

Vinicius Coral Ghanem; Marilia Lordello Passos; André Luís Piccinini; Ramon Coral Ghanem
DOI: 10.5935/0004-2749.20180068
ABSTRACT
The following report describes a case of apical leucoma syndrome after hyperopic photorefractive keratectomy following hyperopic laser in situ keratomileusis and the subsequent treatment of this complication with focal phototherapeutic keratectomy. The patient underwent focal transepithelial phototherapeutic keratectomy of 70 µm ablation and 1.5 mm diameter after pupil and ablation offset correction. After 1 year, significant improvement in vision was observed and only slight residual opacity remained on biomicroscopy and optical coherence tomography. Focal phototherapeutic keratectomy was effective and safe for the treatment of this complication.
Keywords: Hyperopia/therapy; Keratomileusis, laser in situ; Corneal surgery, laser; Photorefractive keratectomy
RESUMO
O relato a seguir descreve um caso da síndrome do Leucoma Apical após cirurgia ceratorrefrativa hipermetrópica depois de Laser hiperópico in situ keratomileusis, e o subsequente tratamento desta complicação com ceratectomia fototerapêutica focal. O paciente foi submetido à ceratectomia fototerapêutica focal transepitelial com ablação de 70 µm e diâmetro de 1,5 mm, após correção de offset pupilar. Depois de um ano, foi observada uma melhora significativa da acuidade visual permanecendo apenas leve opacidade residual na biomicroscopia e tomografia de coerência óptica. A ceratectomia fototerapêutica focal foi efetiva e segura para o tratamento desta complicação.
Descritores: Hiperopia/terapia; Ceratomileuse assistida por excimer laser in situ; Cirurgia da córnea a laser; Ceratectomia fotorrefrativa
INTRODUCTION
Hyperopic laser-assisted in situ keratomileusis (H-LASIK) is a safe and effective treatment for correction of hyperopia(1). Although uncommon, complications after H-LASIK tend to be associated with epithelial ingrowth, dry eyes, and high-order aberrations, especially coma and spherical aberrations(1-4). It is expected that treatments, which result in high final keratometry, especially above 50 D, can cause apical scarring(5). Sener et al.(6) described apical nodular subepithelial corneal scarring as a complication of hyperopic photorefractive keratectomy (PRK) retreatment.
To the best of our knowledge, this is the first report of focal phototherapeutic keratectomy (PTK) for treatment of apical nodular subepithelial scarring after hyperopic PRK following H-LASIK.
CASE REPORT
A 50-year-old Caucasian woman with +3.00 D of hyperopia (oculus uterque) underwent monovision LASIK in November 2007 with a Schwind Esiris excimer laser. Five years and 10 months after surgery, the patient returned to the hospital, complaining of poor near uncorrected visual acuity of 20/30 <J6 OD (oculus dextrus) and 20/20 J6 OS (oculus sinister). Corrected distance visual acuity (CDVA) of both eyes was 20/20 (+2.00 OD and +0.25 OS). On examination, the flap diameter was approximately 8.0 mm. Topography of OD showed apical keratometry regression of 1.7 D, but the topography pattern was the same as it was in 2008. Apical keratometric OS measurements were exactly the same as in February 2008 (Figure 1). The thinnest point of the cornea of OD was 500 µm.
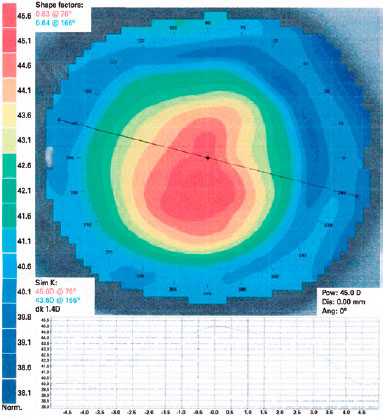
To obtain a larger ablation zone, hyperopic aberration-free PRK on OD was performed in September 2013. The epithelium was removed with a blunt spatula, without the use of alcohol. The target was -1.60 D. The optical zone was 6.70 mm, and the total ablation zone was 8.66 mm. Next, Mitomycin C (MMC) 0.02% was applied for 20 s to the ablated area followed by irrigation with 15 mL of balanced saline solution. The Schwind Amaris estimated keratometry after PRK was 45.65 D 158°/46.35 D 68° and apical keratometry of 47.5 D.
