

Antonio Ramos Suárez; Ana Chinchurreta Capote; Yolanda Fernández Barrientos; Mercedes Lorenzo Soto; Saturnino Gismero Moreno; Fernando García Martín
DOI: 10.5935/0004-2749.20180050
ABSTRACT
A 43-year-old male with a history of eosinophilic angiocentric fibrosis presented with headache and double vision since 48 h. Idiopathic hypertrophic pachymeningitis was diagnosed based on nuclear magnetic resonance and comprehensive systemic study findings. Eosinophilic angiocentric fibrosis and idiopathic hypertrophic pachymeningitis have been associated with IgG4-related diseases, but this was the first case in which they coexisted in the same patient. After steroid treatment failure, rituximab was used with excellent results.
Keywords: Headache; Meningitis; Magnetic resonance imaging; Eosinophilia; Fibrosis; Rituximab; Humans; Case reports
RESUMO
Um homem de 43 anos, com história de fibrose angiocêntrica eosinofílica, apresentou cefaléia e visão dupla com 48 horas. A paquimeningite hipertrófica idiopática foi diagnosticada com base na ressonância magnética nuclear e em achados sistêmicos abrangentes no estudo. A fibrose angiocêntrica eosinofílica e a paquimeningite hipertrófica idiopática foram associadas a doenças relacionadas à IgG4, mas este foi o primeiro caso em que elas coexistiram no mesmo paciente. Após a falha do tratamento com esteroides, o rituximabe foi usado com excelentes resultados.
Descritores: Cefaléia; Meningite; Imagem por ressonância magnética; Eosinofilia; Fibrose; Rituximab; Humanos; Relatos de casos
INTRODUCTION
Idiopathic hypertrophic pachymeningitis (IHP) is a rare condition characterized by thickening of the dura. It may present as a neuro-ophthalmological disorder and is usually accompanied by headache. The main clinical features at presentation include headache, loss of vision, diplopia, papilledema, and other cranial nerve involvement(1-9). Eosinophilic angiocentric fibrosis (EAF) is also a rare condition; it causes tumefactive lesions of the upper airways and orbit(10-12). Ophthalmic manifestations have been infrequently reported, mainly including orbital involvement that caused epiphora, proptosis, and diplopia. Both IHP and EAF have been associated with immunoglobulin G4 (IgG4)-related diseases (IgG4-RDs)(2-5,10,13).
We present the first case of IHP and EAF coexisting in the same patient.
CASE REPORT
A 43-year-old male, with a history of multiple nasal polyps secondary to EAF, presented with headache and horizontal diplopia since 48 h. EAF had been diagnosed 5 years earlier, but the patient was not under treatment.
The best corrected visual acuity (BCVA) was 1.0 for both the eyes. Examinations revealed orthophoria in the primary position, but adduction of the left eye was slightly limited. Pupillary reflexes, anterior pole, and fundoscopy findings were normal for both the eyes. Diplopia was only apparent on gazing to the right, due to which incomplete paralysis of the left third cranial nerve was diagnosed.
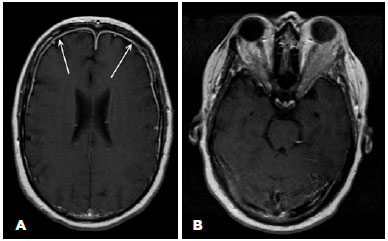
Brain magnetic resonance imaging (MRI) revealed meningeal thickening, which was strongly enhanced by contrast, mainly in the bilateral frontal region, affecting the orbital apex. Also, diffuse fat infiltration was evident in both the lateral orbit areas (Figure 1).
A comprehensive systemic study failed to reveal any underlying neoplastic, immunological, or infectious involvement. The erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels were slightly elevated (26 mm/h and 6.9 mg/l, respectively). Serum lgG4 levels were normal (24 mg/dl).
A lumbar puncture demonstrated normal opening pressure. Cytochemical analysis of the cerebrospinal fluid (CSF) showed a slight increase in protein levels and cellularity and decrease in lymphocyte counts. Microbiological findings were negative, and no tumor cells were evident. The patient refused to undergo meningeal or orbital biopsy. Based on these findings, IHP was diagnosed.
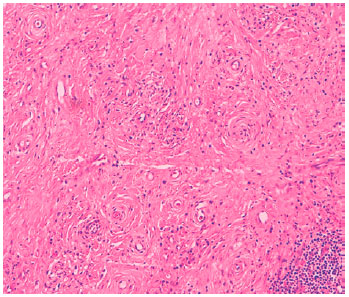
Biopsies of the nasal polyps were performed. Pathological findings revealed characteristics typical of EAF (Figure 2). No IgG deposits were visible on immunofluoroscopy.
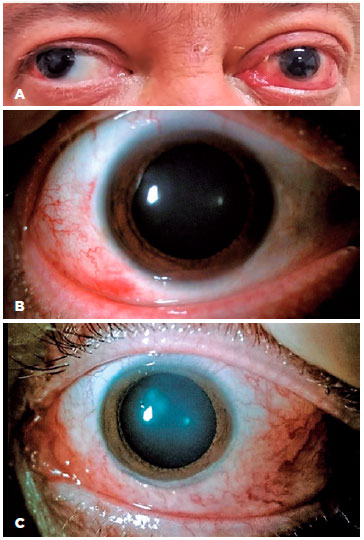
Treatment was started with bolus steroids and intravenous cyclophosphamide (1000 mg), but the patient reported progressive loss of vision in the left eye. BCVA was 1.0 in the right eye, and there was light perception in the left eye, which had a Marcus Gunn pupil and marked limitation of motility at all gaze positions, except abduction. This limitation was particularly apparent during adduction. These signs were consistent with those of complete paralysis of the left third cranial nerve (Figure 3A). The anterior pole of the right eye presented slight chemosis and conjunctival hyperemia (Figure 3B). Furthermore, the left eye presented proptosis with intense conjunctival chemosis. Anisocoria was accompanied by moderate mydriasis of the left pupil (Figure 3C).
In view of the unfavorable developments, we decided to start methotrexate administration with two doses of rituximab IV (1000 mg) at an interval of 2 weeks.
Ten days after the first rituximab administration, ocular motility almost returned to normal (Figure 4A). The anterior pole of the right eye was normal (Figure 4B), and chemosis and proptosis in the left had significantly improved (Figure 4C). However, BCVA of the left eye showed no improvement; the Marcus Gunn pupil and anisocoria persisted in the left eye (Figure 4B and C). The patient was discharged, with a treatment regimen of prednisone (50 mg/day) and methotrexate (20 mg/week). After 2 months, the patient's condition remained stable, with prednisone dose reduced to 15 mg/day.
DISCUSSION
IHP is characterized by focal or diffuse thickening of the dura, with unknown etiology. The diagnosis is based on exclusion of various infectious, autoimmune, and neoplastic infiltration diseases, which provoke similar effects. Accordingly, when clinical and imaging results are compatible, a broad range study should be conducted to rule out any underlying pathological causes for the condition(1-9).
IHP has recently been associated with IgG4-RDs(2-5,13). It has been postulated that IgG4-RDs may account for a substantial subset of patients who were previously classified as idiopathic. The definitive diagnosis of IgG4-RD requires histological confirmation; however, in this case, the patient refused to undergo meningeal biopsy. EAF is a rare condition which is usually classified as a type of IgG4-RD(10,13). The present case did not present typical histopathological signs of IgG4-RD in the nasal polyps biopsy. Moreover, serum IgG4 levels were normal. Therefore, we cannot consider this case to be associated with IgG4. To the best of our knowledge, this is the first report of IHP associated with EAF.
Headache is the most common and almost universal symptom of IHP. Any cranial nerve may be affected, but the oculomotor and optic nerves are more commonly involved(1-3,6,7,9). The resulting visual impairment can range from slight decrease in visual acuity to amaurosis(1-4). In our case, the signs were compatible with complete paralysis of the left third cranial nerve, but the proptosis, optic neuropathy, ocular motility, and MRI findings indicated orbital infiltration instead of isolated third nerve palsy related to pachymeningitis. Treatment with rituximab did not improve BCVA of the left eye, probably due to irreversible ischemic damage to the optic nerve. Although the anterior pole may also be affected by proptosis, hyperemia, and chemosis, as reported in this case, the occurrence of this event is extremely rare, and we found only one previous report in the literature(1).
MRI was fundamental for the diagnosis; it revealed areas of dural thickening. The lesions were enhanced due to contrast administration(1-4,7,9). MRI can also be useful for follow-ups(1,2). CSF usually presents with normal opening pressure, elevated protein levels, and increased cellularity at the expense of lymphocytes(1,2,6,9). In addition, ESR and CRP levels are often elevated(1,2,6,9). In our patient, MRI revealed typical IHP findings. Also, ESR and CRP levels and CSF evaluation findings were all consistent with the diagnosis of IHP.
Steroids are the first-line treatment for IHP, and the use of immunosuppressants is a good option in resistant cases(1,3,7,9). Our patient was treated with rituximab due to the severity of the condition, partial response to steroids, and need to prevent a similar situation occurring in the right eye. The patient's prognosis was excellent. We only found three previous reports, wherein rituximab was used to treat IHP and showed favorable results(2,3).
REFERENCES
1. Zhao M, Geng T, Qiao L, Shi J, Xie J, Huang F, et al. Idiopathic hypertrophic pachymeningitis: clinical, laboratory and neuroradiologic features in China. J Clin Neurosci. 2014;21(7):1127-32.
2. Wallace ZS, Carruthers MN, Khosroshahi A, Carruthers R, Shinagare S, Stemmer-Rachamimov A, et al. IgG4-related disease and hypertrophic pachymeningitis. Medicine. 2013;92(4):206-16.
3. Popkirov S, Kowalski T, Schlegel U, Skodda S. Immunoglobulin- G4-related hypertrophic pachymeningitis with antineutrophil cytoplasmatic antibodies effectively treated with rituximab. J Clin Neurosci. 2015;22(6):1038-40.
4. Ramirez L, D’Auria A, Popalzai A, Sanossian N. Bilateral vision loss secondary to pachymeningitis in a patient with IgG4-related disease. Front Neurol. 2014;5:192. doi: 10.3389/fneur.2014.00192.
5. Lu Z, Tongxi L, Jie L, Yujuan J, Wei J, Xia L, et al. IgG4-related spinal pachymeningitis. Clin Rheumatol. 2016;35(6):1549-53. doi: 10.1007/ s10067-015-3104-x.
6. Zhu R, He Z, Ren Y. Idiopathic hypertrophic craniocervical pachymeningitis. Eur Spine J. 2015;24(4):633-5.
7. Reggio E, Giliberto C, Sortino G, Zappia M. A case of headache and idiopathic hypertrophic cranial pachymeningitis drastically improved after CSF tapping. Headache. 2016;56(1):176-7.
8. Abhilash K, Minimol K. Idiopathic hypertrophic pachymeningitis. Int J Res Med Sci. 2013;1(4):599-600.
9. Riku S, Kato S. Idiopathic hypertrophic pachymeningitis. Neuropathology. 2003;23(4):335-44.
10. Deshpande V, Khosroshahi A, Nielsen GP, Hamilos DL, Stone JH. Eosinophilic angiocentric fibrosis is a form of IgG4-related systemic disease. Am J Surg Pathol. 2011;35(5):701-6.
11. Li Y, Liu H, Han D, Zang H, Wang T, Hu B. Eosinophilic angiocentric fibrosis of the nasal septum. Case Rep Otolaryngol. 2013;2013: 267285. doi:10.1155/2013/267285
12. Lloyd AP, Benzimra JD, Warfield AT, Prasad BT, Matthews TD, Ahmed SK. Optic neuropathy secondary to eosinophilic angiocentric fibrosis. J Neuroophthalmol. 2015;35(1):45-7.
13. Khosroshahi A, Deshpande V, Stone JH. The clinical and pathological features of IgG4-related disease. Curr Rheumatol Rep. 2011; 13(6):473-81.
Submitted for publication:
November 29, 2016.
Accepted for publication:
March 16, 2018.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose