

Ana L. Basílio; Ana Cabugueira; Bárbara Borges; Rita Flores; Ana Amaro; Ana Magriço
DOI: 10.5935/0004-2749.20180067
ABSTRACT
Chronic lacrimal canaliculitis is a rare infection of the lacrimal system, and can lead to misdiagnosis due to its overlapping presentation to other common entities. The authors report a case of lacrimal canaliculitis with a three-year history of recurrent unilateral red eye and mucopurulent discharge. Here, we describe the clinical course, surgical details, and microbial analysis of canaliculitis infection.
Keywords: Canaliculitis/surgery; Streptococcus constellatus; Antibacterial agents.
RESUMO
A canaliculite lacrimal crónica é uma infecção rara do sistema lacrimal e pode levar a erros de diagnóstico devido à sua apresentação sobreposta a outras entidades comuns. Os autores relatam um caso de canaliculite lacrimal com história de três anos de olho vermelho unilateral recorrente e secreção mucopurulenta. Aqui, descrevemos o curso clínico, os detalhes cirúrgicos e a análise microbiológica da infecção por canaliculite.
Descritores: Canaliculite/cirurgia; Streptococcus constellatus; Antibacterianos
INTRODUCTION
Chronic lacrimal canaliculitis is a rare infection of the lacrimal system, accounting for only 2% of patients with lacrimal disease(1). This infection is typically caused by Actinomyces and less commonly by other organisms such as Staphylococcus and Streptococcus spp(2).
The most frequent patient complaints are red eye and discharge, and the classic presenting signs are mild-to-severe swelling of the canaliculus, spontaneous mucopurulent discharge from the lacrimal punctum, epiphora, and red pouting punctum(3). This infection is usually unilateral and most commonly involves the lower canaliculus(2).
Its similarity to other diseases may lead to misdiagnosis by clinicians; this is particularly important regarding surgical treatment of this condition. Infection of the lacrimal system is associated with dacryoliths or concretions formation, which is related to inefficient use of an isolated medical strategy as a definitive treatment(4).
CASE REPORT
The authors report the case of a previously healthy 43-year-old man who was born in Bangladesh and has been a resident of Portugal for the last 2 years. He presented for an ophthalmological evaluation based on a three-year history of recurrent episodes of unilateral (left) red eye and mucopurulent discharge. During that time, he underwent treatment by other physicians (general clinicians and ophthalmologists), which included multiple rounds of topical antibiotics and steroids, resulting in temporary symptom improvement with inevitable recurrence after a few days or weeks.
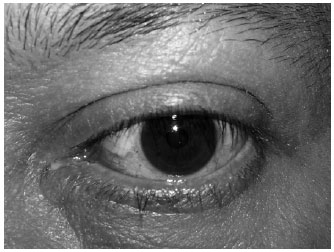
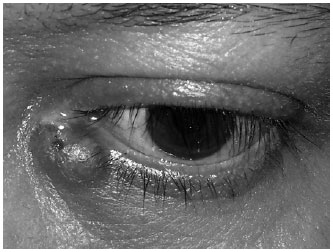
At presentation, a left ocular examination revealed an inferior conjunctival hyperemia combined with mild inferior canalicular swelling, pouting punctum, and mucopurulent discharge from the punctum triggered by palpation over the inferior canaliculus trajectory (Figure 1). Lacrimal system probing and irrigation was normal, and a diagnosis of chronic lacrimal canaliculitis was assumed. Cultural analysis of the mucopurulent discharge revealed cephalosporin-resistant Streptococcus constellatus, and we attempted therapy with ceftazidime irrigation combined with a scheme of ceftazidime fortified drops. The symptoms recurred after two weeks of clinical improvement, and an abscess had formed over the inflamed canaliculus with creation of a skin fistula noted (Figure 2). We performed dacryocystography to exclude the presence of a lacrimal diverticulum and results were normal.
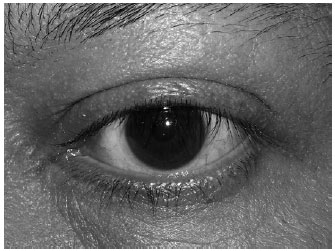
A surgical approach was determined for abscess drainage and removal of dacryoliths under local anesthesia (lidocaine 2% with 1:100,000 epinephrine). We made an incision through the skin and the abscessed area, removing the mucopurulent content and multiple dacryoliths. Sodium chloride 0.9% and hydrogen peroxide solution were used to wash and test lacrimal canaliculus patency. The region was left open and unsutured, and a surgical drain was kept in place for 10 days. The incisional wound healed by second intention without compromising lacrimal drainage. Ciprofloxacin, both topical (0.3% eye drops solution every 6 hours) and systemic (500 mg by mouth every 12 hours) were prescribed for 10 days. The patient was asymptomatic with no inflammatory or infectious signs at one month (Figure 3) and no evidence of recurrence after one year of follow-up.
DISCUSSION
Chronic lacrimal canaliculitis is a chronic inflammation of the canalicular system of the eye that can remain undiagnosed for a long period of time because it is rare and has a variable presentation(2). Patients may present with red eye, purulent discharge, epiphora, or a pouting punctum, and it may be confused with other disorders including chronic conjunctivitis, inflamed chalazion, or dacryocystitis(5-7). The lower canaliculus is most commonly affected area (49.6%-87%)(6-8), which coincides with the location in the present case.
Actinomyces is the most common causative agent of canaliculitis; however, a recent change in the microbiological profile has triggered the emergence of other microorganisms including Streptococcus spp., Staphylococcus spp., Corynebacterium spp., and fungi. Among the Streptococcus spp., S. viridans (24.4%), S. constellatus (6.1%), S. pneumoniae (3.8%), and S. gamma hemolytic (3.8%) are the most common bacterial causes of canaliculus infection(2).
In our patient, the dacryoliths were located within the abscess where they probably developed as a result of tear stasis and inflammation/infection. According to the literature, eye concretions are present in 26%-34.4% of cases(6). Canaliculus infection may lead to dacryolith formation by electrolyte precipitation from a supersaturated solution existing within the canaliculus due to tear stasis and inflammation(9).
A detailed clinical evaluation is sufficient for diagnosing most cases of lacrimal canaliculitis. A correct diagnosis is important because a surgical strategy is commonly needed to treat this clinical entity. Repeated antibiotic irrigation has been suggested as an alternative to surgical intervention for the treatment of chronic canaliculitis(10). However, canaliculotomy with removal of all concretions combined with topical antibiotic therapy remains the gold standard of treatment (2). Wound closure is not necessary, as it usually heals correctly by secondary intention(4), systemic antibiotic treatment may be prescribed.
In conclusion, lacrimal canaliculitis may be diagnosed incorrectly and treated as conjunctivitis, inflamed chalazion, or dacryocystitis with an inevitable recurrence of symptoms. New causative agents for lacrimal canaliculitis are emerging and include Streptococcus and Staphylococcus spp., and surgical removal of all concretions along with topical antibiotic coverage is considered the gold standard for definitive treatment.
REFERENCES
1. Demant E, Hurwitz JJ. Canaliculitis: review of 12 cases. Can J Ophthalmol. 1980;15(2):73-5.
2. Gogandy M, Al-Sheikh O, Chaudhry I. Clinical features and bacteriology of lacrimal canaliculitis in patients presenting to a tertiary eye care center in the Middle East. Saudi J Ophthalmol. 2014; 28(1):31-5.
3. McNab A. Manual of orbital and lacrimal surgery. New York: Churchill Livingstone; 1994. p. 79-80.
4. Fulmer NL, Neal JG, Bussard GM, Edlich RF. Lacrimal canaliculitis. Am J Emerg Med. 1999;17(4):385-6.
5. Vécsei VP, Huber-Spitzy V, Arocker-Mettinger E, Steinkogler FJ. Canaliculitis: difficulties in diagnosis, differential diagnosis and comparison between conservative and surgical treatment. Ophthalmologica. 1994;208(6):314-7.
6. Lin SC, Kao SC, Tsai CC, Cheng CY, Kau HC, Hsu WM, et al. Clinical characteristics and factors associated the outcome of lacrimal canaliculitis. Acta Ophthalmol. 2011;89(8):759-63.
7. Pavilack MA, Frueh BR. Through curettage in the treatment of chronic canaliculitis. Arch Ophthalmol. 1992;110(2):200-2.
8. Anand S, Hollingworth K, Kumar V, Sandramouli S. Canaliculitis: the incidence of long-term epiphora following canaliculotomy. Orbit. 2004;23(1):19-26.
9. Baratz KH, Bartley GB, Campbell RJ, Garrity JA. An eyelash nidus for dacryoliths of the lacrimal excretory and secretory systems. Am J Ophthalmol. 1991;111(5):624-7.
10. Mohan ER, Kabra S, Udhay P, Madhavan HN. Intracanalicular antibiotics may obviate the need for surgical management of chronic suppurative canaliculitis. Indian J Ophthalmol. 2008;56(4):338-40.
Submitted for publication:
January 22, 2018.
Accepted for publication:
April 10, 2018.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose