

Zélia M. Correa1; Bradley Huth2; James J. Augsburger1
DOI: 10.5935/0004-2749.20180064
ABSTRACT
Purpose: To evaluate the incidence, potential correlation with transcleral fine needle aspiration biopsy, and treatment of scleral necrosis in patients with posterior uveal melanomas treated by 125I plaque radiotherapy and assessed by transcleral fine needle aspiration biopsy.
Methods: We performed a retrospective review of posterior uveal melanoma treated by 125I plaque radiotherapy at a single academic institution between July 2006 and July 2013. Consecutive patients diagnosed with a posterior uveal melanoma during the study period that had an anterior margin at or anterior to the equator who were evaluated by transcleral fine needle aspiration biopsy prior to 125I plaque radiotherapy were included. The main outcome measure was development of scleral necrosis, and the secondary outcome was treatment of this complication. Statistical analysis included computation of conventional descriptive statistics, cross-tabulation and chi-square tests of potential factors related to the development of scleral necrosis, and summarizing of treatment approaches and results. The incidence of treatment of scleral necrosis was calculated using the Kaplan-Meier method.
Results: During the 7-year study period, 87 posterior uveal melanomas were evaluated by transcleral fine needle aspiration biopsy and treated by 125I plaque radiotherapy. The median largest basal diameter of the tumor was 13.3 mm, and the median thickness was 6.8 mm. Eight patients (9.2%) developed scleral necrosis during follow-up. Thicker tumors (> 6.5 mm) were more likely to develop scleral necrosis (n=7) than thinner tumors (p=0.05). The median interval between 125I plaque radiotherapy and detection of scleral necrosis was 19.1 months. The overall cumulative probability of scleral necrosis was 6.2% at 6 months and 14.3% at 24 months, subsequently remaining stable. For thicker tumors, the probability of scleral necrosis was 23.5% at 45.4 months. Five patients were treated by scleral patch graft (62.5%) and three by observation (37.5%). One patient underwent enucleation after two failed scleral patch attempts and recurrent scleral necrosis. The mean follow-up period for patients with scleral necrosis was 34.5 months.
Conclusions: Thicker posterior uveal melanomas are more likely to develop scleral necrosis after 125I plaque radiotherapy and transcleral fine needle aspiration biopsy. While observation is sufficient for managing limited scleral necrosis, scleral patch graft is a viable alternative for eye preservation in extensive scleral necrosis.
Keywords: Melanoma; Uveal neoplasms; Iodine radioisotopes; Brachytherapy; Necrosis; Sclera; Biopsy, fine needle
RESUMO
Objetivo: Avaliar incidência, possível correlação da biópsia aspirativa com agulha fina trans-escleral e manejo da necrose escleral em pacientes com melanoma da úvea posterior tratados com placa de Iodo-125 (PLACA) avaliados pela biópsia aspirativa com agulha fina trans-escleral.
Métodos: Revisão retrospectiva de melanoma da úvea posterior tratados com placa de Iodo-125 entre 07/2006 e 07/2013 em uma única instituição acadêmica. Pacientes diagnosticados consecutivamente com melanoma da úvea posterior durante o intervalo desse estudo cuja margem anterior está no equador ou anterior ao mesmo e foram avaliados pela biópsia aspirativa com agulha fina trans-escleral antes do tratamento com PLACA foram incluídos. O principal desfecho avaliado foi desenvolvimento de necrose escleral e o desfecho secundário foi o manejo dessa complicação. Análise estatística incluiu computação de variáveis descritivas convencionais; tabulação e teste do Chi-quadrado de fatores potencialmente relacionados com o desenvolvimento de necrose escleral e sumarização do manejo dessa complicação. A incidência de necrose escleral foi calculada usando o método de Kaplan-Meier.
Resultados: Durante o período de 7 anos desse estudo, 87 melanomas da úvea posterior foram avaliados pela biópsia aspirativa com agulha fina trans-escleral e tratados com placa. A mediana do maior diâmetro basal tumoral foi 13,3 mm e a mediana da espessura foi 6,8 mm. Oito pacientes (9,2%) desenvolveram necrose escleral durante o período de acompanhamento. Tumores mais espessos (> 6,5 mm) foram mais propensos a desenvolver necrose escleral (n=7) que tumores mais finos (p=0,05). O intervalo mediano entre PLACA e a detecção da necrose escleral foi 19,1 meses. Probabilidade cumulativa de desenvolvimento de necrose escleral foi 6,2% em 6 meses e 14,3% em 24 meses permanecendo estável subsequentemente. Em tumores espessos, a probabilidade de necrose escleral foi 23,5% em 45,4 meses. Cinco pacientes foram manejados com enxerto escleral (62,5%), 3 foram observados (37,5%). Um paciente foi enucleado após 2 enxertos esclerais com necrose escleral recidivada. Tempo de seguimento médio dos pacientes com necrose escleral foi 34,5 meses.
Conclusões: Tumores espessos pareceram mais propensos a desenvolver necrose escleral após PLACA e biópsia aspirativa com agulha fina trans-escleral para melanoma da úvea posterior. Apesar de observação para necrose escleral limitada ser suficiente, enxerto de esclera é uma alternativa viável para preservação ocular em necrose escleral extensa.
Descritores: Melanoma; Neoplasias uveais; Radioisótopos de iodo; Braquiterapia; Necrose; Esclera; Biopsia por agulha fina
INTRODUCTION
Focal radiation therapy delivered by plaque brachytherapy, proton beam radiotherapy, or stereotactic radiation therapy is the standard treatment for ciliary body and choroidal melanoma(1), particularly given that the Collaborative Ocular Melanoma Study showed that there were no differences in survival outcomes and small differences in quality of life outcomes between patients treated with plaque radiotherapy and those treated with enucleation(2). The total dose of radiation delivered is dependent on tumor size and location. I plaque radiotherapy for uveal melanoma generally125 requires a dose of 80 to 100 Gy to the tumor apex and 350 to 400 Gy to the tumor base(2,3).
Ocular complications after plaque radiotherapy for posterior uveal melanoma (PUM) have been studied extensively(3-5). These complications include radiation-induced dry eye in 8% of patients, diplopia in 10% of patients, strabismus in 2% of patients, keratitis in 4% to 21% of patients, iris neovascularization in 4% to 23% of patients, neovascular glaucoma in 2% to 45% of patients, cataract in 8% to 68% of patients, vitreous hemorrhage in 4% to 18% of patients, radiation retinopathy in 10% to 63% of patients, radiation maculopathy in 13% to 52% of patients, optic neuropathy in 4% to 46% of patients, and scleral necrosis in 7% to 33% of patients(3,4).
Scleral necrosis (SNEC) after plaque radiotherapy is an unusual complication of plaque therapy(6). A study has shown an incidence of SNEC of 7% among patients treated with 60Co and 1% among those treated with 125I(3). Conversely, surgically induced necrotizing sclerokeratitis has been described after intracapsular and extracapsular cataract extraction with large corneoscleral wounds exposing the inflammatory potential of full-thickness scleral incisions(7). Although the etiology of postsurgical SNEC is unknown, it is possible that focal radiation cumulatively increases the local inflammation caused by the plaque implantation and fine needle aspiration biopsy (FNAB) procedures. Given that many centers are adopting FNAB as a means of obtaining clinically relevant information about tumor diagnosis and prognosis prior to treatment, and the transcleral fine needle aspiration biopsy (tsFNAB) approach seems to be preferred over the transvitreal route because it minimizes the risks of retinal detachment and vitreous hemorrhage, the authors felt the importance of analyzing the impact of such procedures on the outcome of these patients.
The purpose of this study was to evaluate the incidence and treatment of SNEC in posterior uveal melanomas treated by 125I plaque radiation and evaluated by tsFNAB prior to treatment.
METHODS
This study followed the tenets of the Declaration of Helsinki and was approved by the University of Cincinnati’s Institutional Review Board as part of an ongoing data collection of the Ocular Oncology database.
The study is a retrospective chart review of all patients with posterior uveal melanomas treated by radiation between July 2006 and July 2013 in our single center. We selected patients with ciliochoroidal or choroidal melanocytic tumors with anterior margins at or anterior to the equator who were evaluated by tsFNAB prior to or at the time of treatment with 125I plaque radiation. The technique used for tsFNAB consists of conjunctival peritomy exposing the quadrant where the tumor is located and securing the rectus muscles closest to the tumor site to allow positioning immobilization of the eye. Transillumination is then used to outline the shadow cast by the tumor. Although some patients require temporary disinsertion of one rectus muscle to allow adequate positioning of the plaque, the partial thickness lamellar incision is performed at least 3 mm away from the muscle insertion and preferably on the (previously identified) thickest portion of the tumor. A 25-gauge needle is passed through the scleral incision and into the tumor. The assistant performs manual aspiration while the surgeon holds the aspirating needle. The sampling process is repeated three times, after which a separate 7-0 polyglactin 910 suture is used to close the biopsy site. In cases where the tumor is immediately treated, the radioactive 125I plaque is then placed over the biopsy site, covering the tumor shadow, and secured with four 5-0-nylon sutures for the duration of treatment. The conjunctiva is closed with separate 7-0 polyglactin 910 l sutures. During treatment with the plaque, the amount of radiation delivered to the sclera overlying the tumor varies, depending on tumor thickness and largest basal diameter, to ensure delivery of a target dose of 80 Gy to the tumor apex.
Following treatment, the patients were evaluated at least 1, 3, 6, and 12 months after radiation and once yearly after that. Patient evaluations consisted of comprehensive eye examination, B-scan ultrasound, and/or ultrasound biomicroscopy (UBM) to evaluate tumor regression.
In this study, the information collected included deidentified demographic data, tumor site, date of treatment and type of radiation used, time of follow-up and development of SNEC, detection of metastasis, and death.
Statistical analysis using the IBM Statistical Package for the Social Sciences (SPSS) software for Windows included computation of conventional descriptive statistics, cross-tabulation and chi-square tests of factors possibly related to the development of SNEC, and summarizing of treatment approaches and results. The incidence of SNEC was calculated by the Kaplan-Meier method.
RESULTS
A total of 435 patients with PUM were treated during the 7-year study period. Eighty-seven patients were evaluated by tsFNAB and subsequently treated by 125I plaque radiation. Fifty-one percent of patients were women (n=43), and the location of the tumor was almost equally distributed; 50.6% of patients had ciliary body involvement (n=44). In 93.1% of patients, tsFNAB was performed at the time of plaque implantation.
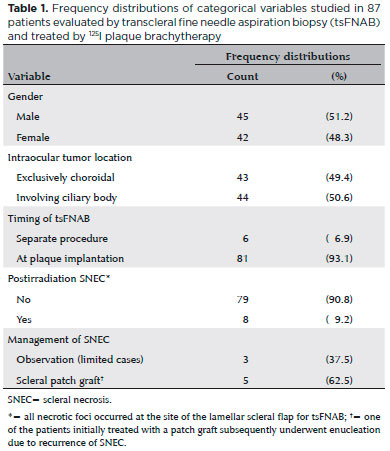
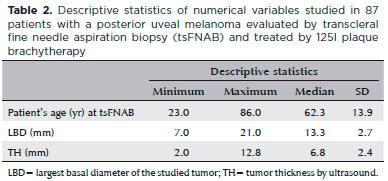
Table 1 summarizes the frequency distributions of the categorical variables studied. The median patient age was 62.3 (± 13.9) years. The median largest basal diameter was 13.3 (± 2.7) mm, and the median tumor thickness was 6.8 (± 2.4) mm. Table 2 summarizes the descriptive statistics of the numerical variables studied.
Eight patients (9.2%) developed SNEC after 125I plaque treatment. All patients had one rectus muscle disinserted, but SNEC did not develop at the muscle stump. The cumulative probability of development of SNEC after radiation treatment and tsFNAB is shown in figure 1. The tumors that developed SNEC measured 6, 7.6, 8.5, 9, 9.1, 9.5, 9.8, and 11.5 mm. Thicker tumors (> 6.5 mm) were significantly more likely to develop SNEC (n=7) than thinner tumors (p=0.05).
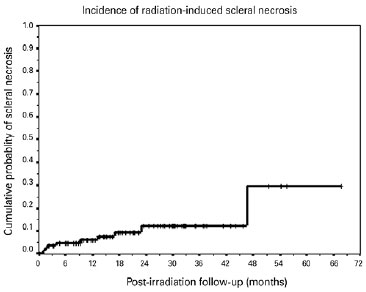
The median interval between 125I plaque treatment and detection of SNEC was 19.1 months. The cumulative probability of developing radiation-induced SNEC was 6.2% at 6 months, 7.4% at 12 months, 10.1% at 18 months, and 14.3% at 24 months, remaining stable thereafter, with a probability of 14.3% at 42 months (Figure 1). The cumulative probability of developing radiation-induced SNEC for thicker tumors was 23.5% at 45.4 months.
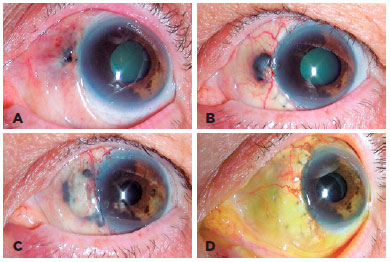
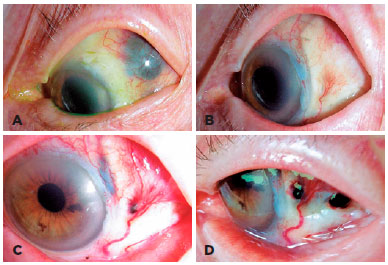
All patients with SNEC had intraocular pressure (IOP) measurements of 18 mmHg or higher, and those needing additional patch grafts had IOP measurements of 20 mmHg or higher (with the use of topical anti-glaucomatous medications). The treatment of patients who developed SNEC varied according to the extent of the scleral defect, visual acuity, and the presence or absence of rubeosis iridis and neovascular glaucoma (Figures 2 and 3). Five patients were treated by implantation of a scleral patch graft (62.5%) and three were treated by observation (37.5%). One of these patients underwent enucleation after two failed patch grafts due to recurrence of SNEC and development of neovascular glaucoma (Figure 3).
The mean follow-up period was 22.1 (± 14.0) months among patients who did not develop SNEC and ±34.5 months among those who developed SNEC. Of the eight patients who developed SNEC, only one died, due to cardiovascular disease; another developed metastasis but at the present time is doing well with systemic treatment 22 months later. The overall cumulative probability of survival for the entire group was 77.3%.
DISCUSSION
The effect of ionizing radiation delivered through low-dose brachytherapy on living cells has been thoroughly studied by several authors(3,4). At the cellular level, lower radiation doses (up to 30 Gy) have been shown to increase membrane permeability. Higher doses rupture membranes, causing cell death. Doses of 5 to 100 Gy disrupt cytoplasmic lysosomes, releasing enzymes that digest cellular structures. Given that disturbed mitochondrial function interrupts the production of adenosine triphosphate (ATP), cell death occurs after all ATP is used. Irradiated cells may enter abnormal and fatal mitosis or a prolonged phase of cell-cycle arrest once they can no longer divide, which is followed by senescence and eventual death. Another mechanism of cell death is apoptosis, which occurs by activation of the TP53 gene by irreparable DNA damage(8).
Several possible mechanisms may explain the early development of scleral defect in this subset of patients. First, a direct necrotizing effect of radiation on the sclera is possible. However, the scleral dose of radiation received follows the tumor apical dose recommended by the Collaborative Ocular Melanoma Study(9), and it is uniform regardless of tumor location. Such a dose is generally well tolerated by the sclera. Second, indirect effects of treatment on the sclera may have occurred because of local ischemic inflammation related to disinsertion of extraocular muscle(s) that varies depending on tumor location, intraocular tumor necrosis, or both. However, because the sclera is relatively avascular and experimental vascular deprivation has not been shown to trigger scleral changes, this mechanism alone cannot be responsible for the development of SNEC(10). Third, an occult systemic autoimmune vasculitic disease may have precipitated postoperative SNEC. Fourth, either the direct or the indirect effects of surgery mentioned above could have been synergistic with the presence of an occult systemic autoimmune vasculitic disease(7). Finally, focal weakening of the sclera because of tsFNAB and/or unrecognized perforation during disinsertion or reinsertion of extraocular muscles could increase the likelihood of SNEC(6). All patients who developed SNEC had one of the rectus muscles disinserted. Interestingly, none of the patients developed SNEC at the muscle insertion.
Studies have found tumor thickness >6-7 mm, ciliary body involvement, radiation dose to the sclera >400 Gy, intraocular pressure >21 mmHg, and ciliary body location as important risk factors for SNEC(3,11,12). Similarly, we found that thicker tumors (which received a higher dose of radiation to the sclera) to be a significant factor. Further, it seems that higher IOP may have a mechanical effect on the already weakened and ischemic sclera, pushing the necrotic tumor to extrude. Additionally, it seems that ciliary body or pre-equatorial location correlates with larger tumors, and in our series, the area of tumor necrosis was coincidentally the site of tsFNAB.
Our rationale for studying this select group of patients was based on our personal observation of an increase in SNEC at the site of tsFNAB. This observation, coupled with the rise of the transcleral sampling approach, suggested that it was reasonable to take a critical look at these data. Despite the possibility of such a finding happening by chance, this series suggests that the surgical technique used for tsFNAB (with a scleral flap over the puncture site) had a potential role in the development of radiation-induced SNEC in patients treated by plaque radiotherapy. Although the precise cause of the SNEC cannot be established in each patient with certainty, certain measures can be taken to minimize postoperative inflammation, such as sub-Tenon’s steroids or longer-term topical steroids; different surgical techniques to decrease the weakness of the scleral wall and use of nonabsorbable sutures may also help to decrease the incidence of SNEC.
While observation has been our choice for management of limited SNEC, the scleral patch graft is a safe alternative for eye preservation in cases of extensive SNEC. The choice of enucleation of eyes with SNEC depends greatly on the extent of the eye wall defect, the amount of exposed uveal tissue, vision potential, intraocular pressure, and ocular comfort reported by the patient.
In summary, this series of cases shows that patients with thicker tumors are more likely to develop SNEC after plaque radiotherapy, thus confirming the role of radiation dose and possibly tsFNAB in this process.
REFERENCES
1. Radin PP, Lumbroso-Le Rouic L, Levy-Gabriel C, Dendale R, Sastre X, Deshardubs K. Scleral necrosis after radiation therapy for uveal melanomas: report of 23 cases. Graefes Arch Clin Exp Ophthalmol. 2008;246(12):1731-6.
2. Collaborative Ocular Melanoma Study Group. The COMS randomized trial of iodine 125 brachytherapy for choroidal melanoma: V. Twelve-year mortality rates and prognostic factors: COMS report No. 28. Arch Ophthalmol. 2006;124(12):1684-93.
3. Kaliki S, Shields CL, Rojanaporn D, Badai J, Devisetty L, Emrich J, et al. Scleral necrosis after plaque radiotherapy of uveal melanoma: a case-control study. Ophthalmology. 2013;120(5):1004-11.
4. Puusaari I, Heikkonen J, Kivela T. Ocular complications after iodine brachytherapy for large uveal melanomas. Ophthalmology. 2004; 111(9):1768-77.
5. Suesskind D, Scheiderbauer J, Buchgeister M, Partsch M, Budach W, Bartz-Schmidt KU, et al. Retrospective evaluation of patients with uveal melanoma treated by stereotactic radiosurgery with and without tumor resection. JAMA Ophthalmol. 2013;131(5):630-7. Comment in: JAMA Ophthalmol. 2014;132(3):367-8.
6. Correa ZM, Augsburger JJ, Freire J, Eagle RC Jr. Early-onset scleral necrosis after iodine I 125 plaque radiotherapy for ciliochoroidal melanoma. Arch Ophthalmol. 1999;117(2):259-61.
7. O’Donoghue E, Lightman S, Tuft S, Watson P. Surgically induced necrotising sclerokeratitis (SINS)-precipitating factors and response to treatment. Br J Ophthalmol. 1992;76(1):17-21.
8. Groenewald CK, Damato B. Effects of radiotherapy on uveal melanomas and adjacent tissues. Eye (London). 2013;27(2):163-71.
9. Chiu-Tsao ST, Astrahan MA, Finger PT, Followill DS, Meigooni AS, Melhus CS, et al. Dosimetry of (125)I and (103)Pd COMS eye plaques for intraocular tumors: report of Task Group 129 by the AAPM and ABS. Med Phys. 2012;39(10):6161-84.
10. Doshi RR, Harocopos GJ, Schwab IR, Cunningham ET Jr. The spectrum of post-operative necrosis. Surv Ophthalmol. 2013;58(6):620-33.
11. Gunduz KS, Shields CL, Shields JA, Cater J, freira JE, Brady LW. Plaque radiotherapy of uveal melanoma with predominant ciliary body involvement. Arch Ophthalmol. 1999;117(2):170-7.
12. Chaudhry IA, Liu M, Shamsi FA, Arat YO, Shetlar DJ, Boniuk M. Corneoscleral necrosis after episcleral Au-198 brachytherapy of uveal melanoma. Retina. 2009;29(1):73-9.
Submitted for publication:
April 24, 2017.
Accepted for publication:
February 8, 2018.
Approved by the following research ethics committee: University of Cincinnati (# 2012-4914)
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose