

Kursat Atalay; Senay Asik Nacaroglu; Ahmet Kirgiz
DOI: 10.5935/0004-2749.20180098
ABSTRACT
Although minimally invasive glaucoma surgery using different types of implants is a promising strategy for treating glaucoma, potential long-term complications require further evaluation. Here, we report a case of the anterior chamber displacement of a Xen implant due to a maneuver aimed at correcting a dysfunctional and bent subconjunctival implant.
Keywords: Glaucoma; Filtering surgery; Minimally invasive surgical procedures/methods; Anterior chamber
RESUMO
Embora a cirurgia de glaucoma minimamente invasiva, que usa diferentes tipos de implantes, seja uma estratégia promissora para o tratamento do glaucoma, as possíveis complicações a longo prazo exigem uma avaliação mais aprofundada. Aqui, relatamos um caso de deslocamento da câmara anterior de um implante Xen devido a uma manobra que visa corrigir um implante subconjuntival disfuncional e dobrado.
Descritores: Glaucoma; Cirurgia filtrante; Procedimentos cirúrgicos minimamente invasivos/métodos; Câmara anterior
INTRODUCTION
Minimally invasive surgery using micro-bypass implants is a promising strategy for treating glaucoma(1). An implant, the Xen gel stent (XGS) (XEN® gel stent, Allergan), is thought to work per the criteria of the Hagen-Poiseuille equation for the treatment of primary open-angle glaucoma (POAG)(2). XGS has a 45-µm lumen size, and it is 6 mm long from one end to the other. Several reports have confirmed that XGS provides favorable outcomes in terms of intraocular pressure (IOP) control, and only a few recent reports have indicated complications(3). Here, we report a case of the anterior chamber (AC) displacement of an XGS and its removal during a maneuver for correction of a dysfunctional and bent implant.
CASE REPORT
A 68-year-old male patient diagnosed with POAG showed glaucoma progression despite three anti-glaucoma eye-drop treatments and one session of selective laser trabeculoplasty (SLT) in his left eye. Visual acuity measurements done using the Snellen chart were 0.8 in the right eye and 0.3 in the left eye. His IOP readings were 21 mmHg in the right eye and 30 mmHg in the left eye. Pseudophakia and an epiretinal membrane formation were present in the left eye. Average results of nerve fiber layer analyses of the optic discs were 99 in the right eye and 55 in the left eye. The mean deviation in the visual field examination was -9.82 in the right eye and -18.59 in the left eye.
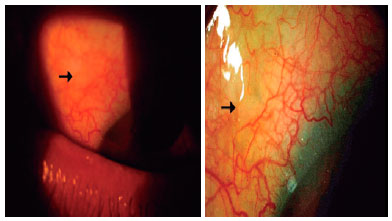
The patient underwent a routine surgery with 0.2 mg/ml mitomycin C administered sub-conjunctivally, as described previously(4). The tip of XGS was observed via gonioscopy at the end of the surgery. The patient visited six months after an uncomplicated early follow-up period, and we found an increased IOP (35 mmHg) with a blebless and bent XGS (Figure 1). We thought that the dysfunction of the implant was due to the bending; therefore, we planned a maneuver to straighten XGS. We placed a lid speculum while the patient was under topical anesthesia in the polyclinic room. We used a sterile blunt spatula to support the bending side of the Xen over the conjunctiva and then applied a sterile cotton swab to push the free end of the stent gently to properly align it. The resistance of tissue felt during application of the cotton swab suddenly decreased. A subconjunctival bleb formed with backward movement of XGS into the AC (Figure 2). The IOP was measured to be 10 mmHg after this maneuver. However, one month after this procedure, the IOP rose to 35 mmHg and the cornea was edematous. Because of the proximity of XGS to the cornea, and the willingness of the patient to have it removed, we removed XGS. The IOP decreased to 20 mmHg with two glaucoma eye drops, and the corneal edema was resolved.
DISCUSSION
Manipulations of an XGS may unintentionally shift its position. Some mechanisms have been proposed to explain the relative fixation of an XGS at the implantation site; for example, Dervenis et al., suggested that the implant position is not fixed and secured, and therefore migration to the AC can occur(3). These authors argued for a potential role of episcleritis and external forces applied by the patient to XGS as reasons for the movement of the implant. Episcleritis is an inflammatory disease that affects the anterior segment of the eye. Our patient did not mention any ocular trauma or eye rubbing during the follow-up period. We also did not detect any previous episcleritis diagnosis from the patient’s history. However, the patient had a history of SLT treatment. The SLT involves aiming NdYag laser spots onto the AC angle and usually causes a transient and slight, but detectable, inflammatory reaction in the AC of the eye(5,6). Matrix metalloproteinases, which are important enzymes in extracellular collagen breakdown, increase in activity during inflammation(7). The implantation of biomaterials is also known to induce local reactions that affect the extracellular matrix and the implant itself(8). If Dervenis et al. are correct regarding the causative role of episcleritis and inflammation in the mobility of XGS, the only potential source of inflammation in the AC of our patient was his history of SLT treatment(3).
In our case, the malfunctioning XGS could have been managed in a different way; for example, we could have attempted to needle around the tip of XGS rather than pushing or manipulating the implant itself. In addition, in our case, XGS was not completely displaced into the AC. However, a total movement of XGS into the AC may have inevitably complicated a preexisting condition. Therefore, an operating room may be a more appropriate site for such maneuvers, to avoid subjecting the patient to additional surgical stress.
In the present case, XGS was shown to have the potential to move from the implantation site. Manipulations over Xen material should be done cautiously, preferably in an operating room.
REFERENCES
1. Kerr NM, Wang J, Barton K. Minimally invasive glaucoma surgery as primary stand-alone surgery for glaucoma. Clin Exp Ophthalmol. 2017;45(4):393-400. doi: 10.1111/ceo.12888.
2. Sheybani A, Reitsamer H, Ahmed II K. Fluid dynamics of a novel micro-fistula implant for the surgical treatment of glaucoma. Invest Ophthalmol Vis Sci. 2015;56(8):4789-95. doi: 10.1167/iovs.15-16625. Comment in: Invest Ophthalmol Vis Sci. 2015;56(13):8026.
3. Dervenis N, Mikropoulou AM, Dervenis P, Lewis A. Dislocation of a previously successful XEN glaucoma implant into the anterior chamber: a case report. BMC Ophthalmol. 2017;17(1):148. doi: 10.1186/s12886-017-0540-1.
4. Galal A, Bilgic A, Eltanamly R, Osman A. XEN glaucoma implant with mitomycin C 1-year follow-up: results and complications. J Ophthalmol. 2017;2017:5457246. doi: 10.1155/2017/5457246.
5. Kramer TR, Noecker RJ. Comparison of the morphologic changes after selective laser trabeculoplasty and argon laser trabeculoplasty in human eye bank eyes. Ophthalmology. 2001;108(4):773-9.
6. De Keyser M, De Belder M, De Groot V. Randomized prospective study of the use of anti-inflammatory drops after selective laser trabeculoplasty. J Glaucoma. 2017;26(2):e22-9.
7. Bradley JM, Anderssohn AM, Colvis CM, Parshley DE, Zhu XH, Ruddat MS, et al. Mediation of laser trabeculoplasty-induced matrix metalloproteinase expression by IL-1beta and TNFalpha. Invest Ophthalmol Vis Sci. 2000;41(2):422-30.
8. Franz S, Rammelt S, Scharnweber D, Simon JC. Immune responses to implants – A review of the implications for the design of immunomodulatory biomaterials. Biomaterials. 2011;32(28):6692-709. doi: 10.1016/j.biomaterials.2011.05.078
Submitted for publication:
February 6, 2018.
Accepted for publication:
June 10, 2018.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose