

Tiago Ribeiro Schmalfuss1; Egidio Picetti2; Helena Messinger Pakter3
DOI: 10.5935/0004-2749.20180051
ABSTRACT
The diagnosis of angle-closure glaucoma secondary to iridociliary cysts is challenging and lacks compiled literature support. We present a rare case of bilateral angle-closure glaucoma associated with pseudoplateau iris due to multiple ciliary cysts and conducted a systematic review of the literature to find similar case reports published between November 2006 and November 2016. Only 19 case reports present treatment modalities, and most cases required more than one therapeutic approach for controlling the intraocular pressure. Pseudoplateau iris attributed to iridociliary cysts should be considered in the differential diagnosis of patients with narrow angles, particularly those with ocular hypertension and glaucoma, in which management is complex. In addition to gonioscopy, ultrasound biomicroscopy is considered the conclusive method for accurate diagnosis.
Keywords: Angle-closure glaucoma; Cyst complications; Ciliary body; Iris diseases; Ultrasound biomicroscopy; Differential diagnosis Pseudoplateau iris
RESUMO
O diagnóstico de glaucoma de ângulo fechado secundário a cistos iridociliares é desafiador e não possui suporte da literatura compilada. Apresentamos um caso bilateral raro de glaucoma de ângulo fechado associado à íris pseudoplateau devido a cistos ciliares múltiplos e realizamos uma revisão sistemática da literatura de relatos de casos similares publicados entre novembro de 2006 e novembro de 2016. Apenas 19 relatos de casos apresentaram as modalidades de tratamento e na maioria deles foi necessário mais de uma abordagem terapêutica para controlar a pressão intra-ocular. Íris pseudoplateau atribuída a cistos iridociliários deve ser considerada no diagnóstico diferencial de pacientes com ângulos estreitos, particularmente aqueles com hipertensão ocular e glaucoma, em que o manejo é complexo. Além da gonioscopia, a biomicroscopia ultra-sônica é considerada o método conclusivo para o diagnóstico correto.
Descritores: Glaucoma de ângulo fechado/etiologia; Cistos/complicações; Corpo ciliar; Doenças da íris; Biomicroscopia ultra-sônica; Diagnóstico diferencial; Íris pseudoplateau
INTRODUCTION
Primary iridociliary cysts can push the iris root anteriorly, causing a pseudoplateau iris configuration, with or without angle-closure glaucoma(1,2). Primary ciliary body cysts occur spontaneously and are epithelial-lined spaces arising from the pigmented epithelial layer of the iris and ciliary body(3). Secondary ciliary body cysts arise from traumatic implantation of the epithelium, from metastatic or parasitic lesions, or after the long-term use of miotics(4,5). Although the majority of the iridociliary cysts run a benign course, rarely causing complications or requiring treatment(2), angle-closure glaucoma may develop when an angle greater than 180° is involved(5). Ultrasound biomicroscopy enables accurate diagnosis, identifying cysts at the ciliary body that mimic the plateau iris syndrome(1). This condition, known as pseudoplateau iris syndrome, is difficult to detect clinically. By providing a high-resolution view of the iris and ciliary body, ultrasound biomicroscopy is a useful adjunct to the clinical examination in distinguishing primary cysts of the iris pigment epithelium from solid uveal neoplasia(6).
This report presents a systematic review of case reports of ciliary body cysts and pseudoplateau iris in the literature. We also present a rare case of bilateral angle-closure-glaucoma-associated pseudoplateau iris secondary to the presence of multiple cysts of the ciliary body.
CASE REPORT
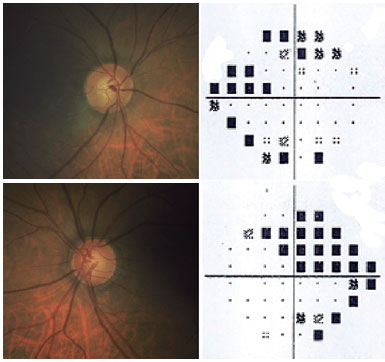
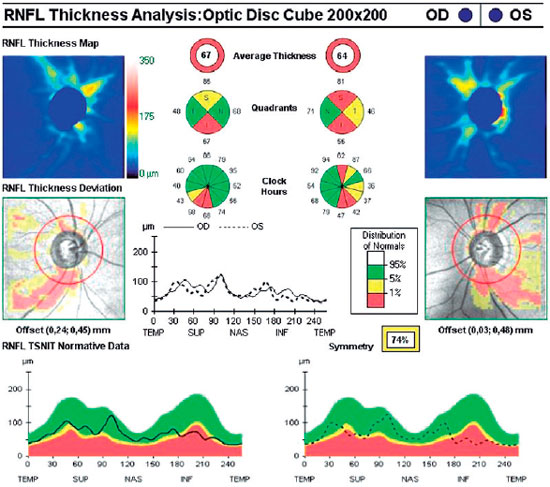
A 54-year-old Brazilian white male was referred to the glaucoma service of Hospital Nossa Senhora da Conceição, Porto Alegre, Brazil for evaluation of his chronic, uncontrolled bilateral glaucoma. His previous medical history was remarkable for diabetes mellitus and systemic arterial hypertension. He was using several glaucoma medications, including timolol, brimonidine, and latanoprost. His corrected visual acuity was 20/20 in both eyes (refractive error: right eye, +1.25; left eye, +0.75). Intraocular pressure (IOP), as measured by Perkins applanation tonometry, was 34 mmHg in the right eye (RE) and 38 mmHg in the left eye (LE). The central corneal thickness was 546 in the RE and 560 in the LE. On anterior segment examination, a very shallow anterior chamber was noted bilaterally; gonioscopy revealed bilateral narrow iridotrabecular angles. Schwalb's line was only visible by indention in both eyes, and there were no peripheral anterior synechiae. Optic discs had remarkable cupping (cup-to-disc ratio, 0.7) and inferior temporal thinning of the neuroretinal rim in both eyes. Both eyes had a corresponding upper nasal scotoma at the Humphrey visual field (Figure 1). The retinal nerve fiber layer, as measured by optical coherence tomography, was decreased inferiorly in both eyes (Figure 2).
Primary angle-closure glaucoma was diagnosed and Neodymium:yttrium-aluminum-garnet (Nd:YAG) laser peripheral iridotomy was performed in both eyes.
Despite the presence of patent iridotomies, the IOP remained high in both eyes, and repeat gonioscopy revealed no change in the iridotrabecular angle configuration.
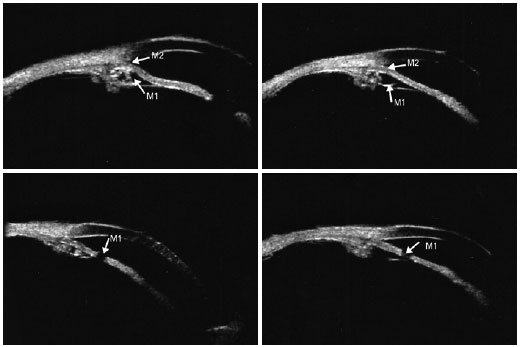
Ultrasound biomicroscopy (UBM) of the angles confirmed the presence of very narrow or opposed iridotrabecular angles with multiple cysts at the iris root and iridociliary junction in all meridians. Laser iridotomies confirmed patency in both eyes (Figure 3).
The decision was made to initiate pilocarpine (2%) treatment, which markedly reduced the IOP to 12 mmHg in both eyes. The patient has been followed now for over 18 months. He is on pilocarpine, brimonidine, and timolol; the IOP remains near 12 mmHg in both eyes. There has been no glaucoma progression during this 18-month follow up.
SYSTEMATIC REVIEW
In light of this case, we performed a systematic review of the literature, searching the Medline (PubMed) database for all English and non-English articles published between November 1, 2006 and November 30, 2016. We used the following search words: “ciliary body cyst OR pseudoplateau iris OR iridociliary cyst OR plateau-like iris.” Only case reports articles were included. We confined our search to studies in humans. Any additional studies cited in review articles were also investigated. We also contacted experts in this field of study regarding similar cases.
Data extraction was performed independently by two researchers (TR Schmalfuss and E Picetti) using a customized protocol. Any disagreement was resolved by consensus. The data extraction form included the title, authors, country of origin, year of publication, number of patients/eyes, patient age and gender, number and shape of the ciliary cysts, iridotrabecular angle configuration, presence of increased intraocular pressure and/or glaucoma damage, treatment, and outcome.
We used the CARE guidelines to assess the quality of the case reports(7).
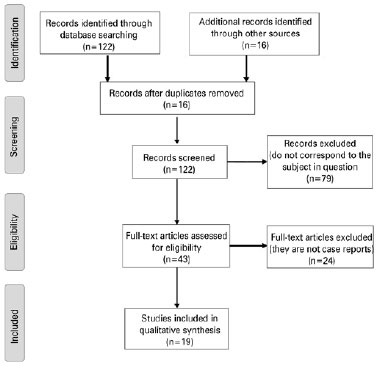
RESULTS
Overall 122 articles were published during this 10-year period. Of these, only 43 corresponded to the desired subject matter (ciliary or iridociliary body cyst in humans) and only 19 were case presentations. We include a PRISMA flow diagram to depict the flow of information through the different phases of this systematic review (Diagram 1)(8). A list of excluded articles is available upon request. We found that most of these articles met the criteria for quality set by the CARE guidelines (detailed information upon request).
Of the 19 articles included in this review, the reports include 13 bilateral cases, 7 unilateral cases (one author reports two unilateral cases), adding up to 20 cases involving 33 eyes. All included studies, their patient characteristics, treatments, and outcomes are listed in table 1. To allow for comparisons, we also included our reported case in this table, making a total of 35 eyes.
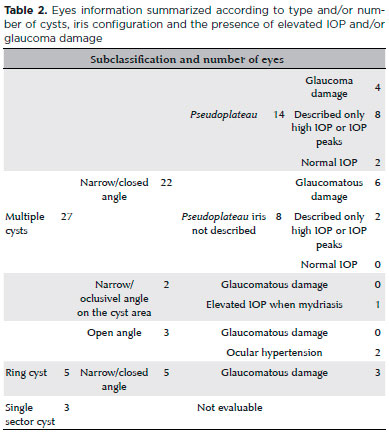
Of the 35 eyes, 27 had multiple iridociliary or ciliary cysts, 22 had narrow or closed angles, and 14 had a pseudoplateau iris configuration. To summarize the case report findings, we divided the eyes according to type and/or number of cysts, iris configuration, and the presence of elevated IOP and/or glaucoma damage. These data are shown in table 2. To describe patient treatments, we further classified the cases into 3 groups: group 1, eyes with ciliary body cyst/iridociliary cysts with a pseudoplateau iris; group 2, eyes with ciliary body cyst/iridociliary cysts and glaucoma due to angle closure but without a pseudoplateau iris; and group 3, the remaining eyes.
Group 1 comprises 7 articles(9-15) describing 8 patients (6 bilateral cases and 2 unilateral cases, totaling 14 eyes) with pseudoplateau iris configuration due to ciliary body cyst/iridociliary cysts. YAG LASER iridotomies were performed in all of those eyes. Following iridotomies, only two unilateral cases(9) had an open angle configuration. In all other cases, patent iridotomies neither opened the angle and nor controlled the IOP, and different therapeutic strategies were implemented. Following iridotomy, one of the patients underwent LASER iridoplasty in one eye(10), which changed the configuration of the root of the convex iris to concave and led to the disappearance of the cysts; the IOP decreased to 17 mmHg without further treatment. In this case, the IOP was within the normal limits for up to 6 months. Using UBM, it was possible to observe the reappearance of the cysts in the laser-treated eye and that the return of the iris pseudoplateau configuration; the IOP increased again. Timolol (0.5%, bid) was prescribed, and at the 12-month follow up, the IOP was 14 mmHg in both eyes. Ang et al.(11) reported a case of bilateral narrow iridotrabecular angle with plateau iris configuration, elevated IOP, but with no glaucoma damage. Iridotomy was performed in both eyes, but the iridotrabecular angle configurations did not change. Argon laser peripheral iridoplasty was than performed in the LE, and again, there was no change in the angle configuration. Since the patient was asymptomatic and had no signs of glaucoma damage, although the IOP ranged from 18 to 26 mmHg in both eyes, they elected to monitor him closely without further treatment. In another case(12), after failure of IOP control with iridotomy and iridoplasty, the eye underwent phacoemulsification, resulting in the opening of the angle and IOP control. In 3 cases, the IOP was controlled only with timolol(10,13,14). In one case, the IOP was controlled with pilocarpine only(15), and in one case, the IOP was controlled only with the combination of pilocarpine, timolol, and brimonidine (our patient).
Group 2 comprises 7 studies,(16-22) including 7 case reports presenting with iridociliary cysts and glaucoma with angle closure but with no pseudoplateau iris configuration. Three of these cases had ring iridociliary cysts(16-18), and the other 4 had multiples cysts(19-22). In all cases with ring iridociliary cysts, medical therapies were ineffective. In one of those cases(16), the IOP was controlled after phacoemulsification and endocycloplasty. In another(17), the IOP was controlled after lens extraction via pars plana, IOL implantation in the capsular bag, anterior capsulotomy, and posterior sinequialisis. Choudhari et al.(18), describe a case in which they performed YAG LASER to rupture the cyst in the RE, despite the fact that the IOP was normal. In the LE (fellow eye), which had uncontrolled IOP despite medication, 180° transscleral diode cyclophotocoagulation was performed; the IOP still was not controlled. Of the 4 cases involving multiple cysts(19-22), one is described by Mosaed et al.(19) as requiring Baerveldt Glaucoma Implantation combined with medical therapy to achieve IOP control. In another multiple cyst case(20), topical medication was combined with oral acetazolamide to achieve what the authors refer as “acceptable” IOP (RE 20 mmHg and LE 10 mmHg). Gabriel et al.(21) reported a case of bilateral glaucoma with iridocorneal and iridolenticular synechiae, which they treated using maximal topical antiglaucomatous medication in both eyes. Approximately 4 years following this management, the patient's IOP became uncontrolled. The LE was performed trabeculectomy with mitomicina C and, approximately 1 year later, a pars plana lensectomy and vitrectomy with glaucoma shunt valve implant. The IOP remains controlled. In the case described by Katsimpris et al.(22) no therapy was given and cataract extraction was proposed for both eyes in the immediate future.
Group 3 comprises 5 reports(23-27) describing cases that did not fit under the aforementioned categories. Aykan et al.(23) describes a bilateral case of multiple iridociliary cysts, ocular hypertension, and open angle that was treated using Nd:YAG laser iridocystotomy followed by selective laser trabeculoplasty (inferior 180°); no further ocular medication was needed. The other 4 articles(24-27) do not describe how the conditions were treated.
Similar to the mechanism of angular closure by pseudoplateau iris due to iridociliary cysts, a report describes the occurrence of angle closure caused by a combination of a plateau-like iris and enlarged Soemmering's ring in the pseudophakic eye(28). Soemmering's ring is a structure that results from the proliferation of lenticular epithelial cells in the peripheral part of the capsular bag that remain after cataract extraction. Kitamura et al.(28) report a case of plateau-like iris and angle closure induced by enlarged Soemmering's ring and uncontrolled IOP despite a patent iridectomy and treatment with latanoprost, timolol, and dorzolamide. The IOP decreased to normal after treatment with 2% pilocarpine.
DISCUSSION
Here we describe a unique case of bilateral glaucoma secondary to iridociliary cysts and pseudoplateau iris configuration. We also performed a systematic review of case reports of ciliary body cysts. We found that among the articles that clearly describe angle closure due to pseudoplateau iris secondary to iridociliary cysts, none of the cases described were bilateral. After attempting different treatment modalities, we were able to control the IOP using topical 2% pilocarpine, which was reported only in one of the cases reviewed.
Similar to a case described by Baba et al.(15), our patient responded very well to pilocarpine treatment with IOP control over the 18-month follow-up period. Nevertheless, it is important to state that the chronic use of pilocarpine is not free of side effects and, in fact, preferably should be used for short periods of time. For instance, pilocarpine may not prevent intermittent angle closure attacks and anterior peripheral synechiae. In addition, its chronic use may lead to posterior synechia, which in turn may make mydriasis difficult, complicating the visualization of cysts and performance of transpupillary cystotomy. For these reasons, our patient has been closely followed and observed for synechiae formation, and we have plans for cystotomy in the near future.
Shukla et al.(29) retrospectively analyzed 76 patients referred to a UBM clinic for evaluation of the angle-closure mechanism. Although the study was not designed to investigate treatment modalities, they reported that out of the 21 patients diagnosed with pseudoplateau iris due to iridociliary cysts, the vast majority had laser iridotomies (18 patients) and/or used pilocarpine (11 patients); only 1 patient underwent trabeculectomy at some point during follow up. We suppose that in fact all of these iridotomies were performed because the mechanism of the angle closure was not obvious before the UBM results.
Our review of the literature shows that different treatment modalities have been tried for controlling ocular hypertension and/or glaucoma damage. Peripheral iridotomy proved to be ineffective for angle opening and IOP control in most cases. In these cases, iridotomy did not prevent intermittent angle-closure attacks, mainly because the pupillary blockage mechanism is irrelevant in these cases.
Some cases initially responded well to medical therapy, but in longer follow-ups, most cases required surgical intervention to control IOP. Three authors(10,11,12) attempted to treat the eyes with iridoplasty, which successfully opened up the angle and controlled the IOP for 6 months in one case(10), and was ineffective in the other cases(11,12). In 2005, Crowston et al.(30) described a case of angle-closure glaucoma associated with the pseudoplateau iris by iridociliary cysts in which argon laser peripheral iridoplasty opened the angle and controlled the IOP.
Despite our effort to perform a wide literature search, our results are subject to publication bias. Many other similar cases may not have been reported in the literature and therefore are not included in this review. Another limitation of our study is that some of the reports did not clearly state all the information regarding their cases, which limits our ability to make comparisons.
CONCLUSIONS
Although a relatively rare entity, pseudoplateau iris secondary to iridociliary cysts is a differential diagnosis that should be considered in patients with a narrow angle, especially in cases of ocular hypertension or glaucoma not responsive to peripheral iridotomy. The differential diagnosis between plateau and pseudoplateau iris is important for adequate therapeutic management, since each of these entities presents different characteristics. Gonioscopy is import for the initial examination of these patients, but UBM is the definitive examination used to distinguish between these diagnoses. No one therapy is ideal for treating all cases of pseudoplateau iris secondary to iridociliary cysts and associated with ocular hypertension or glaucoma. This entity remains a therapeutic challenge, and new research is needed to better understand and treat these patients.
REFERENCES
1. Azuara-Blanco A, Spaeth GL, Araujo SV, Augsburger JJ, Terebuh AK. Plateau iris syndrome associated with multiple ciliary body cysts. Report of three cases. Arch Ophthalmol. 1996;114(6):666-8.
2. Lois N, Shields CL, Shields JA, Mercado G. Primary cysts of the iris pigment epithelium. Clinical features and natural course in 234 patients. Ophthalmology. 1998;105(10):1879-85.
3. Shields JA. Primary cysts of the iris. Trans Am Ophthalmol Soc. 1981;79:771-809.
4. Shields JA, Kline MW, Augsburger JJ. Primary iris cysts: a review of the literature and report of 62 cases. Br J Ophthalmol. 1984;68(3): 152-66.
5. Marigo FA, Esaki K, Finger PT, Ishikawa H, Greenfield DS, Liebmann JM, et al. Differential diagnosis of anterior segment cysts by ultrasound biomicroscopy. Ophthalmology. 1999;106(11):2131-5.
6. O’Connor MD, Kertes PJ, Sheikh A. Multiple bilateral primary cysts of the iris pigment epithelium. Can J Ophthalmol. 2006;41(6):761-2.
7. Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D; CARE Group. The CARE guidelines: consensus-based clinical case reporting guideline development. Headache. 2013;53(10):1541-7.
8. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. PLoS Med [Internet]. 2009 [cited 2017 Jun 21];6(7):e1000097. doi:10.1371/journal.pmed1000097.
9. Berkani Kitouni Z, Kitouni Y, Boukhecham D, Kherroubi R, Hartani D. [Plateau-like iris configuration secondary to multiple iridociliary cysts: case report of one family]. J Fr Ophtalmol. 2015;38(3):e41-2. French.
10. Ispa-Callén MC, Lara-Medina J, Zarco-Tejada JM, López-Mondéjar E, Celis-Sánchez J, González-Del-Valle F. [Argon laser iridoplasty as treatment of plateau-like iris configuration secondary to multiple ciliary body cysts: long-term follow-up by ultrasound biomicroscopy]. Arch Soc Esp Oftalmol. 2009;84(11):569-72. Spanish.
11. Ang GS, Bochmann F, Azuara-Blanco A. Argon laser peripheral iridoplasty for plateau iris associated with iridociliary cysts: a case report. Cases J. 2008;1(1):368.
12. Vila-Arteaga J, Díaz-Céspedes RA, Suriano MM. Plateau iris secondary to iridociliary cysts. Arch Soc Esp Oftalmol. 2015;90(11):542-5.
13. Kaushik S, Ichhpujani P, Kaur S, Singh Pandav S. Optic disk pit and iridociliary cyst precipitating angle-closure glaucoma. J Curr Glaucoma Pract. 2014;8(1):33-5.
14. Le Corre A, Dot C, Feraoun M, Burelle X, Grasswill C, Perrenoud F, et al. [Plateau iris-like configuration resulting from numerous iridociliary cysts]. J Fr Ophtalmol. 2009;32(7):501-4. French.
15. Baba T, Hirooka K, Takagishi M, Sato S, Shiraga F. Plateau iris syndrome associated with cysts and nocturnal elevation of intraocular pressure. Can J Ophthalmol. 2008;43(6):725.
16. Pathak-Ray V, Ahmed II. Phaco-endocycloplasty: a novel technique for management of ring iridociliary cyst presenting as acute angle closure. Oman J Ophthalmol. 2016;9(1):63-5.
17. Seki M, Fukuchi T, Yoshino T, Ueda J, Hasebe H, Ueki S, et al. Secondary glaucoma associated with bilateral complete ring cysts of the ciliary body. J Glaucoma. 2014;23(7):477-81.
18. Choudhari NS, Amula GM, Neog A. Inadvertent rupture of iridociliary cyst following transscleral Diode laser. Indian J Ophthalmol. 2013;61(3):124-6.
19. Mosaed S, Jacobsen BH, Lin KY. Case report: imaging and treatment of ophthalmic manifestations in oculodentodigital dysplasia. BMC Ophthalmol. 2016;16:5.
20. Curtin J, Moloney G, Grigg J, Sharota Franzco D. Clinical characterization and proposed mechanism of juvenile glaucoma-a patient with a chromosome 4p deletion, Wolf-Hirschhorn Syndrome. Ophthalmic Genet. 2010;31(3):135-8.
21. Gabriel LA, Sachdeva R, Marcotty A, Rockwood EJ, Traboulsi EI. Oculodentodigital dysplasia: new ocular findings and a novel connexin 43 mutation. Arch Ophthalmol. 2011;129(6):781-4.
22. Katsimpris JM, Petropoulos IK, Sunaric-Mégevand G. Ultrasound biomicroscopy evaluation of angle closure in a patient with multiple and bilateral iridociliary cysts. Klin Monbl Augenheilkd. 2007; 224(4):324-7.
23. Aykan U, Yıldırım O. Combined laser treatment in a patient with pigment dispersion secondary to a large iris pigment epithelial cyst. Balkan Med J. 2012;29(3):339-42.
24. Aydin A, Kocak I, Sabahyildizi M. Auto-refractometry may assist in discovering asymptomatic iridociliary cysts. J Fr Ophtalmol. 2014; 37(5):e71-2.
25. Baile R, Sahasrabuddhe M, Nadkarni S, Karira V, Kelkar J, Bhonde S. Bilateral multiple primary iridociliary cysts - A rare case report. Saudi J Ophthalmol. 2011;25(1):89-91.
26. Rivero V, Aparicio MJ, Suárez-Leoz M, Fernández A. Vitreous hemorrhage secondary to iridociliary cyst. Arch Soc Esp Oftalmol. 2015;90(12):600-3.
27. Khan AO, Al-Assiri A. Lens coloboma associated with a ciliary body cyst. Ophthalmic Genet. 2007;28(4):208-9.
28. Kitamura F, Inoue T, Kuroda U, Tanihara H. Angle closure caused by a plateau-like iris associated with an enlarged Soemmering’s ring: a case report. BMC Ophthalmol. 2016;16(1):49.
29. Shukla S, Damji KF, Harasymowycz P, Chialant D, Kent JS, Chevrier R, et al. Clinical features distinguishing angle closure from pseudoplateau versus plateau iris. Br J Ophthalmol. 2008;92(3):340-4.
30. Crowston JG, Medeiros FA, Mosaed S, Weinreb RN. Argon laser iridoplasty in the treatment of plateau-like iris configuration as result of numerous ciliary body cysts. Am J Ophthalmol. 2005; 139(2):381-3.
Submitted for publication:
June 23, 2017.
Accepted for publication:
October 16, 2017.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose