

Luísa Nardino Gazzola1; Mariela Regina Dalmarco Ghem1; Crislaine Serpe1; Marcony Rodrigues Santhiago2; Glauco Reggiani Mello1
DOI: 10.5935/0004-2749.20180083
ABSTRACT
A patient with bilateral aniridia and progressive congenital cataract was treated at the age of 7 years through phacoaspiration with femtosecond laser capsulotomy, in-the-bag intraocular lens implantation, and pars plana vitrectomy (combined with posterior capsulotomy). The diameter of the planned anterior capsulotomy was 4.7 mm; however, due to elevated tension in the young capsular bag, the capsulotomy diameter increased (to around 6 mm) shortly after release of the tension by the laser. In addition, the patient had a very flat and small cornea, causing the formation of air bubbles in the curved laser interface. This was addressed by filling the gap by using a viscoelastic. A very similar situation was observed in both eyes. Use of the femtosecond laser facilitated a successful outcome in a complex congenital cataract case with a safe capsulotomy that ensured in-the-bag intraocular lens placement.
Keywords: Aniridia; Cataract/congenital; Capsulorhexis; Phacoemulsification; Lens implantation, intraocular; Laser therapy; Case reports
RESUMO
Paciente com aniridia bilateral e catarata congênita progressiva foi tratado com a idade de 7 anos através de facoemulsificação com capsulotomia anterior por laser de femtosegundo, implante de lente intra-ocular e vitrectomia via pars plana (combinada com capsulotomia posterior). O diâmetro da capsulotomia anterior prevista foi de 4,7mm, porém, devido à elevada tensão do saco capsular jovem, o diâmetro da capsulotomia aumentou (para cerca de 6mm) logo após a liberação da tensão pelo laser. Além disso, o paciente tinha uma córnea muito plana e pequena, causando a formação de bolhas de ar na interface do laser. Isso foi resolvido preenchendo a lacuna usando um viscoelástico. Uma situação muito semelhante foi observada em ambos os olhos. O uso do laser de femtosegundo facilitou um resultado bem-sucedido em um caso complexo de catarata congênita com uma capsulotomia anterior segura que garantiu a colocação da lente intra-ocular dentro do saco capsular.
Descritores: Aniridia; Catarata/congênito; Capsulorrexe; Facoemulsificação; Implante de lente intraocular; Terapia a laser; Relatos de casos
INTRODUCTION
Aniridia, a rare eye disease characterized by the total or partial absence of the iris, is attributed to different degrees of hypoplasia and malformation. Microcornea, corneal clouding, glaucoma, lens subluxation, hypoplasia of the optic nerve and fovea, and cataract are among the co-ocular manifestations of aniridia(1). The disease can also be accompanied by a primary limbal stem-cell deficiency due to an insufficient stromal microenvironment to support stem cell function(2).
The currently accepted surgical technique to treat congenital cataracts after the first year of life is manual phacoemulsification and intraocular lens (IOL) implantation, at times followed by pars plana vitrectomy(3). Capsulotomy is a crucial surgical step and is considerably more difficult when manually performed in children due to increased capsular elasticity and a tendency for anterior and posterior tears(4). In aniridia, the importance of a perfectly executed capsulotomy is even greater, because without the iris, the surgeon faces fewer options for proper positioning of the IOL.
In this particular case, there was an association of a progressive bilateral congenital cataract in a pediatric patient with congenital aniridia.
CASE REPORT
A 7-year-old boy diagnosed as having bilateral aniridia and mild congenital cataract at 3 months of age presented with visual impairment and increased lens opacity in both eyes. He was a term baby with a birth weight of 2730 g, with no major alterations reported during pregnancy or delivery. The patient denied having any comorbidities.
On ophthalmic examination, significant bilateral posterior subcapsular lens opacity and aniridia were noted. Optic disc stereo photography was unremarkable. The best corrected visual acuity (BCVA) was 1 logMar (Snellen equivalent 20/200) in the right eye, 0.845 logMar (Snellen equivalent 20/140) in the left eye, with SE +7.00D OU. Perkins tonometry in the office was normal at 14 mmHg OD and 15 mmHg OS and did not require the patient to be sedated.
Corneal tomography (Galilei G2, Ziemer, Port-Switzerland) showed a regular flat cornea in both eyes. Simulated keratometry showed 40.14 D at 52 degrees and 41.03 D at 142 degrees in the right eye and 40.13 D at 66 degrees and 40.95 D at 150 degrees in the left eye. The thinnest pachymetry score was 695 micra in the right eye and 690 micra in the left eye. Axial length measured by immersion ultrasound biometry was 21.10 mm in the right eye and 21.12 mm in left eye. Anterior chamber depth was 3.33 mm in the right eye and 3.21 mm in the left eye.
The family approved the plan of phacoaspiration assisted by femtosecond laser and hydrophobic acrylic IOL implantation followed by pars plana vitrectomy (combined with posterior capsulotomy) in both eyes, starting with the right eye. They were previously informed about the poor visual prognosis due to other congenital abnormalities and probable amblyopia.
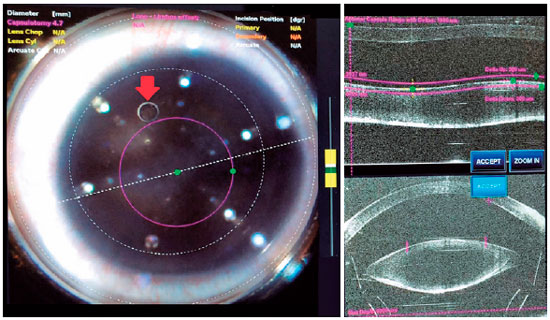
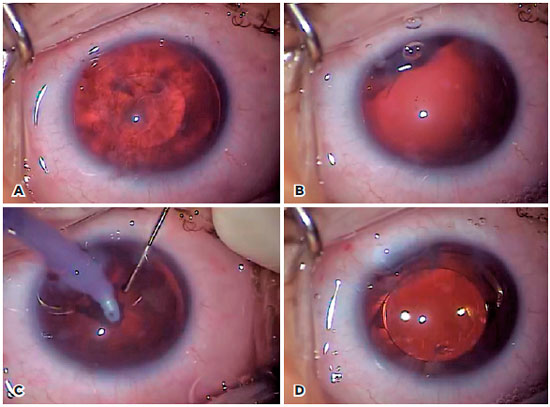
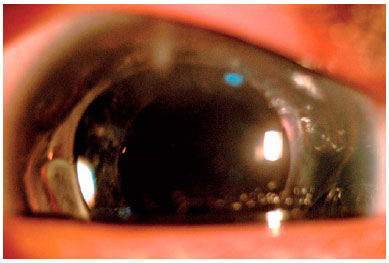
The surgery was completely performed under general anesthesia (including femtosecond laser docking). An assistant helped to keep the patient’s head in an adequate position during docking and capsulotomy. The capsulotomy was the only surgical step performed using the Femtosecond laser (Alcon-LenSx Lasers Inc., Fort Worth, TX, USA) (Figure 1), with manual corneal incisions and an automated nuclear phacoaspiration (Infinity Alcon, Fort Worth, TX, USA). The surgical plan did not include femtosecond laser fracture and incisions because we expected a very soft nucleus that could be easily aspirated without the need for ultrasound energy. The patient also had mild corneal neovascularization (that could impair the laser corneal incisions) probably due to a mild limbal stem cell deficiency, which is expected with aniridia syndrome. Docking was difficult for both eyes due to the formation of an air bubble in the interface, presumed to be related to the very flat and small cornea. After 3 unsuccessful docking attempts, the surgeon decided to use a 2% methylcellulose viscoelastic to fill the gap and avoid bubble formation in the interface. The diameter of the planned capsulotomy was 4.7 mm (Figure 2A). There were no tags or tears in the anterior capsule. Nevertheless, during the phacoaspiration procedure, we observed that the capsulotomy was larger than planned (Figure 2B), probably due to a greater release of tension in the elastic capsule related to pediatric lens peculiarities. Phacoaspiration was performed using only a coaxial irrigation/aspiration system without any difficulty (Figure 2C). A +31.00D IOL (AcrySof SA60AT; Alcon Laboratories, Fort Worth, TX, USA) was implanted in the bag (Figure 2D). Pars plana vitrectomy was then performed, including a posterior capsular bag opening. There were no postoperative complications. The same procedure was performed on the patient’s left eye. One and a half years after the surgeries, the subjective refraction was +1,50 -1,00 110° OD with a plano value of -2,25 95° OS and the BCVA was 0.4 logMar (Snellen equivalent 20/50) OU (Figure 3).
DISCUSSION
Several surgical techniques, such as pars plana vitrectomy, traditional phacoemulsification, and surgery assisted by a femtosecond laser, can be used to treat congenital cataract. In case of a severe decrease in BCVA, most surgeons consider performing an early cataract surgery within the first year of life with or without IOL implantation(5). Interference in the development and behavior of the child are other alterations that should be investigated in the indication of surgery for cataract correction. In the present case, the patient had been diagnosed as having mild cataract at 3 months of age. Nevertheless, the progressive nature of his cataract justified posterior intervention at 7 years of age. Until then, the patient’s visual acuity and development were compatible with his age and aniridia. Cataract surgery in children has many potential complications such as increased postoperative inflammation, axial growth after cataract extraction, less accurate calculation of the IOL, secondary glaucoma, posterior-capsule opacification, and amblyopia management(4,5). Additionally, the properties of the pediatric lens and capsule contribute to an increased risk of anterior tears during capsulotomy, making this crucial step considerably more difficult in pediatric patients than in adult patients(4). Manual continuous curvilinear capsulorrhexis (CCC) is a popular anterior capsulotomy technique for treating adult cataract because it is relatively easy to perform and yields a low rate of radial tears(4). However, the anterior lens capsule in children is very elastic and requires the application of more force before tearing begins.
Although the Femtosecond laser provides a more precise capsulotomy and IOL positioning, it demonstrates no relevant clinical gain and increased complications, such as suction break during capsulotomy creation, conjunctival redness or hemorrhage, capsule tags and bridges, anterior capsule tears, endothelial damage, and intraoperative pupil miosis(6-8).
This presenting patient required a perfectly executed capsulotomy, because there was no anterior support from the iris as in regular cataract surgeries. Therefore, the surgeon was unable to place the IOL into the ciliary sulcus. In addition, the absence of the iris compromises iris fixated IOL technique. A scleral fixated IOL is not the first option in children due to increased postoperative complications. Furthermore, there is little experience with transscleral fixated IOLs in pediatric patients(9). The prior perfectly executed capsulotomy helped us ensure proper IOL positioning in our patient.
Implantation of an aniridia-correcting IOL was not performed for three main reasons: the IOL that we considered the best for this type of correction (Morcher, Stuttgart, Germany) is not commercialized in Brazil. This type of IOL usually has a larger diameter, requiring a larger incision, which could introduce more risks than benefits in cases of congenital aniridia. We believe that its use has a greater indication in cases of traumatic aniridia. Greater fibrosis of the remaining peripheral posterior capsule, which occurs after phacoemulsification in pediatric patients, generates an important peripheral posterior capsule opacity, which can help reduce postoperative photophobia.
Because of the elevated tension inside the pediatric capsular bag and its elastic properties, there was an immediate increase in the capsulotomy diameter shortly after the laser procedure. Despite the 4.7mm planned diameter, it was measured as 6 mm by comparison to the IOL optic. These data show the importance of a smaller capsulotomy plan in children when compared to adults.
Another challenge encountered during this procedure was the patient’s very flat and small cornea, leading to the formation of air bubbles in the curved laser interface requiring the use of a viscoelastic to fill the gap.
The use of the femtosecond laser can contribute to a successful outcome in specific complex cases. This case report warrants larger studies on the use of femtosecond lasers in congenital cataract surgery and aniridia, associated or not, in order to provide further information about femtosecond laser-assisted phacoemulsification complications and their management.
REFERENCES
1. Biswas J, Chakrabarti A, Das D. Rare association of familial aniridia, microcornea with myopia and aphakia. Middle East Afr J Ophthalmol. 2014;21(3):268-70.
2. Dua HS, Saini JS, Azuara-Blanco A, Gupta P. Limbal stem cell deficiency: concept, aetiology, clinical presentation, diagnosis and management. Indian J Ophthalmol. 2000;48(2):83-92.
3. Wilson ME, Pandey SK, Thakur J. Paediatric cataract blindness in the developing world: surgical techniques and intraocular lenses in the new millennium. Br J Ophthalmol. 2003;87(1):14-9.
4. Wilson ME. Anterior lens capsule management in pediatric cataract surgery. Trans Am Ophthalmol Soc. 2004;102:391-422.
5. Medsinge A, Nischal KK. Pediatric cataract: challenges and future directions. Clin Ophthalmol. 2015;9:77-90.
6. Kránitz K, Takacs A, Miháltz K, Kovács I, Knorz MC, Nagy ZZ. Femtosecond laser capsulotomy and manual continuous curvilinear capsulorrhexis parameters and their effects on intraocular lens centration. J Refract Surg. 2011;27(8):558-63.
7. Moshirfar M, Churgin D, Hsu M. Femtosecond laser-assisted cataract surgery: A current review. Middle East Afr J Ophthalmol. 2011; 18(4):285-91.
8. Nagy ZZ, Takacs AI, Filkorn T, Kránitz K, Gyenes A, Juhász É, et al. Complications of femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2014;40(1):20-8.
9. Ahmadieh H, Javadi MA. Intra-ocular lens implantation in children. Curr Opin Ophthalmol. 2001;12:(1)30-4.
Submitted for publication:
August 2, 2017.
Accepted for publication:
April 18, 2018.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose