

Newton Kara-Junior1; Camila Ribeiro Koch1; Marcony Rodrigues de Santhiago1,2; Luciana Fornari3; Bruno Caramelli3
DOI: 10.5935/0004-2749.20180069
ABSTRACT
Patients undergoing cataract surgery are generally elderly, and many take drugs with systemic effects. The surgeon must be aware of the risks of continuing or discontinuing such medications perioperatively. Antiplatelet drugs and anticoagulants, prescribed to reduce the incidence of thromboembolic events, are often used in this population. This paper aims to review the perioperative use of antiplatelet and anticoagulant drugs in the setting of cataract surgery. Topical or intracameral anesthesia is preferred over anesthesia injected with needles. Aspirin can be safely continued in patients undergoing cataract surgery. Warfarin has been extensively studied, and the risk of hemorrhage associated with cataract surgery is low if the international normalized ratio is in the therapeutic range. Only a few studies of direct oral anticoagulants are available, and therefore no definite recommendations regarding those agents can be made at this time. Anesthesia in cataract surgery carries a low risk, even for patients taking anticoagulant or antiplatelet drugs. The discontinuation of this class of drugs before cataract surgery may increase the risk of thromboembolism.
Keywords: Anticoagulants; Platelet aggregation inhibitors; Cataract extraction; Risk factors
RESUMO
Os pacientes submetidos à cirurgia de catarata são geralmente idosos e muitos deles usam drogas com efeitos sistêmicos. No entanto, o cirurgião deve estar ciente dos riscos em manter ou descontinuar medicamentos sistêmicos no pré-operatório da cirurgia de catarata, como os anticoagulantes e os antiplaquetários. Este artigo tem como objetivo revisar a classe de drogas antiplaquetárias e anticoagulantes e orientar o cirurgião de catarata. A classe de fármacos anticoagulantes e antiplaquetária reduz a incidência de eventos potencialmente tromboembólicos. A anestesia tópica ou intracameral nesses pacientes deve ser preferida em relação à anestesia com agulhas. Aspirina pode ser mantida com segurança nos pacientes submetidos à cirurgia de catarata. A varfarina foi amplamente estudada e os riscos na cirurgia de catarata são baixos, no entanto, o INR deve ser controlado. Mais estudos são necessários com anticoagulantes orais diretos. Anestesia na cirurgia de catarata tem baixo risco de complicações, mesmo em uso de anticoagulantes ou antiplaquetários sistêmicos. A descontinuação desta classe de medicamentos no pré-operatório da cirurgia de catarata pode aumentar os riscos sistêmicos tromboembólicos.
Descritores: Anticoagulantes; Inibidores da agregação de plaquetas; Extração de catarata; Fatores de risco
INTRODUCTION
According to the World Health Organization, cataract surgery is the most frequently performed surgical procedure in the world(1,2). The population of people over 65 years of age is expected to double in the next decade, many of whom would benefit from cataract surgery. However, a large proportion of these individuals also have age-related comorbidities, for which they take drugs with various systemic effects(3). The cataract surgeon must consider the risk of perioperative complications posed by some of these agents(4), requiring awareness of the various classes of drugs that are usually prescribed for this age group(5).
Antiplatelet agents (Ap) and anticoagulants (Ac) are used to minimize the risk of thromboembolic events in patients with coronary heart disease (e.g., with intracoronary stents requiring the use of two Ap drugs for some period of time) or other cardiovascular diseases, such as atrial fibrillation(6,7). While the discontinuation of antithrombotic treatment in order to minimize the risk of bleeding during cataract surgery might be considered routine by some, it is potentially harmful for patients who are at an increased risk of thrombosis(8).
This paper aims to review and update knowledge about Ac/Ap agents and their management during cataract surgery. We conducted a systematic literature review using the online database Medical Literature Analysis and Retrieval System Online (MEDLINE) and Cochrane Library databases from 1994 to 2017 for Ac/Ap agents. The references were selected by the classes of Ac/Ap drugs most used in medical practice and their risks in cataract surgery.
1. Indications for Ac/Ap drugs
The main indications for these drugs are in the management or prevention of thromboembolic events in disorders such as stroke, acute myocardial infarction, angina, cardiac surgery, prosthetic heart valves, acute coronary syndrome, pulmonary embolism, venous thromboembolism, and atrial fibrillation(9-11). According to current guidelines, some form of antithrombotic treatment is indicated in 70% to 80% of patients with atrial fibrillation and in 20% to 30% of patients with coronary artery disease(12).
2. Classification and mechanism of action of Ac/Ap drugs
2.1 Anticoagulant drugs
The drugs most frequently given parenterally are unfractionated heparin and low molecular weight heparin (LMWH) (e.g., enoxaparin, dalteparin), and the most frequently used oral agent is warfarin. Newer agents, the direct oral anticoagulants (DOAC), are increasingly prescribed. Figure 1 shows the classification, target, and half-life of Ac drugs.
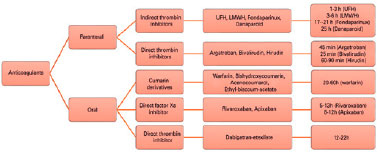
The DOAC class includes drugs that directly inhibit activated coagulation factors. Dabigatran inhibits factor IIa (thrombin), and apixaban and rivaroxaban inhibit factor Xa(13-15). These drugs were developed as alternatives to heparin and warfarin for the treatment of arterial and venous thromboembolic diseases. The advantages are a fixed dose, no need for routine monitoring of the prothrombin time, and a lower risk of bleeding. The average peak period of anticoagulation provided by DOACs ranges between 1 and 4 hours, a much shorter time range than warfarin(16).
Although the use of warfarin has several drawbacks, including a narrow therapeutic range and interaction with other drugs, it is still widely used because of its low cost. It is an oral vitamin K antagonist, but it acts on both vitamin K-dependent and -independent coagulation factors, affecting factors II, VII, IX, X, and proteins C and S(12,13). It takes several days for these factors to be synthesized after interruption of warfarin, predisposing to hemorrhagic complications even after discontinuation of the drug(14). Conversely, interruption of warfarin preoperatively may lead to a hypercoagulable state related to differential recovery of factors that had been inhibited by the drug(12). It is thought that proteins C and S recover more slowly than other vitamin K-dependent coagulation factors, causing a temporary imbalance between coagulation and anticoagulation(6,10).
The other route of administration of Ac agents is parenteral. Unfractioned heparin inactivates thrombin (factor II) and factors Xa, IXa, XIa, and XIIa(17). LMWH has a more predictable pharmacokinetic profile than standard heparin and has an increased affinity for factor Xa relative to thrombin. Fondaparinux inhibits factor Xa but has no effect on thrombin formation because it selectively binds to antithrombin(6). The direct thrombin inhibitors exert their effect by directly and selectively binding to the active site of factor IIa(15).
2.2 Antiplatelet drugs
The antiplatelet agents used most often are aspirin and clopidrogrel. They interfere with platelet function and are therefore prophylactic against thrombosis. They are the first-line of antithrombotic therapy to treat and prevent acute ischemic syndromes(9,12). Figure 2 shows the classification, target, and half-life of Ap drugs.
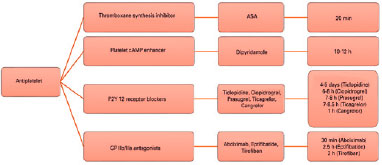
Aspirin irreversibly inhibits cyclooxygenase 1, thereby blocking formation of thromboxane A2, an effect that persists for 5 to 7 days. Clopidrogrel acts as an adenosine diphosphate receptor antagonist and is a prodrug. It is activated by binding irreversibly to the P2Y12 receptor, leading to permanent inhibition of bound platelets. Prasugel and ticagrelor were developed to inhibit platelet aggregation more consistently and rapidly than clopidogrel. Ticagrelor, which is not a prodrug, binds directly and reversibly to the P2Y12 receptor(9,18). Glycoprotein IIb/IIIa receptor antagonists are another class that bind to these receptors, reducing platelet aggregation. They are given intravenously or by direct intracoronary infusion during percutaneous coronary intervention(6).
3. Ac/Ap agents and cataract surgery
Even though cataract surgery itself is considered to be a low risk procedure, the majority of patients for whom it is indicated have a moderate degree of surgical risk according to the American Society of Anesthesiologists A classification and other risk scores(19,20). The use of Ac/Ap agents may increase the risk of hemorrhage or other complications in other types of surgery. However, the risk of bleeding must be balanced against the danger of thromboembolic events if the medications are discontinued.
3.1 Risk of anesthesia in cataract surgery
Cataract surgery can be performed under general anesthesia or with sedation and local or topical anesthesia. Under topical anesthesia, additional intracameral anesthesia with lidocaine can be administered intraoperatively(22). Local anesthesia includes peribulbar or retrobulbar blocks and sub-Tenon anesthesia(23). Among the options, topical anesthesia is preferred by most surgeons(21).
Benzimra et al.(8) reported on 48,862 patients in a national dataset, assessing complications in the 28.1% who were taking Ac/Ap drugs. With sub-Tenon anesthesia, there were no potentially sight-threatening complications and no cases of retrobulbar hemorrhage. However, those taking clopidogrel or warfarin had an increase in minor complications due to the use of a sharp needle. These results were consistent with the findings of Kumar et al.(24). Kobayashi et al. showed that patients taking warfarin, aspirin, or both had a higher incidence of subconjunctival hemorrhage with sub-Tenon anesthesia than patients who discontinued therapy had(25). They stated that the risk of bleeding depends on the anesthetic technique, a risk that persists even if the antithrombotic medication is interrupted. There is evidence of an increased risk of orbital hemorrhage (0.2% to 1.0%) when local anesthesia is performed using needles(26). Davis et al.(27) observed low rates of retrobulbar hemorrhage in 16,224 anesthetic blocks, an incidence of 0.07% with a peribulbar block versus 0.44% with a retrobulbar block.
Some studies have shown that cataract surgery can be performed with local anesthesia without complications even with continued oral Ac therapy in the therapeutic range as indicated by the international normalized ratio (INR)(3,28). Katz et al.(29) studied more than 19,000 patients who underwent senile cataract surgery. Their results were consistent with those noted above, indicating that medical and ophthalmic adverse events were low in cataract surgery. They recommended not suspending Ac/Ap agents preoperatively because of the increased risk of antithrombotic events for which these medications had been prescribed in the first place. As yet, there are only a few studies analyzing the risk of complications in cataract surgery in patients taking DOACs(13,14,30). The majority of available data is from patients taking warfarin.
To evaluate the safety of continuing warfarin therapy during cataract surgery with topical anesthesia, Kara-Junior et al.(31) prospectively compared 60 eyes, 30 in patients taking warfarin and 30 in individuals not on an Ac in the Clinic Hospital, Universidade de São Paulo Medical School. An INR between 1.9 and 2.7 was an inclusion criterion for those on warfarin to ensure that the medication was in the therapeutic range. The authors did not observe any perioperative intracameral bleeding, and there were no postoperative complications in either group. After one month, 90% of the patients had a corrected visual acuity of 20/40 or better. These results are consistent with those of other investigators(21,32) and support the concept that continuing warfarin in patients undergoing cataract surgery with topical anesthesia does not have a significant increase in vision-threatening bleeding.
3.2 Systemic risks
Two studies with a large number of patients undergoing cataract surgery showed that more than 28% of patients were using aspirin and 5.1% were on warfarin(8,29). There is little data on cataract surgery in patients taking double antiplatelet therapy(24,33). If these drugs were to be discontinued perioperatively, it is important to understand the systemic risks.
The efficacy of warfarin has been consistent across studies in decreasing the risk of stroke in patients with atrial fibrillation. A review indicated an absolute reduction in annual stroke incidence from 4.5% in control patients to 1.4% in patients assigned to adjusted-dose warfarin; interrupting the anticoagulation increases the risk of stroke(34). In patients treated with Ap agents for nonrheumatic atrial fibrillation, cerebrovascular disease, or artificial cardiac valves, the suspension of those agents is associated with even higher risks of thromboembolic complications(12,35). In patients undergoing coronary artery bypass surgery and other nonophthalmologic procedures, clopidogrel has been shown to increase the risk of postoperative hemorrhage(36,37). Regarding warfarin, the Royal College of Ophthalmologists(26) advised on being aware of the drug’s effectiveness in reducing death caused by thromboembolic events and that suspending it increases the risk of such events.
4. Recommendations to cataract surgeons
The 2004 guidelines from the Royal College of Ophthalmologists in the United Kingdom recommended maintaining anticoagulation in patients undergoing cataract surgery(26). The American Academy of Ophthalmology has similar recommendations. They advise continuation of warfarin in patients undergoing cataract surgery, provided that the INR is in the therapeutic range (I+ evidence, good quality, strong recommendation) and that aspirin should be discontinued perioperatively only if the risk of bleeding outweighs the drug’s potential benefit (I- evidence, good quality, strong recommendation)(38). Table 1 shows current recommendations for cataract surgery in patients taking Ac/Ap drugs.
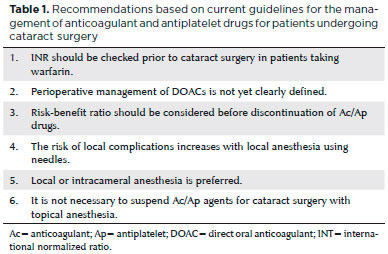
Preoperatively, patients must be informed about the risks of continuing Ac/Ap agents, thereby risking orbital bleeding, or of discontinuing the drugs, which increases the risk of thromboembolic events(25,39). It is recommended that these issues be included in the surgical consent form(40). Self-administered health questionnaires can help patients remember the medications they are using as well as comorbidities, supplementing the ophthalmologists’ records. Furthermore, it is well to remember that drug metabolism may be slower in older patients(33,41).
Anesthesia for patients taking Ac/Ap agents requires careful consideration. Retrobulbar (intraconal) or peribulbar (extraconal) anesthesia is not recommended because of a slightly higher risk of orbital hemorrhage(23). Sub-Tenon or topical anesthesia is generally preferred(24). With topical or intracameral anesthesia, there is no indication for suspension of Ac/Ap medications. However, with sub-Tenon anesthesia, the use of less sharp needles is recommended when performing local cauterization to reduce the incidence or extension of subconjunctival hemorrhage(29).
INR is used to monitor the anticoagulant effect of warfarin at intervals appropriate for each patient(42). Assuming that it has been decided to continue warfarin when a patient has cataract surgery, it is vital to ensure that the INR remains in the therapeutic range to avoid inadequate anticoagulation, increasing the risk of thromboembolic events or too much anticoagulation, with the attendant higher risk of bleeding(12,20). Warfarin does not need to be discontinued if the INR is in the 2 to 3 range. However, if the INR is 3 to 4, the patient’s attending physician and cataract surgeon should discuss the best approach together. Since the half-life of vitamin K antagonists is variable, if warfarin is going to be discontinued, it is usually recommended to be stopped at least five days before surgery. This may, however, increase the risk of thromboembolic events depending on when the anticoagulant effect dissipates. That is why such a decision must be made very carefully in consultation with the attending physician and the patient, so that the risk/benefit ratio is understood. Data from other types of surgery in patients on clopidogrel, which irreversibly blocks activation of platelets to which it is bound, suggests that it, too, should be discontinued five days before surgery if the decision to interrupt treatment has been taken(20,43).
For patients taking DOACs, preoperative management of the medication is more convenient. The duration of the effect can be as short as 24 hours depending on renal function, and blood-test monitoring is unnecessary(13).
A recent guideline(44) from the Brazilian Society of Cardiology suggests that, while warfarin therapy should be continued in patients undergoing cataract surgery as long as the INR is within the therapeutic range, there is insufficient evidence on how to manage DOACs in this setting. They recommend consultation between the surgeon and the attending physician to reach a consensus. If the decision is to suspend the DOAC, it should be discontinued at least 24 hours before surgery, depending on the patient’s renal function. For patients on Ap agents for secondary prevention of coronary heart disease, aspirin or clopidogrel should be maintained during cataract surgery. Patients who have undergone coronary angioplasty require double Ap therapy for a defined period of time depending on the type of stent, in order to avoid stent thrombosis. If cataract surgery cannot be postponed during that period, the guidelines indicate that double Ap therapy should not be stopped.
Ophthalmic bleeding events associated with cataract surgery generally have few or no serious consequences, even if Ac/Ap medications are continued perioperatively. Discontinuation of these drugs may increase morbidity or mortality due to potentially serious thromboembolic events. Topical anesthesia is preferred for patients taking these medications. If it appears that Ac/Ap agents should be discontinued preoperatively, close consultation between the surgeon and the patient’s attending physician is mandatory in order to try to limit the risks associated with this course of action.
REFERENCES
1. World Health Organization. A framework and indicators for monitoring VISION 2020-The Right to Sight. Report of a WHO Working Group. Geneva: WHO;2002.
2. Caligaris LS, Medina NH, Lansingh VC, Waldman EA, Yaacov-Pena F. Analyses of cataract surgery performed by the Unified Health System in Brazil, 2006-2007. Rev Panam Salud Publica. 2011;29(6):428-32.
3. Grzybowski A, Ascaso FJ, Kupidura-Majewski K, Packer M. Continuation of anticoagulant and antiplatelet therapy during phacoemulsification cataract surgery. Curr Opin Ophthalmol. 2015; 26(1):28-33.
4. Lira RP, Nascimento MA, Kara-Jose N, Arieta CE. [Predictive value of preoperative tests in facectomy]. Rev Saude Publica. 2003; 37(2):197-202. Portuguese.
5. Michalska-Malecka K, Nowak M, Gosciniewicz P, Karpe J, Slowinska- Lozynska L, Lypaczewska A, et al. Results of cataract surgery in the very elderly population. Clin Interv Aging. 2013;8:1041-6.
6. Lorga Filho AM, Azmus AD, Soeiro AM, Quadros AS, Avezum A, Jr., Marques AC, et al. Brazilian guidelines on platelet antiaggregants and anticoagulants in cardiology. Arq Bras Cardiol. 2013;101(3 Suppl 3):1-95.
7. Jafri SM. Periprocedural thromboprophylaxis in patients receiving chronic anticoagulation therapy. Am Heart J. 2004;147(1):3-15.
8. Benzimra JD, Johnston RL, Jaycock P, Galloway PH, Lambert G, Chung AK, et al. The Cataract National Dataset electronic multicentre audit of 55,567 operations: antiplatelet and anticoagulant medications. Eye (Lond). 2009;23(1):10-6.
9. Patrono C, Morais J, Baigent C, Collet JP, Fitzgerald D, Halvorsen S, et al. Antiplatelet agents for the treatment and prevention of coronary atherothrombosis. J Am Coll Cardiol. 2017;70(14):1760-76.
10. Lip GY, Windecker S, Huber K, Kirchhof P, Marin F, Ten Berg JM, et al. Management of antithrombotic therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous coronary or valve interventions: a joint consensus document of the European Society of Cardiology Working Group on Thrombosis, European Heart Rhythm Association (EHRA), European Association of Percutaneous Cardiovascular Interventions (EAPCI) and European Association of Acute Cardiac Care (ACCA) endorsed by the Heart Rhythm Society (HRS) and Asia-Pacific Heart Rhythm Society (APHRS). Eur Heart J. 2014;35(45):3155-79.
11. Bartholomay E, Polli I, Borges AP, Kalil C, Arroque A, Kohler I, et al. Prevalence of oral anticoagulation in atrial fibrillation. Clinics (Sao Paulo). 2014;69(9):615-20.
12. Lip GY, Huber K, Andreotti F, Arnesen H, Airaksinen JK, Cuisset T, et al. Antithrombotic management of atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing coronary stenting: executive summary--a Consensus Document of the European Society of Cardiology Working Group on Thrombosis, endorsed by the European Heart Rhythm Association (EHRA) and the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2010;31(11):1311-8.
13. Blum RA, Lindfield D. Direct oral anticoagulant drugs (DOAC). J Cataract Refract Surg. 2016;42(1):171-2.
14. Christos S, Naples R. Anticoagulation reversal and treatment strategies in major bleeding: Update 2016. West J Emerg Med. 2016; 17(3):264-70.
15. Mancl EE, Crawford AN, Voils SA. Contemporary anticoagulation reversal focus on direct thrombin inhibitors and factor Xa inhibitors. J Pharm Pract. 2013;26(1):43-51.
16. Faraoni D, Levy JH, Albaladejo P, Samama CM, Groupe d’Intérêt en Hémostase Périopératoire. Updates in the perioperative and emergency management of non-vitamin K antagonist oral anticoagulants. Crit Care. 2015;19:203.
17. Garcia DA, Baglin TP, Weitz JI, Samama MM. Parenteral anticoagulants: A ntithrombotic therapy and prevention of thrombosis. 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e24S-e43S.
18. Born G, Patrono C. Antiplatelet drugs. Br J Pharmacol. 2006;147 Suppl 1:S241-51.
19. Pinho C, Grandini PC, Gualandro DM, Calderaro D, Monachini M, Caramelli B. Multicenter study of perioperative evaluation for noncardiac surgeries in Brazil (EMAPO). Clinics (Sao Paulo). 2007; 62(1):17-22.
20. Payal AR, Sola-Del Valle D, Gonzalez-Gonzalez LA, Cakiner-Egilmez T, Chomsky AS, Vollman DE, et al. American Society of Anesthesiologists classification in cataract surgery: Results from the Ophthalmic Surgery Outcomes Data Project. J Cataract Refract Surg. 2016;42(7):972-82.
21. Hosoda Y, Kuriyama S, Jingami Y, Hattori H, Hayashi H, Matsumoto M. A comparison of patient pain and visual outcome using topical anesthesia versus regional anesthesia during cataract surgery. Clin Ophthalmol. 2016;10:1139-44.
22. Ezra DG, Allan BD. Topical anaesthesia alone versus topical anaesthesia with intracameral lidocaine for phacoemulsification. Cochrane Database Syst Rev. 2007(3):CD005276.
23. Alhassan MB, Kyari F, Ejere HO. Peribulbar versus retrobulbar anaesthesia for cataract surgery. Cochrane Database Syst Rev. 2015(7):Cd004083.
24. Kumar N, Jivan S, Thomas P, McLure H. Sub-tenon’s anesthesia with aspirin, warfarin, and clopidogrel. J Cataract Refract Surg. 2006; 32(6):1022-5.
25. Kobayashi H. Evaluation of the need to discontinue antiplatelet and anticoagulant medications before cataract surgery. J Cataract Refract Surg. 2010;36(7):1115-9.
26. The Royal College of Ophthalmologists. Cataract surgery guidelines [Internet]. London, UK: Royal College of Ophthalmologists, 2004; [updated 2010; cited 2018 Jan 20]. Available from: http://www.rcophth.ac.uk/docs/publication/published/FinalVersionGuidelines.
27. Davis DB, 2nd, Mandel MR. Efficacy and complication rate of 16,224 consecutive peribulbar blocks. A prospective multicenter study. J Cataract Refract Surg. 1994;20(3):327-37.
28. Assia EI, Raskin T, Kaiserman I, Rotenstreich Y, Segev F. Effect of aspirin intake on bleeding during cataract surgery. J Cataract Refract Surg. 1998;24(9):1243-6.
29. Katz J, Feldman MA, Bass EB, Lubomski LH, Tielsch JM, Petty BG, et al. Risks and benefits of anticoagulant and antiplatelet medication use before cataract surgery. Ophthalmology. 2003;110(9):1784-8.
30. Jun M, Lix LM, Durand M, Dahl M, Paterson JM, Dormuth CR, et al. Comparative safety of direct oral anticoagulants and warfarin in venous thromboembolism: multicentre, population based, observational study. BMJ. 2017;359:j4323.
31. Kara-Junior N, Santhiago MR, Almeida HG, Raiza AC. Safety of warfarin therapy during cataract surgery under topical anesthesia. Arq Bras Oftalmol. 2015;78(3):173-4.
32. Carter K, Miller KM. Phacoemulsification and lens implantation in patients treated with aspirin or warfarin. J Cataract Refract Surg. 1998;24(10):1361-4.
33. Davies BR. Combined aspirin and clopidogrel in cataract surgical patients: a new risk factor for ocular haemorrhage? Br J Ophthalmol. 2004;88(9):1226-7.
34. Di Legge S, Koch G, Diomedi M, Stanzione P, Sallustio F. Stroke prevention: managing modifiable risk factors. Stroke Res Treat. 2012; 2012:391538.
35. Kong KL, Khan J. Ophthalmic patients on antithrombotic drugs: a review and guide to perioperative management. Br J Ophthalmol. 2015;99(8):1025-30.
36. Leong JY, Baker RA, Shah PJ, Cherian VK, Knight JL. Clopidogrel and bleeding after coronary artery bypass graft surgery. Ann Thorac Surg. 2005;80(3):928-33.
37. Ernst A, Eberhardt R, Wahidi M, Becker HD, Herth FJ. Effect of routine clopidogrel use on bleeding complications after transbronchial biopsy in humans. Chest. 2006;129(3):734-7.
38. Olson RJ, Braga-Mele R, Chen SH, Miller KM, Pineda R, Tweeten JP, et al. Cataract in the adult eye Preferred Practice Pattern®. Ophthalmology. 2017;124(2):P1-P119.
39. Konstantatos A. Anticoagulation and cataract surgery: a review of the current literature. Anaesth Intensive Care. 2001;29(1):11-8.
40. Zhang Y, Ruan X, Tang H, Yang W, Xian Z, Lu M. Video-assisted informed consent for cataract surgery: a randomized controlled trial. J Ophthalmol. 2017;2017:9593631.
41. Keay L, Lindsley K, Tielsch J, Katz J, Schein O. Routine preoperative medical testing for cataract surgery. Cochrane Database Syst Rev. 2012(3):Cd007293.
42. Grzybowski A, Packer M. Anticoagulant and antiplatelet therapy during ocular surgery. Br J Ophthalmol. 2014;98(8):1137-8.
43. Kiire CA, Mukherjee R, Ruparelia N, Keeling D, Prendergast B, Norris JH. Managing antiplatelet and anticoagulant drugs in patients undergoing elective ophthalmic surgery. Br J Ophthalmol. 2014;98(10):1320-4.
44. Gualandro DM YP, Caramelli B, Marques AC, Calderaro D, Luciana S. Fornari LS et al. 3ª Diretriz de Avaliação Cardiovascular Perioperatória da Sociedade Brasileira de Cardiologia. Arq Bras Cardiol. 2017;109(3Supl.1):1-104.
Submitted for publication:
August 24, 2017.
Accepted for publication:
November 23, 2017.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose