

Silvana Artioli Schellini1,2; Roberta Lilian Fernandes de Souza Meneghim1; Larissa Satto1; Pedro Cavinatto1; Alicia Galindo-Ferreiro2; Rajiv Khandekar2
DOI: 10.5935/0004-2749.20180080
ABSTRACT
Purposes: The purpose of this study was to evaluate the magnitude and determinants of bilateral blindness and visual impairment (VI) in the southwest region of São Paulo State, Brazil.
Methods: This cross-sectional study conducted during 2013 and 2014 targeted people of all ages in 10 districts in the southwest region of São Paulo State, Brazil. Ophthalmologists in a mobile unit measured visual acuity and examined eyes. Visual acuity was categorized according to the World Health Organization sex-adjusted rates with 95% confidence intervals (CI) were calculated. Number of blindness and visually impaired was projected for the entire study area.
Results: We examined 2,306 participants. The age- and sex-adjusted frequency of bilateral blindness was 0.26% (95% CI: 0.1-0.4). Females (0.35%) and patients ≥50 years old (0.58%) had higher rate of blindness compared with males and younger individuals. The rate of severe VI was 9.1% (95% CI: 8.8-10.6) and was higher among males (11.6%) and those ≥50 years (12.3%). There could be 880 people with bilateral SVI in the study area. Bilateral severe VI was attributed to cataracts in 63% and was attributed to refractive error in 18%.
Conclusion: Visual impairment and blindness in the study population was low and mainly due to cataract and refractive errors. Initiatives should be addressed by health care services to further reduce avoidable blindness in the region.
Keywords: Visual impairment; Blindness; Cataract; Refractive errors; Brazil
RESUMO
Objetivos: O objetivo deste estudo foi avaliar a magnitude e determinantes da cegueira bilateral e deficiência visual (DV) na região sudoeste do estado de São Paulo, Brasil.
Métodos: Trata-se de um estudo transversal do qual participaram pessoas de todas as idades, habitantes de 10 distritos da região sudoeste do estado de São Paulo - Brasil, nos anos de 2013-
2014. Oftalmologistas avaliaram a acuidade visual e realizaram exame oftalmológico usando uma unidade móvel. A acuidade visual foi categorizada seguindo os critérios da Organização Mundial de Saúde. Foi calculada a taxa ajustada por idade-sexo e o intervalo de confiança de 95% para estimar o número de cegos e deficientes visuais na população.
Resultados: Foram examinadas 2.306 pessoas. A frequência de cegueira bilateral ajustada por idade e sexo foi de 0,26% (95% CI: 0,1-0,4). Mulheres (0,35%) e indivíduos ≥50 anos (0,58%) foram os que tiveram maior taxa de cegueira. A taxa de deficiência visual grave foi de 9,1% (95% CI: 8,8-10,6), ocorrendo mais em homens (11,6%), com idade ≥50 anos (12,3%). Estimativas indicaram existência de 880 pessoas com deficiência visual grave bilateral na região. Catarata (63%) e erros refrativos (18%) foram as principais causas de deficiência visual grave.
Conclusão: Deficiência visual grave e cegueira na região estudada foram baixas, sendo as causas mais frequentes a catarata e os erros de refração. Os serviços de saúde precisam implementar iniciativas para reduzir as causas evitáveis de cegueira na região.
Descritores: Deficiência visual; Cegueira; Catarata; Erros de refração; Brasil
INTRODUCTION
The global estimate of visually impaired (VI) worldwide in 2017 was 253 million (blindness in 36 million and moderate-to-severe visual impairment in 217 million)(1). Globally, 81% of individuals with blindness or VI are ≥50 years old(1). The prevalence of blindness and VI as well as the causes vary around the world(1) and within Latin American countries(2). Accurate data are crucial for planning for and monitoring the progress of VISION 2020: The Right to Sight global initiative to eliminate avoidable blindness in all member countries(3).
Brazil is within the region of the Americas designated by the World Health Organization(4). Based on the census of 2010, the estimated population of Brazil in 2014 was 200 million(4). Demographically, nearly one-fourth of the population is below 15 years of age, and only one-tenth is 60 years and older(4). Although agriculture is the main economic activity, 87% of the population resides in urban areas(4). The per capita gross domestic product of Brazil in 2014 was US$5.97(5). Despite Brazil is rapidly evolving economy, poverty remains an important issue and has an impact on access to appropriate ophthalmic care(6).
Prior to 2010 there were several assessments of VI and blindness in Brazil and specifically in Sao Paulo State(7-9). However, updating information on eye disease in the same region will be helpful in evaluating progress in the health sector, particularly that of eye health care.
Sao Paulo State is in southwest Brazil and has 17 health regions(10). The region of the present study is composed of 68 municipalities(10) with approximately 2,500,000 inhabitants. In many of the small cities in this health region, primary health care alone is provided; ophthalmic care is not available in those cities. However, the University Hospital of Botucatu Medical School, a tertiary reference eye center, has provided outreach eye care services for this region over the past decade. This care is delivered through a mobile ophthalmic unit visiting a particular city once a week on request. In addition to providing care, the unit generates information on visual disabilities through a community-based study with a view to enhancing eye care services in the region. The purpose of this study, based on data collected through this service delivery program, was to evaluate magnitude and determinants etiologies of visual impairment VI and blindness in the southwest region of São Paulo State, Brazil.
METHODS
A cross-sectional study using a convenience sample from the eye care service delivery program described above was carried out in 10 districts of the southwest region of São Paulo State, Brazil, during 2013 and 2014. The Ethics Committee in Human Research from the Botucatu Medical School approved the study protocol.
The target population comprised all individuals residing in the study area and registered in the basic health units of the municipalities. Local health authorities invited all residents in need of ophthalmic care to attend the mobile clinic. We included in the study all those agreeing to take part, excluding only those declining to participate.
The study team comprised four ophthalmologists and four mid-level eye care professionals trained in the study methodology. A mobile ophthalmic unit stationed within each health community center was used for a complete eye examination of each participant. Data were collected on age, sex, location of residence, and eye disease.
Uncorrected visual acuity (VA) was measured for each eye using an illuminated Snellen E chart placed 6 m from the participant. Vision was again tested with spectacles to measure presenting VA for distance. If the participant was unable to read the letter on the top line of the chart, testing was repeated at a distance of 1 m. If the patient could not see the top line at 1 m, the vision was tested and recorded as counting fingers, seeing hand movements, light perception, or no light perception. If the presenting VA was less than 6/6, an objective refraction was performed and the best-corrected visual acuity (BCVA) from this refraction was noted. For participants <40 years of age, cycloplegic refraction was performed. Cycloplegia was achieved by instilling one drop of 1% cyclopentolate in each eye, which was repeated after five minutes a maximum of three times. For patients >5 years old, intraocular pressure (IOP) was measured with a noncontact pneumotonometer (CT-60 Computerized Tonometer, Topcon Corp., Tokyo, Japan). The mean of three measurements was recorded as the IOP of each eye. If the IOP was >25 mmHg, the measurements were repeated using a Goldman applanation tonometer (Haag Strait, Bern, Switzerland). Slit lamp biomicroscopy (BQ-900, Haag Strait) was performed to evaluate the anterior segment. Posterior segment evaluation was performed with a 90D Volk lens and a slit lamp. To ensure consistent quality, the study staff were trained and periodically monitored and the equipment was frequently calibrated. All data collection forms were pretested.
Participants who required further clinical or surgical management were referred to the Botucatu Medical School university hospital. The final diagnosis of visual disability was based on comprehensive eye assessment, further investigations as indicated, and an expert ophthalmologist’s opinion.
The International Classification of Diseases Update and Revision 2006-version 10 was used to grade VI(11). Severe VI (SVI) was defined as a BCVA of <6/60 in the better eye and a corresponding restriction in the field of vision. Moderate VI (MVI) was defined as the BCVA of <6/18 to ≥6/60 in the better eye. Blindness was defined as a BCVA worse than 3/60.
Data were collected on a form and then transferred to an Excel spreadsheet (Microsoft Corp., Redmond, WA, USA). Data were then analyzed with the Statistical Package for Social Studies (SPSS 19.0; IBM Corp., New York, NY, USA). Univariate analysis was performed with a parametric method.
The participants were grouped based on age: <20 years; 21 to 50 years; and >50 years. The crude rates of VI for each sex and age group for each city were calculated, after which age-sex-standardized rates with 95% confidence intervals (CI) were calculated. Based on the population in our sample, we projected the possible number of individuals with visual disabilities in the study area.
RESULTS
Senior citizens were over represented in the study compared with children and working-age adults, confirming that standardizing the rates for age and sex was essential (Table 1).
There were six patients with bilateral blindness, for an age-sex-adjusted rate of 0.26% (95% CI: 0.1 to 0.4). Female participants (0.35%) and those 50 years and older (0.58%) had higher rate of blindness compared with males and younger individuals (Table 2).
The rate of SVI in the study population was 9.1% (95% CI: 8.8-10.6), affecting mainly males and those older than 50 years (Table 3). The rate of MVI was estimated to be 19.1% (95% CI: 18.8-20.2), affecting primarily females and individuals over 50 years of age (Table 4).
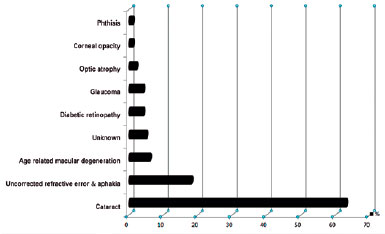
SVI was noted on presenting VA testing in 164 (8.1%) participants over the age of 20, of whom 104 (63.4%) still had SVI with BCVA. The main causes of SVI were cataracts (30.5%) and uncorrected refractive errors (RE) or uncorrected aphakia (10.5%) (Figure 1). Among participants younger than 20 years, 46 (1.9% of the entire sample of 2306) had SVI based on uncorrected VA, of whom only five had BCVA less than 3/60 in the better eye. This was due in one to cataract and in four to uncorrected RE or uncorrected aphakia. VI due to ocular infections was uncommon in this population.
Among the 1,032 participants over age 50, cataract was the principal cause of bilateral blindness in four participants (0.4%) and of SVI in 80 participants (7.8%). Thus, among those over age 50 in the study area population, as many as 9,000 individuals could be blind due to cataract and 17,000 individuals could have SVI secondary to cataract.
Based on 18% of the total study sample with SVI due to uncorrected RE, it is estimated that 50,000 people of all ages in the study area require spectacles or other visual aids for vision correction.
DISCUSSION
Our study evaluated the magnitude and determinants of blindness and VI in a convenience sample of individuals attending a mobile ophthalmic unit in São Paulo State, Brazil. The use of a mobile ophthalmic unit to study a convenience sample is uncommon in epidemiologic studies and could be an alternative to undertaking similar studies while providing assistance, allowing simultaneous collection of data and provision of eye care services
We estimated 0.26% of bilateral blindness of 0.26% among residents of the municipalities covered in this study. This result from a convenience sample of people actively seeking ophthalmic care may overestimate the true prevalence in the general population. Thus, the actual blindness rates in the community could be lower than 0.26%. A cross-sectional study performed a decade earlier in the same region reported a 0.4% prevalence of blindness (95% CI: 0.2 to 0.6)(9). The lower rate in our study might reflect the impact of continuous mobile eye care services provided in the region in the past 10 years.
Among individuals older than 50 years in our study, the blindness rate was 0.58%. A population-based survey in 2005 evaluating individuals older than 50 years from Sao Paulo City, Sao Paulo State, Brazil, was 1.5%(8). That study was completed 10 years earlier than ours, and differences in access to eye care services between the two different studied regions of Sao Paulo State or in the study design may account for the discrepancy in the results.
In Latin America, the prevalence of blindness among individuals older than 50 years reportedly varies from 0.7% (95% CI: 0.4-1.0) in Argentina to 3.0% (95% CI: 2.3-3.6) in Panama(2). The global estimate of the prevalence of bilateral blindness in 2017 was 0.48%(1), higher than that in the present study and comparable to that in industrialized countries(12).
The prevalence of SVI in our study was 9.7%, which is higher than the 7.4% reported in a similar area in 2009(9), but is lower than the rate reported in Campinas, Sao Paulo State, in 2003(7). Differences in sampling procedures among different study populations likely explains the discrepancies between results.
The rate of SVI in the present study was lower than that in El Salvador (14%)(2), but was much higher than the global estimated prevalence of SVI and MVI combined (2.95%), for all ages(1). These differences may be related to sampling techniques and may also reflect the variability in access to eye care services within the regions studied.
The proportion of females in the study population was higher than the females, in our sample and there were more women who were blind. The overrepresentation of females in our study can be because of longer life expectancy for women compared with men in Brazil(4), or it may be because outreach activities such as the mobile eye care unit can bridge the sex gap in developing countries. Another explanation may be the characteristics of the study region, which is mostly comprised of small cities where men are the labor force, while most women undertake domestic chores. Thus, women might find it easier to attend community health projects such as ours. In addition, as men are the income earners in this region, they may have the funds to seek eye services at hospitals, while women are less likely able to afford hospital care. They might therefore be more likely to take advantage of community-based, low-cost services.
We adjusted the rates of visual disability based on age and sex to obtain an accurate estimate for the study area as a whole and to allow comparison with other studies of visual disabilities. We found a very low rate of visual disabilities in children under 20 years old. The sample required for a prevalence study should be large; hence outcomes from this relatively small subgroup of children should be interpreted with caution. Our study may also have some bias because senior citizens over 50 years old were overrepresented in the sample, both in relation to the general Brazilian population and in comparison with children and working-aged adults.
The current study enrolled subjects of all ages. However, the WHO recommends surveys targeting individuals ≥50 years old in countries with limited resources, an undertaking known as the Rapid Assessment for the Prevention of Blindness(2,13,14). Numerous studies from Latin America based on this program or on the Rapid Assessment of Cataract Surgical Services have involved samples of individuals ≥50 years old(2,7,8,15,16), although other prevalence surveys have included individuals 40 years and older(12), and WHO estimates include all ages(1).
Approximately 6% of the population in the study area is comprised of individuals ≥50 years. Undertaking a survey only of that age group may be cost effective, but it will eliminate a large population of younger people from surveys designed to enhance effective eye-care planning(13,18). Such surveys fail to address the problem of visual disability in the entire community, depriving younger age groups of the planning needed to reduce visual disability throughout the population of interest.
Blindness in children was not detected in our study. The adjusted prevalence of bilateral SVI for patients <20 years old was 12.5%. The causes of SVI in this particular group were the same as in adults (cataract and RE), although REs were more important than cataracts in this young subgroup.
The finding that cataract (63%) and uncorrected RE (18%) were the main causes of SVI in our study corresponds with the findings of another study in the same region noting that these two etiologies contributed to 85% of VI(9,19). In Campinas, Sao Paulo State, 41% of blindness was due to cataract(7). The difference between our results and those of the Campinas study is likely related to study design, as we used a convenience sample and the Campinas study used a population-based sample. The causes of blindness in the current study are similar to data from other countries, for example, cataract is responsible for 25%(1) to 33%(20) of blindness globally.
The ophthalmic services in the study area should be enhanced to provide care for the projected numbers of patients with cataract-related disability, whether 9,000 with blindness or 17,000 with SVI. Notably, bilateral cataract surgery is required for disabled individuals, so the resources required would be double that of the number of individuals needing it.
Measuring both the presenting VA and the BCVA allowed us to highlight the role of uncorrected RE as a cause of visual disability in the study area. We found that RE was the second most common cause of SVI, with prevalence of 2.1% in our sample. Nearly one-fourth of the population had uncorrected RE causing some degree of VI. A cross-sectional study in the same area reported that 13.8% of subjects had uncorrected RE, with a prevalence of optically reversible low vision of 4.6% and of blindness of 1.8%(21). The 2.1% prevalence of visual disability due to uncorrected RE in our study is in line with previous data from Brazil (2.3%)(22), Colombia (1.4%)(23), and Chile (2.1%)(24), while this prevalence of visual disability due to uncorrected RE is lower than that in Venezuela (5.0%)(25).
We estimated that 50,000 people in the total population require spectacles to improve their VI. The high percentage of SVI due to uncorrected RE in our study is of particular concern, indicating the urgent need to establish affordable refractive services in smaller cities like those in our study area. Beyond this, mobile units can provide access for populations where local services for refraction are unavailable. We recommend the provision of low-cost visual aids and education encouraging the use of visual aids in the target population.
Other causes of SVI in our population were related to posterior segment pathologies such as age-related macular degeneration (AMD) in 6%, diabetic retinopathy (DR) in 4%, and optic nerve atrophy in 2%. The proportion of AMD is higher in developed countries and in high-income regions(26). A study from Sao Paulo City, Brazil, reported that AMD contributed to 16.4% of new cases of blindness(27). The prevalence of AMD in Latin America is 15%(28), contributing to 5% of blindness or 4% of VI globally(1). The low presentation of AMD in our study could be due to a large proportion of patients with significant cataracts precluding posterior segment examination or because the age structure of our sample did not precisely match the age structures of population-based studies. Another cause could be the manner in which the data was collected, with the listing of a preventable or curable disorder as a principal cause of VI seen as a priority in the mobile units in our study, so that less attention was paid to AMD.
DR was responsible for SVI in 4% of our sample. In another study from the same geographic area as ours, the prevalence of type 2 diabetes and DR was 8.7% and 7.6%, respectively(29). The lower rate of SVI due to DR in our population could be due to the continued provision of eye care in the study area over the past 10 years. Changing lifestyles in these communities will likely result in decreases in the prevalence of metabolic diseases such as diabetes. Health care providers should plan for a reduction in the frequence of diabetes and its associated comorbidities.
Glaucoma was responsible for 4% of SVI in our sample. A previous study from the same region reported the same 4% prevalence of glaucoma(7), and 7.4% of blindness in Brazil is due to glaucoma(30). However, the prevalence of glaucoma-related visual disability was lower in our study compared with other Latin American countries, including Honduras (21.1%), Paraguay (15.6%), Uruguay (14.3%), Peru (13.7%), and Panama (10.2%)(2,16).
The strength of the present study is the sample size, the opportunity to assess individuals in their own community using a mobile unit which favored participation, and data based on a complete ophthalmic exam done by a trained team of ophthalmologists.
Limitations of our study include the use of a convenience sample recruited through a program offering ophthalmic care to a specific population rather than to a population-based sample. Our results, then, are not precisely representative of the general population. However, our design allowed data collection for projecting future resource requirements at the same time as that when we rendered care to individuals in need. Another limitation is the fact that we did not include standard assessment of visual field defects to define blindness and SVI. This may have resulted in underrepresentation of certain types of visual disabilities.
In conclusion, we found that individuals presenting for eye care in the study area had a lower prevalence of blindness and SVI compared with previous estimates. Visual disabilities were more prevalent in females and in those individuals aged 50 years or older. Cataract not operated and uncorrected RE remain the most common causes of VI. These issues must be urgently addressed to attain the goals of VISION 2020 in our region.
REFERENCES
1. Bourne RR, Flaxman SR, Braithwaite T, Cicinelli MV, Das A, Jonas JB et al. Vision Loss Expert Group. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(9):e888-97.
2. Silva JC, Mújica OJ, Vega E, Barcelo A, Lansingh VC, McLeod J et al. A comparative assessment of avoidable blindness and visual impairment in seven Latin American countries: prevalence, coverage, and inequality. Rev Panam Salud Publica. 2015;37(1):13-20.
3. Pizzarello L, Abiose A, Ffytche T, Duerksen R, Thulasiraj R, Taylor H et al. VISION 2020: The Right to Sight: a global initiative to eliminate avoidable blindness. Arch Ophthalmol. 2004;122(4):615-20.
4. Brazil Demographics Profile. 2014 [Internet]. IndexMundi; 2018. [cited 2018 Feb 22]. Available from: http://www.indexmundi.com/brazil/demographics_profile.html
5. World Health Organization (WHO). Global health indicators. [Internet]. Geneve: WHO; 2012. [cited 2018 Feb 22]. Available from: http://www.who.int/healthinfo/EN_WHS2012_Part3.pdf
6. Product GD. (GDP) in Brazil [Internet]. 2014. Traiding Economics; c2018. [cited 2018 Feb 22]. Available from: http://www.tradingeconomics.com/brazil/gdp
7. Eduardo Leite Arieta C, Nicolini Delgado AM, José NK, Temporini ER, Alves MR, de Carvalho Moreira Filho D. Refractive errors and cataract as causes of visual impairment in Brazil. Ophthalmic Epidemiol. 2003;10(1):15-22.
8. Salomao SR, Cinoto RW, Berezovsky A, Araujo-Filho A, Mitsuhiro MR, Mendieta L et al. Prevalence and causes of vision impairment and blindness in older adults in Brazil: the Sao Paulo Eye Study. Ophthalmic Epidemiol. 2008;15(3):167-75.
9. Schellini SA, Carvalho GM, Rendeiro FS, Padovani CR, Hirai FE. Prevalence of diabetes and diabetic retinopathy in a Brazilian population. Ophthalmic Epidemiol. 2014;21(1):33-8.
10. São Paulo (Estado) Secretaria de Estado da Saude. Governo do Estado de São Paulo, Brazil http://www.saude.sp.gov.br/ses/institucional/departamentos-regionais-de-saude. Online accessed on 27/10/2017.
11. World Health Organization (WHO). Change the definition of blindness [Internet]. Geneve: WHO; [cited 2018 Feb 22]. Available from: http://www.who.int/blindness/ChangetheDefinitionofBlindness.pdf?ua=1
12. Varma R, Kim JS, Burkemper BS, Wen G, Torres M, Hsu C et al.; Chinese American Eye Study Group. Prevalence and Causes of Visual Impairment and Blindness in Chinese American Adults: The Chinese American Eye Study. JAMA Ophthalmol. 2016 ;134(7):785-93.
13. Resnikoff S, Keys TU. Future trends in global blindness. Indian J Ophthalmol. 2012;60(5):387-95.
14. Limburg H, Silva JC, Foster A. Cataract in Latin America: findings from nine recent surveys. Rev Panam Salud Publica. 2009;25(5): 449-55.
15. Furtado JM, Lansingh VC, Carter MJ, Milanese MF, Peña BN, Ghersi HA et al. Causes of blindness and visual impairment in Latin America. Surv Ophthalmol. 2012;57(2):149-77.
16. Silva JC. National surveys of avoidable blindness and visual impairment in Argentina, El Salvador, Honduras, Panama, Peru, and Uruguay. Rev Panam Salud Publica. 2014;36(4):209-13.
17. Limburg H, Espinoza R, Lansingh VC, Silva JC. Functional low vision in adults from Latin America: findings from population-based surveys in 15 countries. Rev Panam Salud Publica. 2015;37(6):371-8.
18. Gupta N, Kocur I. Chronic eye disease and the WHO Universal Eye Health Global Action Plan 2014-2019. Can J Ophthalmol. 2014 Oct;49(5):403-5.
19. Schellini SA, Durkin SR, Hoyama E, Hirai F, Cordeiro R, Casson RJ et al. Prevalence and causes of visual impairment in a Brazilian population: the Botucatu Eye Study. BMC Ophthalmol. 2009;9(1):8.
20. Bourne RR, Stevens GA, White RA, Smith JL, Flaxman SR, Price H et al.; Vision Loss Expert Group. Causes of vision loss worldwide, 1990-2010: a systematic analysis. Lancet Glob Health. 2013;1(6): e339-49.
21. Ferraz FH, Corrente JE, Opromolla P, Schellini SA. Influence of uncorrected refractive error and unmet refractive error on visual impairment in a Brazilian population. BMC Ophthalmol. 2014; 14(1):84.
22. Arieta CE, de Oliveira DF, Lupinacci AP, Novaes P, Paccola M, Jose NK et al. Cataract remains an important cause of blindness in Campinas, Brazil. Ophthalmic Epidemiol. 2009;16(1):58-63.
23. Ramırez VG, Serrano JJ, Villamizar LA. Prevalencia de ceguera en el Departamento de Santander-colombia. MedUNAB. 2009;12:66-73.
24. Barrıa F. Reporte de actividades de prevencion de ceguera en Chile. Arch Chil Oftalmol. 2005;62:9-14.
25. Siso F, Esche G, Limburg HT. Test Nacional de Catarata Servicios Quirúrgicos. Primera Encuesta Nacional. Rev Oftalmol Venez. 2005; 61:112-39.
26. Bourne R, Price H, Taylor H, Leasher J, Keeffe J, Glanville J, et al. Global Burden of Disease Vision Loss Expert Group. New systematic review methodology for visual impairment and blindness for the 2010 Global Burden of Disease study. Ophthalmic Epidemiol. 2013;20(1):33-9.
27. Salomão SR, Soares FS, Berezovsky A, Araújo-Filho A, Mitsuhiro MR, Watanabe SE, et al. Prevalence and outcomes of cataract surgery in Brazil: the São Paulo eye study. Am J Ophthalmol. 2009; 148(2):199-206.e2.
28. Bourne R, Price H, Stevens G, Group GB; GBD Vision Loss Expert Group. Global burden of visual impairment and blindness. Arch Ophthalmol. 2012;130(5):645-7.
29. Schellini SA, Carvalho GM, Rendeiro FS, Padovani CR, Hirai FE. Prevalence of diabetes and diabetic retinopathy in a Brazilian population. Ophthalmic Epidemiol. 2014;21(1):33-8.
30. Salomão SR, Mitsuhiro MR, Belfort R Jr. Visual impairment and blindness: an overview of prevalence and causes in Brazil. An Acad Bras Cienc. 2009;81(3):539-49.
Submitted for publication:
November 7, 2017.
Accepted for publication:
February 16, 2018.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Approved by the following research ethics committee: Faculdade de Medicina de Botucatu, Universidade Estadual Paulista (# 50/2015)