Five days later, the cornea epithelium had healed and the therapeutic contact lens (TCL) was removed. One month after PRK, the patient returned with intense epithelial hyperplasia of 3.5 mm and a slight stromal haze in the visual axis, without signs of inflammation or infection. Best corrected visual acuity was 20/400. It was decided to remove the epithelium in the central 4 mm, and a TCL was fitted (ACUVUE, Johnson & Johnson, São José dos Campos, SP, Brazil). Gatifloxacin 0.3% with prednisolone acetate 1% (Zypred, Allergan, São Paulo, SP, Brazil) was prescribed until TCL removal, 6 days later, when a slight apical epithelial hyperplasia was observed. Fluorometholone acetate 0.1% (Flutinol, Latinofarma, São Paulo, Brazil) was prescribed three times a day for 30 days.
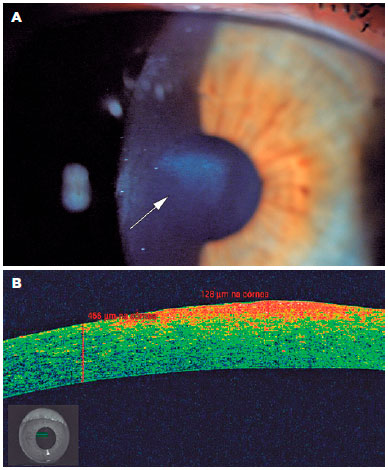
One year and 5 months after PRK, CDVA was 20/200 OD. On examination, a leucoma (diameter of 1.5 mm and depth of 128 µm; Figure 2A and 2B, respectively) was observed on the visual axis, but almost all of the leucoma reached only about 80 µm, as estimated by optical coherence tomography (OCT). The use of a contact lens did not improve vision. The patient was informed of the complications and possible treatment with PTK. She was further informed of an expected secondary hyperopic shift due to flattening of the corneal center.
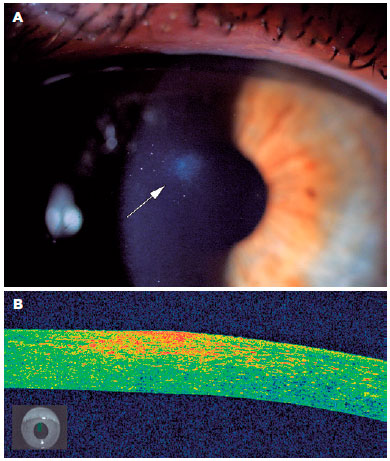
The patient underwent focal transepithelial PTK. After pupil and ablation offset correction, the ablation depth was 70 µm and diameter was 1.5 mm. The pupil offset was measured with a Keratron Scout videokeratoscope (Optikon, Rome, Italy), but it was not possible to calculate ablation offset as the topographical measurements were deemed unreliable. Therefore, ablation offset was based on slit lamp measurements. The pupil diameter was 3.22 mm, radius was 0.10 mm, and angle was 169°. The ablation offset radius was 0.30 mm, and the angle was 105°. The depth of ablation was based on OCT. We opted for 70 µm in order to avoid excessive stromal ablation. MMC 0.02% was applied to the ablated area for 20 s. Postoperative recovery was uneventful. After 1 year, the CDVA was 20/25 (+3.75 -1.0 × 70°). Only a slight residual opacity was observed on biomicroscopy (Figure 3A) and OCT (Figure 3B).
DISCUSSION
Our case highlights an unusual, but important, complication after hyperopic PRK retreatment of apical nodular subepithelial leucoma syndrome. Nevertheless, surface retreatments are considered safe, as the incidence of complications is low(7,8), making it even more difficult to understand the physiopathology of this complication. It must be emphasized that in this case, an apical leucoma developed in the center of the cornea even though this location was not ablated, because hyperopic ablations are performed on the periphery.
Sener et al.(6) described the occurrence of subepithelial apical corneal scarring in 12 eyes of six patients who underwent PRK retreatment for undercorrection after primary hyperopic PRK. Considering that the scarring did not improve even after 40 months of follow-up, it is of utmost importance to have a therapeutic option for these patients.
We might expect this complication to only exist in cases where MMC was not used, such as in the study conducted by Sener et al.(6). However, this complication was observed even with the use of MMC for 20 s, which led us to consider that this complication may not have occurred if MMC was applied for 1 min. In our case, we also observed apical epithelial hypertrophy after 30 days, unlike cases reported where only slight epithelial changes were found.
Torricelli et al.(9) stated that normal regeneration of the epithelial basement membrane (EBM) appears to be a critical factor to predict corneal healing with relative transparency or vision-limiting stromal opacity. Structural and functional abnormalities of the regenerated EBM facilitate prolonged entry of epithelium-derived growth factors into the stroma, which stimulate the development of mature myofibrobasts and, therefore, stromal opacity. Therefore, abnormal EBM healing of the corneal apex might have been the cause for the central corneal opacity found in our patient.
Reinstein et al.(5,10) reported that the hyperopic ablation can induce a more abrupt change in curvature than myopic ablation, consequently leading to increased epithelial compensation. The study showed a doughnut epithelial pattern, similar to patients with keratoconus, characterized by a thin epithelium localized area surrounded by a thickened epithelial ring. The central thinning of the epithelium also flattens the cornea, thus simulating a flatter keratometry than the actual stromal keratometry. We stress the importance of greater care with hyperopic surface treatments, because the actual stromal keratometry is steeper than evaluated by topography. It would be interesting to conduct a study of corneal epithelial thickness in cases that may benefit from surface retreatment after previous hyperopic treatments, in order to avoid retreating corneas with reduced central epithelial thickness.
To the best of our knowledge, this is the first report of a case of apical leucoma syndrome after LASIK retreatment and to propose a treatment for this complication. It is important to emphasize that this approach can be used for focal treatment of corneal opacities without the need for extensive epithelial removal. Because of the very restricted treatment area, recovery is much faster than with conventional PTK, enabling the application of sequential PTKs (with an interval of a few weeks) to treat larger focal lesions. In addition, it is possible to vary the optical treatment zone between the first and subsequent ablations on the basis of the residual lesion diameter.
In brief, hyperopic surface retreatment after PRK or LASIK can cause apical leucoma syndrome. Focal PTK was both effective and safe for treatment of this complication.
REFERENCES
1. Alió JL, El Aswad A, Vega-Estrada A, Javaloy J. Laser in situ keratomileusis for high hyperopia (>5.0 diopters) using optimized aspheric profiles: Efficacy and safety. J Cataract Refract Surg. 2013; 39(4):519-27.
2. Varley GA, Huang D, Rapuano CJ, Schallhorn S, Boxer Wachler BS, Sugar A. LASIK for hyperopia, hyperopic astigmatism, and mixed astigmatism: A report by the American Academy of Ophthalmology. Ophthalmology. 2004;111(8):1604-17.
3. Melki SA, Azar DT. LASIK Complications: etiology, management, and prevention. Surv Ophthalmol. 2001;46(2):95-116.
4. Sridhar MS, Rao SK, Ed F, Vajpayee RB. Complications of Laserin- situ-Keratomileusis. Cur Ophthalmol. 2002;50(4):265-82.
5. Reinstein DZ, Archer TJ, Gobbe M, Ronald H. Silverman A, Coleman DJ. Epihelial thickness after hyperopic lasik: three dimensional display with artemis very high frequency digital ultrasound. J Refract Surg. 2010;26(8):555-64.
6. Sener B, Özdamar A, Aras C. Apical nodular subepithelial corneal scar after retreatment in hyperopic photorefractive keratectomy. J Cataract Refract Surg. 2000;26(3):352-7.
7. Schallhorn SC, Venter JA, Hannan SJ, Hettinger KA, Teenan D. Flap lift and photorefractive keratectomy enhancements after primary laser in situ keratomileusis using a wavefront-guided ablation profile: Refractive and visual outcomes. J Cataract Refract Surg. 2015;41(11):2501-12.
8. Lee BS, Gupta PK, Davis EA, Hardten DR. Outcomes of photorefractive keratectomy enhancement after LASIK. J Refract Surg. 2014;30(8):549-56.
9. Torricelli AAM, Abirami S, Jiahui W, Vivek S, Steven W. The corneal fibrosis response to epithelial-stromal injury. Exp Eye Res. 2017; 142:110-8.
10. Reinstein DZ, Gobbe M, Archer TJ, Silverman RH, Coleman DJ. Epithelial, stromal, and total corneal thickness in keratoconus: three-dimensional display with artemis very-high frequency digital ultrasound. J Refract Surg. 2010;26(4):259-71.
Submitted for publication:
April 26, 2017.
Accepted for publication:
April 10, 2018.
Funding: No specific financial support was received for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose