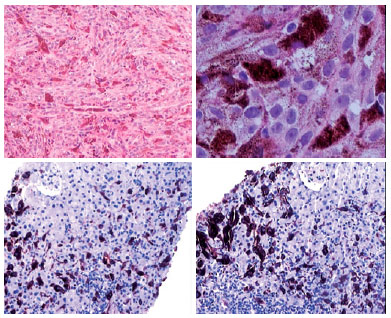
The patient was referred to our ocular oncology service and was examined 21 months postoperatively. The patient’s complaints persisted. On exam, he had visual acuity of 20/60 (6/18). The anterior segment was remarkable for an abnormal red reflex (Figure 1). Dilated fundus examination revealed a superior pigmented choroidal lesion, associated with a retinal detachment that extended inferior to the fovea. On ocular ultrasonography, the lesion had the same characteristics as noted previously but had increased in thickness to 12.2 mm (Figure 2). Abdominal ultrasonography revealed multiple hepatic lesions that were sampled by ultrasound-guided biopsy. A characteristic dark lesion was observed (Figure 3). Histopathological examination and immunohistochemical analysis were performed. The latter was positive for MELAN A, HMB45, and S100. These findings confirmed the diagnosis of hepatic uveal melanoma metastasis with mixed cell type (Figure 4).


Plaque brachytherapy of the left eye was indicated as palliative treatment, and chemoembolization of liver metastases was performed. Nevertheless, the disease progressed, and the patient died 6 months after our initial visit at post-operative month 27.
DISCUSSION
Choroidal melanoma metastasis to the fellow eye is an extremely rare and aggressive phenomenon, with fewer than 10 published case reports(1-6). There are three distinct theories that may shed light on the pathobiology of bilateral choroidal melanoma: the contralateral choroidal tumor may be a metastatic tumor from the primary choroidal melanoma in the first eye; both tumors may be metastatic in origin from a primary cutaneous or visceral melanoma; both choroidal melanomas may be primary tumors(5,7,8).
Unfortunately, there is no curative treatment for metastatic melanoma. Like other related cases, the patient’s disease progressed, resulting in his death after six months. From the clinical history and the histopathologic results, we presumed that the lesion in the left eye was a metastatic tumor from the contralateral eye.
The median time to systemic metastases of uveal melanoma is 3.25 years(8). In our case, the mass in the fellow eye was diagnosed 20 months postoperatively. When looking specifically at choroidal metastasis, our results compare to the low end, as other studies have variable manifestations: with 12 months at the low end(5), 72 months mid-range(4), and 15 years considered long term(2).
The patient presented here was not found not to have cutaneous melanoma. Should the initial choroidal lesion in fact be the metastatic manifestation of a cutaneous melanoma, then, given the natural history, we would expect a more rapid disease progression, as 1- and 2-year survival are 32% and 18%, respectively(9). This was not the case, since the patient was disease free for almost 2 years, making a primary ocular tumor more probable.
REFERENCES
1. Li J, Resnick K, Tso M. Metastasis of malignant melanoma of the choroid and ciliary body to the contralateral choroid. Graefes Arch Clin Exp Ophthalmol. 1993;231(9):546-53.
2. Singh AD, Shields JA, Shields CL, Sato T. Choroidal melanoma metastatic to the contralateral choroid. Am J Ophthalmol. 2001; 132(6):941-3.
3. Diener-West M, Reynolds SM, Agugliaro DJ, Caldwell R, Cumming K, Earle JD, et al. Development of metastatic disease after enrollment in the COMS trials for treatment of choroidal melanoma: Collaborative Ocular Melanoma Study Group Report No. 26. Arch Ophthalmol. 2005;123(12):1639-43.
4. Khetan V, Ambatipudi S, Gopal L. Presumed metastasis of choroidal melanoma to the contralateral choroid. Retin Cases Brief Rep. 2010;4(4):387-9.
5. Caminal Mitjana JM, Vila Grane N, Adan Civera A, Sabater N, Arias Barquet L, Rubio Caso MJ. Clinical Course of a presumed metastatic uveal melanoma to the contralateral choroid. Semin Ophthalmol. 2015;30(5-6):417-9.
6. Torossian NM, Wallace RT, Hwu WJ, Bedikian AY. Metastasis of ciliary body melanoma to the contralateral eye: a case report and review of uveal melanoma literature. Case Rep Oncol Med. 2015; 2015:427163.
7. Singh AD, Shields CL, Shields JA, De Potter P. Bilateral primary uveal melanoma. Bad luck or bad genes? Ophthalmology. 1996; 103(2):256-62.
8. Shields CL, Shields JA. Choroidal and retinal metastasis. In: Arévalo JF, editor. Retinal and choroidal manifestations of selected systemic diseases. New York, NY: Springer New York; 2013. p. 267-82.
9. Dickson PV, Gershenwald JE. Staging and prognosis of cutaneous melanoma. Surg Oncol Clin N Am. 2011;20(1):1-17.
Submitted for publication:
January 22, 2018.
Accepted for publication:
June 3, 2018.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose