

Sergio E. Hernandez-Da Mota1,2; Gerardo Garcia-Aguirre3,4; Raul Velez-Montoya3
DOI: 10.5935/0004-2749.20180082
ABSTRACT
We report the trans-operative approach and short-term outcome for a patient who suffered a traumatic avulsion of the cilioretinal artery branch during the surgical management of a cilioretinal arterial branch occlusion with intraocular embolectomy. The patient underwent a pars plana vitrectomy with in situ embolectomy. The blocked artery was incised using 25 Ga vertical scissors, and embolus manipulation was performed using microsurgical forceps. During embolus extraction, the occluded cilioretinal artery and its branch were inadvertently avulsed and torn with subsequent intense bleeding. Laser and endodiathermy were used for acute hemostasis. The maneuvers created an unintended retinochoroidal anastomosis. Visual-field improvement was noted three months after the surgery. In the event of a complicated surgical embolectomy with the avulsion of the artery, the formation of a retinochoroidal anastomosis and reperfusion of the occluded artery may occur along with the improvement of the visual field in some cases.
Keywords: Retinal artery occlusion; Ciliary arteries; Embolectomy; Vitrectomy; Postoperative complications; Case reports
RESUMO
Relatamos a abordagem transoperatória e o desfecho em curto prazo de um paciente que sofreu uma avulsão traumática do ramo da artéria ciliorretiniana durante o tratamento cirúrgico de uma oclusão do ramo arterial ciliorretiniano com embolectomia intraocular. O paciente foi submetido a uma vitrectomia pars plana com embolectomia in situ. A artéria bloqueada foi incisada com uma tesoura vertical de 25 Ga e a manipulação do êmbolo foi feita com pinça microcirúrgica. Durante a extração do êmbolo, a artéria ciliorretiniana ocluída e seu ramo foram inadvertidamente avulsionados e rasgados com sangramento intenso subsequente. Laser e endodiatermia foram utilizados para hemostasia aguda. As manobras criaram uma anastomose retinocoroidiana não intencional. Melhora do campo visual foi observada três meses após a cirurgia. No caso de uma embolectomia cirúrgica complicada com a avulsão da artéria, a formação de uma anastomose retinocoroidiana e reperfusão da artéria ocluída pode ocorrer juntamente com a melhora do campo visual em alguns casos.
Descritores: Oclusão da artéria retiniana; Artérias ciliares; Embolectomia; Vitrectomia; Complicações pós-operatórias; Relatos de casos
INTRODUCTION
Cilioretinal arterial branch occlusion (CRABO) is an uncommon clinical entity that accounts for less than 10% of all arterial occlusions(1).
Surgical embolectomy is proposed as a feasible alternative to medical therapy for CRABO because of the lack of adequate medical treatment(2-5). The purpose of this case report is to describe the trans-operative management and short-term outcome of a complicated case of surgical embolectomy in a patient with acute cilioretinal artery occlusion.
CASE REPORT
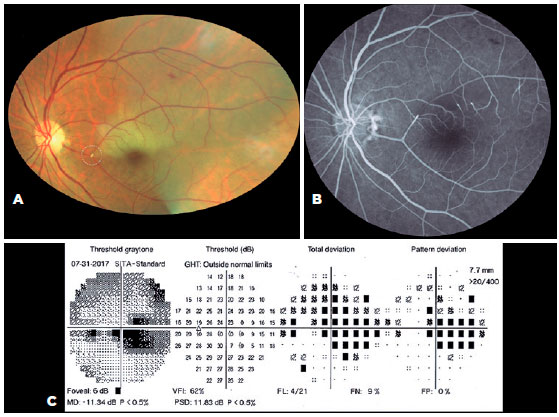
A 65-year-old male patient visited the outpatient clinic referencing significant visual loss in his left eye over the last 7 days. The best corrected visual acuity (BCVA) was 20/20 in his right eye and 5/400 in his left eye. Fundus examination revealed a Hollenhorst plaque obstructing the arterial flow of a branch of the cilioretinal artery, compromising the perfusion of the superior foveal region. Preoperative fluorescein angiography findings, as well as a central and temporal scotoma involving fixation in the 30-2 visual fields, are shown in figure 1.
After discussing several therapeutic alternatives, the patient opted for a surgical embolectomy. A three-port 23 Ga pars plana vitrectomy was performed with separation of the posterior hyaloid. Brilliant blue G was then injected to stain the internal limiting membrane (ILM), which was peeled off from the area surrounding the occlusion site. Once all vitreous and ILM were removed from the embolus site, 25 Ga vertical scissors were used to perform a longitudinal incision in the artery at the occlusion site. During this step of the procedure, the infusion pressure was temporarily elevated to approximately 60 mmHg to minimize the risk of bleeding. Intraocular 25 Ga end-gripping forceps were then used to grasp and remove the exposed embolus. When removing the second and most proximal portion of the embolus, the maneuvers with the forceps tore the cilioretinal artery along with the occluded branch, resulting in massive bleeding. Emergency hemostatic procedures included the injection of perfluorocarbon liquids, endodiathermy, laser burns directly and around the bleeding site, and gas tamponade (SF6).
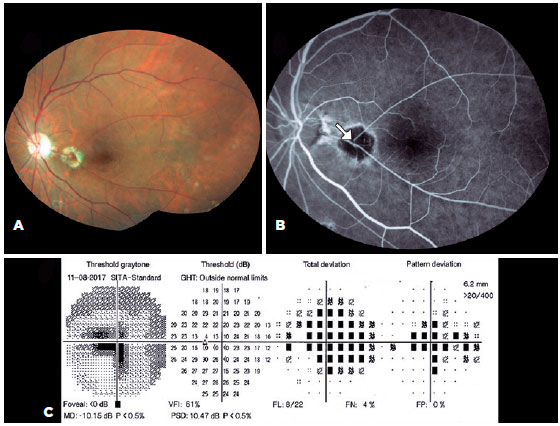
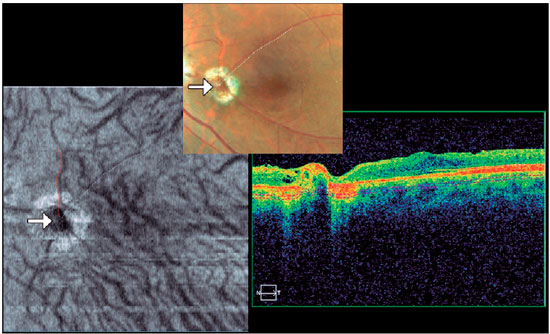
Three months after surgery, visual field testing showed that, although the central scotoma enlarged nasally, best corrected visual acuity improved to 20/400, and the temporal scotoma decreased. Fluorescein angiography showed recovery of the blood flow in the previously occluded vessel. However, the flow appeared not to be continuous with the flow of the cilioretinal artery (Figure 2), which led us to suspect that a retinochoroidal anastomosis had inadvertently occurred. En face OCT imaging at the level of the choroidal Haller-Sattler layers showed the continuous flow of the previously obstructed vessel with the choroidal capillary network, which further supports the idea of a retinochoroidal anastomosis (Figure 3). A video recap of the surgical technique is provided.
DISCUSSION
Surgical embolectomy is a controversial technique of limited benefit in cases of retinal artery occlusions. Given the acute ischemic damage due to the total occlusion of the artery, prompt reperfusion is thought to be crucial to maximize the visual benefits(1-6). Medical treatment options are considered not useful or to yield inconsistent or borderline results. However, they are safer because of their non-invasive nature(1). More invasive options, like the intra-arterial injection of tissue plasminogen activator, offer no substantial benefits despite increasing the risk of serious adverse events(1). Transluminal Nd: YAG laser therapy has been used to photo-disrupt obstructive emboli with promising visual outcomes. Nevertheless, there are reports of significant vitreous hemorrhage and collateral tissue damage with this technique(6).
Peyman successfully performed the first surgical embolectomy in 1990(2). Since then, 13 case reports of surgical embolectomy have been published, with reperfusion of the occluded artery and visual acuity improvement achieved in most cases(2-5).
Our patient referenced 7 days of decreased vision. Although surgery was performed outside the commonly described therapeutic window(1) and there was a rupture of the obstructed vessels during the surgical procedure, the arterial flow was reestablished, and visual fields testing suggested that the temporal scotoma improved.
On the basis of the experimental models of central retinal artery occlusion (CRAO) in rhesus monkeys, the retina suffers no damage for up to 97 min after an acute CRAO, but the damage is massive and irreversible after 4 h. Therefore, no treatment instituted after 4 h from the onset of the arterial occlusion can logically restore any vision in the setting of complete obstruction. Additionally, this model showed that the more protracted the ischemia, the longer the time to recovery.
A complete CRAO is a rare event in humans. Evidence from early studies indicated that treatment should be initiated within 24 h from the original insult. However, there may be cases where the therapeutic window can be extended. Owing to its uncommon presentation and high variability in onset time, clinical trials have been limited in sample size and therefore lack sufficient statistical power to detect small treatment benefits, primarily in patients considered to be outside the recommended therapeutic window. For a new therapy to have a significant impact on the management of retinal artery occlusion, it would need to at least double or triple the success rate of conventional therapeutic options(1-6).
In our patient, nasal enlargement of the central scotoma could be a consequence of the intense laser burns applied to the retina during the emergency hemostatic procedures. The intensity of the thermal injury could favor the formation of a retinochoroidal anastomosis, leading to the reperfusion of the affected area with secondary improvement of the temporal scotoma. Nonetheless, there is a possibility that the fluorescein angiography image is indicating spontaneous reperfusion, which is common in the subacute phase of retinal artery occlusions(1).
One of the most commonly reported complications of embolectomy is vitreous hemorrhage, which occurs in almost 30% of patients that undergo this surgical technique(2-5). Garcia-Arumí et al.(3) reported that reperfusion was not achieved in one of the patients in their series.
Several authors have reported that treatment with lasers might induce the formation of retinochoroidal anastomosis in vein occlusions, with an improvement of the perfusion status of the retina(7). It is unclear whether campimetric improvement of the patient could have been achieved without the laser burns. The reanastomosis of the ruptured arterial vessel might have taken longer to form, and ischemic damage to the retina would have been more significant.
REFERENCES
1. Patel PS, Sadda SR. Retinal Artery occlusions. In: Wilkinson CP, Hinton DR, Sadda SR, Wiedemann P, editors. Ryan´s Retina. Philadelphia (PA): Elsevier; 2018. p. 1136-50.
2. Peyman GA, Gremillion CM Jr. Surgical removal of a branch retinal artery embolus: a case report. Int Ophthalmol. 1990;14(4):295-8.
3. Garcia-Arumi J, Martinez-Castillo V, Boixadera A, Fonollosa A, Corcostegui B. Surgical embolus removal in retinal artery occlusion. Br J Ophthalmol. 2006;90(10):1252-5.
4. Ramchandran RS, Fekrat S. Embolectomy for branch retinal arterial occlusion. Retin Cases Brief Rep. 2010;4(2):116-9.
5. Almeida DR, Mammo Z, Chin EK, Mahajan VB. Surgical embolectomy for fovea-threatening acute retinal artery occlusion. Retin Cases Brief Rep. 2016;10(4):331-3.
6. Hsu TK, Chen SJ, Lei J, Wu Z, Lin CC, Chen MM, et al. Embolus-induced branch retinal artery occlusion with a presenting best-corrected visual acuity of 6/12 and visual field defect: YAG embolectomy safely restores arteriolar perfusion and/or visual function. Retin Cases Brief Rep. 2013;7(3):210-6.
7. Browning DJ. Fundus photographic, fluorescein angiographic, and indocyanine green angiographic signs in successful laser chorioretinal venous anastomosis for central retinal vein occlusion. Ophthalmology. 1999;106(12):2261-8.
Submitted for publication:
February 21, 2018.
Accepted for publication:
April 17, 2018.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose