

Dilay Ozek1; Ozlem Evren Kemer1; Pinar Altiaylik2
DOI: 10.5935/0004-2749.20180089
ABSTRACT
Purpose: We aimed to evaluate the visual quality performance of scleral contact lenses in patients with keratoconus, pellucid marginal degeneration, and post-keratoplasty astigmatism, and their impact on quality of life.
Methods: We included 40 patients (58 eyes) with keratoconus, pellucid marginal degeneration, and post-keratoplasty astigmatism who were examined between October 2014 and June 2017 and fitted with scleral contact lenses in this study. Before fitting scleral contact lenses, we noted refraction, uncorrected distance visual acuity, spectacle-corrected distance visual acuity, uncorrected contrast sensitivity, and spectacle-corrected contrast sensitivity. We performed corneal topography on and applied a questionnaire that included the National Eye Institute Visual Functioning Questionnaire to all participants. We recorded corrected contrast sensitivity and corrected distance visual acuity on the third month after fitting scleral contact lenses and requested that subjects repeat the National Eye Institute Visual Functioning Questionnaire.
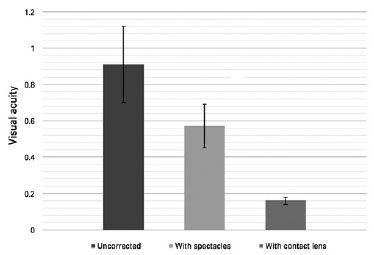
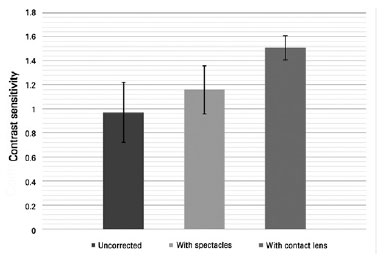
Results: The mean age of patients was 28.12 ± 13.19 years. Mean logMAR uncorrected distance visual acuity, spectacle-corrected distance visual acuity, and corrected distance visual acuity with scleral contact lenses were 0.91 ± 0.21 (0.40-1.80), 0.57 ± 0.12 (0.10-1.80), and 0.16 ± 0.02 (0.00-1.30), respectively. We observed significantly higher corrected distance visual acuity with scleral contact lenses compared with uncorrected distance visual acuity and spectacle-corrected distance visual acuity (p<0.05). Mean uncorrected contrast sensitivity, spectacle-corrected contrast sensitivity and CCS with scleral contact lenses were 0.97 ± 0.12 (0.30-1.65), 1.16 ± 0.51 (0.30-1.80), and 1.51 ± 0.25 (0.90-1.80), respectively. Significantly higher contrast sensitivity levels were recorded with scleral contact lenses compared with those recorded with uncorrected contrast sensitivity and spectacle-corrected contrast sensitivity (p<0.05). We found the National Eye Institute Visual Functioning Questionnaire overall score for patients with scleral contact lens treatment to be significantly higher compared with that for patients with uncorrected sight (p<0.05).
Conclusion: Scleral contact lenses are an effective alternative visual correction method for keratoconus, pellucid marginal degeneration, and post-keratoplasty astigmatism. A significant increase in visual acuity and contrast sensitivity can be obtained with scleral contact lenses in patients with irregular corneas.
Keywords: Keratoconus; Corneal topography; Contrast sensitivity; Sclera; Contact lenses; Sickness impact profile; Visual acuity; Quality of life
RESUMO
Objetivo: Avaliar o desempenho da qualidade visual das lentes de contato esclerais em pacientes com ceratocone, degeneração marginal transparente e astigmatismo pós-ceratoplastia e seu impacto na qualidade de vida.
Métodos: Foram incluídos 40 pacientes (58 olhos) com ceratocone, degeneração marginal transparente ou astigmatismo pós-ceratoplastia que foram examinados entre outubro de 2014 e junho de 2017 e adaptados com lentes de contato esclerais neste estudo. Antes de ajustar as lentes de contato esclerais, registrou-se refração, acuidade visual à distância não corrigida, acuidade visual à distância corrigida por óculos, sensibilidade ao contraste não corrigida e sensibilidade ao contraste corrigida por óculos. Realizamos topografia da córnea e aplicamos um questionário que incluía o Questionário de Funcionamento Visual do National Eye Institute para todos os participantes. Registramos a sensibilidade ao contraste corrigida e corrigimos a acuidade visual à distância no terceiro mês após a adaptação das lentes de contato esclerais e solicitamos aos participantes que repetissem o Questionário de Funcionamento Visual do National Eye Institute.
Resultados: A idade média dos pacientes foi de 28,12 ± 13,19 anos. A acuidade visual à distância não corrigida logMAR média, a acuidade visual à distância corrigida por óculos e a distância visual corrigida com as lentes de contato esclerais foram 0,91 ± 0,21 (0,40-1,80), 0,57 ± 0,12 (0,10-1,80), 0,16 ± 0,02 (0,00-1,30), respectivamente. Observamos uma acuidade visual à distância corrigida significativamente maior com lentes de contato esclerais em comparação à acuidade visual à distância não corrigida e à acuidade visual à distância corrigida por óculos (p<0,05). Sensibilidade ao contraste médio não corrigido, sensibilidade ao contraste corrigida por óculos e CCS com lentes de contato esclerais foram 0,97 ± 0,12 (0,30-1,65), 1,16 ± 0,51 (0,30-1,80), 1,51 ± 0,25 (0,90-1,80), respectivamente. Significativamente maiores níveis de sensibilidade ao contraste foram registrados com lentes de contato esclerais em comparação com aqueles registrados com sensibilidade ao contraste não corrigida e sensibilidade ao contraste corrigida por óculos (p<0,05). Descobrimos que a pontuação geral do Questionário de Funcionamento Visual do National Eye Institute para pacientes em tratamento com lentes de contato esclerais é significativamente maior em comparação com pacientes com visão não corrigia (p<0,05).
Conclusão: As lentes de contato esclerais constituem um método alternativo eficaz de correção visual alternativa para o ceratocone, degeneração marginal transparente e o astigmatismo pós-ceratoplastia. Um aumento significativo na acuidade visual e sensibilidade ao contraste pode ser obtido com lentes de contato esclerais em pacientes com córneas irregulares.
Descritores: Ceratocone; Topografia da córnea; Sensibilidade de contraste; Esclera; Lentes de contato; Perfil de impacto da doença; Acuidade visual; Qualidade de vida
INTRODUCTION
Keratoconus and pellucid marginal degeneration (PMD) are among the most common corneal ectasias. Keratoconus-the progressive thinning of the cornea with poor or distorted vision-is sometimes associated with photophobia as a result of irregular astigmatism(1). Pellucid marginal degeneration-a degenerative corneal condition-is characterized by a peripheral ectasia of the inferior cornea 1 mm-2 mm from the limbus. Soft and rigid gas permeable (RGP) lenses may, in mild to moderate ectasia cases, help to improve vision, but these lenses fail to improve vision in a satisfactory manner for severe cases, and patients may have to use other lenses, such as piggyback contact lenses, hybrid lenses, and scleral contact lenses (ScCLs)(2).
After keratoplasty, the main cause of visual impairment is astigmatism. Surgical or optical methods are generally used to manage high astigmatism and for visual rehabilitation and assessment of binocularity. Spectacles and various types of contact lenses are the most common non-surgical methods for the correction of post-keratoplasty astigmatism (PKA). For those with high/irregular astigmatism and those achieving unsatisfactory results with spectacles, contact lenses are the method of choice.
ScCLs are a group of rigid gas permeable lenses with large diameters. Their name derives from the fact that they completely cover the cornea and rest on the sclera. These lenses are indicated mainly for patients with the visual impairment, photophobia and irregular astigmatism seen in cases of keratoconus, PMD, keratoglobus, and PKA. Further candidates for ScCL use are patients with ocular surface diseases like Stevens-Johnson syndrome, dry eyes, graft-vs-host disease, and ocular cicatricial pemphigoids(3,4).
ScCL users benefit considerably from increased visual acuity and hence from improved quality of life (QoL). Many questionnaires evaluating the comfort of contact lens applications are currently in use. One of the most commonly used is the National Eye Institute Visual Functioning Questionnaire (NEI-VFQ 25), which applies to a wide age range and includes chronic eye diseases. It comprises 25 questions evaluating patients’ complaints and their visual performance, as they relate to general health, general vision, ocular pain, near activities, distance activities, social functioning, mental health and role difficulties, dependency, driving, color vision, and peripheral vision.
We evaluated our study with the first QoL questionnaire applied to scleral lens users and compared their visual acuity and contrast sensitivity results to those reported in the literature.
METHODS
The local Ethics Committee of our institution approved this study, which adhered to the tenets of the Declaration of Helsinki.
We included 58 eyes of 40 patients with the diagnoses of keratoconus, PMD, or PKA treated with mini or full Misa scleral lenses (Microlens® Netherlands) and followed up in our department between October 2014 and May 2017. Prior to ScCL treatment, we reviewed each patient’s medical history. We recorded uncorrected distance visual acuity (UDVA), CS, slit-lamp examinations, funduscopic evaluation, and Kmax and total corneal astigmatism values from corneal topographic examination (Pentacam HR, Oculus Optikgeräte GmbH, Wetzlar Germany). All participants completed a questionnaire (the National Eye Institute Visual Functioning Questionnaire NEI-VFQ 25). We determined the appropriate vault and diameter of ScCLs for each patient according to their corneal topographic Kmax values. We evaluated ScCL compliance of the cornea and conjunctiva with anterior segment optic coherence tomography (Casia swept-source OCT-1000, Tomey, Nagoya, Japan). We re-evaluated corrected distance visual acuity (CDVA) and CS three months after the initiation of the treatment. We re-applied the NEI-VFQ 25 questionnaire following at least 6 hours of continuous ScCL use and analyzed the results.
We excluded cases with any conditions that prevent therapeutic contact lens wear, such as keratitis, or any condition affecting visual acuity, such as retinal disorders and glaucoma, from the study.
We estimated visual acuity with logMAR (Smart System 2 2020 Visual Acuity System; M&S Technologies). We performed contrast sensitivity testing with the Hamilton-Veale chart in uncorrected and contact lens-corrected cases. This test is based on the Pelli-Robson contrast sensitivity test and includes a card with 16 pairs of letters over 8 lines. The patient read the letters and we recoreded the result as log contrast sensitivity [log (l/c)]. The range of the result was from 0 to 2.25 log units.
The same clinician performed the interviews for the application of the NEI-VFQ 25 questionnaire (Turkish version) and recorded the results(5). Higher scores indicated better QoL.
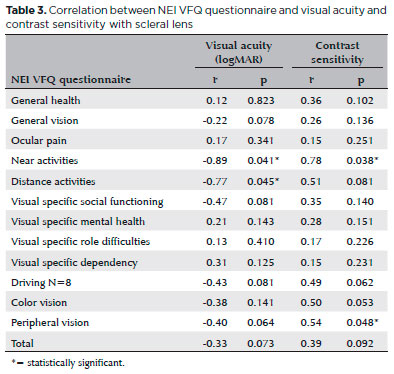
We performed the statistical analysis using SPSS 20.0 for Mac (SPSS, Inc, Chicago, IL). We performed a paired sample T-test to compare the results of the NEI VFQ 25 questionnaire, and an independent samples t-test to compare the visual acuity and contrast sensitivity before and after fitting ScCLs. We used the Pearson correlation coefficient to detect any correlation between the NEI VFQ-25 scores and clinical variables. We accepted a value of p<0.05 as statistically significant (Table 3).
RESULTS
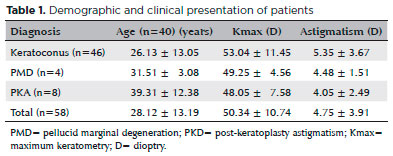
In our study, we diagnosed 46 eyes of 28 patients as having keratoconus, 4 eyes of 4 patients as having PMD and 8 eyes of 8 patients as having PKA. The mean age of patients (32 females and 28 males) was 28.12 ± 13.19 years (range 18 years-52 years). The mean follow-up time was 20.2 ± 5.2 months (4 months-28 months). The average CL wearing time was 10.7 ± 3.25 hours/day (5 hours/day-16 hours/day). The demographic and clinical features of cases are given in table 1.
The mean logMAR UDVA and SC-DVA were 0.91 (0.40-1.80) and 0.57 (0.10-1.80), respectively. CDVA with ScCL was 0.16 (0.00-1.30). We found CDVA to be higher with scleral lens use, compared to UDVA and SC-DVA (p=0.03, p=0.04) (Figure 1).
Mean logMAR UCS was 0.97 ± 0.12 (0.30-1.65) and SC-CS was 1.16 ± 0.51 (0.30-1.80). CCS with scleral lenses was 1.51 ± 0.25 (0.90-1.80). Contrast sensitivity scores were higher with ScCL use than with UCS and SC-CS (Figure 2).
Overall we found the NEI-VFQ scores of patients using ScCLs to be significantly higher than those with uncorrected vision (p=0.02). We recorded significantly higher general vision, distance activities, near activities, vision-specific social functioning, and peripheral vision score for ScCL use than for those with uncorrected vision (Table 2).
There was a positive correlation between CS and near activities and peripheral vision in NEI-VFQ subgroups (r=0.38, p=0.53; r=0.34, p=0.48, respectively). There was negative correlation between logMAR CDVA with scleral lenses, and distance activities and near activities in NEI-VFQ subgroups (r=-0.77, p=0.045; r=-0.89, p=0.041, respectively).
During the follow-up period, 3 keratoconus patients and 2 PKA patients informed us that they had given up wearing CLs after an average of 4 months due to difficulties in changing the saline solution needed for the application of ScCLs every 4 hours during a day. Two patients stopped CL treatment because of corneal hydrops and underwent keratoplasty surgery. We observed no other complications during the follow-up period.
DISCUSSION
Scleral lenses, when used in cases with irregular corneas, provide a smoother refractive surface and also minimize scarring by decreasing pressure on the corneal apex. Designs of Mini-scleral and scleral lenses introduced new opportunities to protect the cornea and assist in visual rehabilitation. ScCLs, since they cover the entire corneal surface and make contact on the relatively less sensitive surface of the sclera, are better tolerated and yield superior results for optical corrections in patients with corneal irregularities. These lenses also serve as a pre-corneal fluid reservoir, providing optical correction while offering rehabilitation and comfort for cases with contact lens intolerance, such as advanced cases of dry eye(6-8).
Various studies have reported improvement in visual acuity (VA) with ScCLs(9,10). VA was measured between 20/60 or better for 72% to 81.8% of PKA patients after ScCL treatment(11-13). Rocha et al., reported that 26 eyes (96.3%) achieved VA of ≥0.30 logMAR, and 21 eyes (77%) achieved an improvement of ≥2 VA lines relative to the CDVA with scleral lenses in PKA(14). In a study by Severinsky et al., 23 patients (82%) were reported to achieve a functional vision of 0.5 or more with ScCL use(15). Picot et al. reported a progression in VA from ± 0.46 to 0.15 ± 0.17 in patients with keratoconus and PKA with ScCL use for 6 months(16). In our study, the mean logMAR VA increased from 0.91 to 0.16 with ScCLs in patients with keratoconus, PMD and PKA.
Sabesan et al. measured CS with CSV-1000 on keratoconus patients fitted with ScCLs and found that it was also significantly improved by factors of 2.4, 1.8, and 1.4 on average for 4 cycles/degrees, 8 cycles/degrees, and 12 cycles/degrees, respectively (p<0.05 for all frequencies)(17). In our study, we detected mean logMAR CS values as 0.97 ± 0.12 (0.30-1.65) for uncorrected vision, 1.16 ± 0.51 (0.30-1.80) with spectacles, and 1.51 ± 0.25 (0.90-1.80) with CL with the Pelli-Robson test. Contrast sensitivity levels were recorded in cases with ScCLs compared with uncorrected cases and spectacle-corrected cases.
Assessment of quality of life (QoL) has recently come to be regarded as a valuable tool for the monitoring of successful treatment in ocular disorders. The NEI-VFQ, developed by Mangione et al. in 1998 for adult patients with chronic ocular diseases, is one of the most commonly used questionnaire to assess QoL, and evaluates the vision-related health status of individuals, in addition to the impact of ocular diseases on patients’ social functions, emotional well-being and daily routine activities(18). Keratoconus is one of the most common ocular diseases which may negatively affect QoL due to its prevalence among young adults in their active years.
Using the NEI-VFQ, similar vision-specific QoL is observed among keratoconus cases as that observed in the elder cases of age-related eye disease study (AREDS) with categories 3 and 4 macular degeneration(19).
A prospective study called Collaborative Longitudinal Evaluation of Keratoconus (CLEK), conducted among 925 keratoconus patients during a 7-year follow-up period, evaluated changes that occurred in the vision-related quality of life (V-QoL). This study reported a decrease in all scales except ocular pain and mental health. Particularly, a 10-letter decrease in high-contrast binocular visual acuity and 3.00 D increase in steep keratometry were associated with significantly larger decreases in V-QoL of the patients. The CLEK study reported that the clinical indicators having the strongest association with lower V-QoL at baseline were visual acuity worse than 20/40 and corneal curvature ≥52 D(20). Aydin Kurna et al. detected that the overall scores of the NEI-VFQ-25 were lower in the keratoconus patients. The difference was reported to be more prominent in the subscales of general vision, ocular pain, near vision, vision-specific mental health, vision-specific role difficulties, and peripheral vision (p<0.05). Vision-related QoL was reported to be worse in keratoconus patients. It was suggested that success in contact lens usage and maintaining higher visual acuity may improve vision related QoL(21).
In the present study we detected a positive correlation between CS and near activities and peripheral vision and a negative correlation between logMAR CDVA with ScCL and distance activities, near activities, and visionspecific social functioning in the NEI-VFQ subgroups.
Picot et al. studied the overall scores of patients-fitted with scleral lenses or not-on the NEI-VFQ 25 questionnaire and reported that they were significantly higher with the use of scleral lenses than without scleral lenses, with overall scores of 80.2/100 and 48.1/100, respectively (p<0.0001). The overall score was found to increase with ScCL usage by an average of 32.1 ± 4.6 points (28, 82) (p<0.0001)(16). In our study we observed that the overall NEI-VFQ 25 score was 52.33/100 before treatment versus 75.63/100 after 3 months of ScCL use. The overall score increased by an average of 22.30/100. The overall scores of patients with contact lens treatment were observed to be significantly higher than those of patients with uncorrected vision (p=0.02).
ScCLs can be applied successfully in irregular corneas with insufficient visual acuity increase under conventional treatment. Since they have a positive impact in increasing QoL, they must be considered as an effective therapeutic option in cases of moderate/severe keratoconus, PMD and PKA patients. QoL in our patients was positively affected by increased visual acuity and contrast sensitivity.
REFERENCES
1. Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol. 1984; 28(4):293-322.
2. Rathi VM, Mandathara PS, Dumpati S. Contact lens in keratoconus. Indian J Ophthalmol. 2013;61(8):410-5.
3. Schornack MM. Scleral lenses: a literature review. Eye Contact Lens. 2015;41(1):3-11.
4. Van der Worp E, Bornman D, Ferreira DL, Faria-Ribeiro M, Garcia-Porta N, Gonzalez-Meijome JM. Modern scleral contact lenses: a review. Cont Lens Anterior Eye. 2014;37(4):240-50. Comment in: Cont Lens Anterior Eye. 2015;38(1):73-4.
5. Toprak B, Eser E, Guler C. Cross-validation of the Turkish Version of the 25-Item National Eye Institute Visual Functioning Questionnaire (NEI-VFQ 25). Ophthalmic Epidemiol. 2005;12(4):259-69.
6. Pullum KW, Whiting MA, Buckley RJ. Scleral contact lenses: the expanding role. Cornea. 2005;24(3):269-77.
7. Cotter JM, Rosenthal P. Scleral contact lenses. J Am Optom Assoc. 1998;69(1):33-40.
8. Jacobs DS. Updated on scleral lenses. Curr Opin Ophthalmol. 2006; 19(4):298-301.
9. Vreugdenhil W, Geerards AJ, Vervaet CJ. A new rigid gas-permeable semi-scleral contact lens for treatment of corneal surface disorders. Cont Lens Anterior Eye. 1998;21(3):85-8.
10. Alipour F, Behrouz MJ, Samet B. Mini-scleral lenses in the visual rehabilitation of patients after penetrating keratoplasty and deep anterior lamellar keratoplasty. Contact Lens Anterior Eye. 2015; 38(1):54-8.
11. Pullum KW, Buckley RJ. A study of 530 patients referred for rigid gas permeable scleral contact lens assessment. Cornea. 1997;16(6): 612-22.
12. Tan DT, Pullum KW, Buckley RJ. Medical applications of scleral contact lenses: 2. Gas permeable scleral contact lenses. Cornea. 1995;14(2):130-7.
13. Segal O, Barkana Y, Hourovitz D, Behrman S, Kamun Y, Avni I, et al. Scleral contact lenses may help where other modalities fail. Cornea. 2003;22(4):308-10.
14. Rocha GA, Miziara PO, Castro AC, Rocha AA.Visual rehabilitation using mini-scleral contact lenses after penetrating keratoplasty. Arq Bras Oftalmol. 2017;80(1):17-20.
15. Severinsky B, Behrman S, Frucht-Pery J, Solomon A. Scleral contact lenses for visual rehabilitation after penetrating keratoplasty: long term outcomes. Cont Lens Anterior Eye. 2014;37(3):196-202.
16. Picot C, Gauthier AS, Campolmi N, Delbosc B. [Quality of life in patients wearing scleral lenses]. J Fr Ophtalmol. 2015;38(7):615-9. French.
17. Sabesan R, Johns L, Tomashevskaya O, Jacobs DS, Rosenthal P, Yoon G. Wavefront-guided scleral lens prosthetic device for keratoconus. Optom Vis Sci. 2013;90(4):314-23.
18. Mangione CM, Lee PP, Pitts J, Gutierrez P, Berry S, Hays RD. Psychometric properties of the National Eye Institute Visual Function Questionnaire (NEI-VFQ). NEI-VFQ Field Test Investigators. Arch Ophthalmol. 1998;116(11):1496-504.
19. Kymes SM, Walline JJ, Zadnik K, Gordon MO; Collaborative Longitudinal Evaluation of Keratoconus study group. Quality of life in keratoconus. Am J Ophthalmol. 2004;138(4):527-35. Comment in: Am J Ophthalmol. 2004;138(4):637-8.
20. Kymes SM, QWalline JJ, Zadnik K, Sterling J, Gordon MO; Collaborative Longitudinal Evaluation of Keratoconus Study Group. Changes in the quality of life of people with keratoconus. Am J Ophthalmol. 2008;145(4):611-7.
21. Aydin Kurna S, Altun A, Gencaga T, Akkaya S, Sengor T. Vision related quality of life in patients with keratoconus. J Ophthalmol. 2014;2014:694542.
Submitted for publication:
October 20, 2017.
Accepted for publication:
March 13, 2018.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Approved by the following research ethics committee: Ankara Numune Education and Research Hospital (# E-15-673)