

Luis Filipe Nakayama; Vinicius Campos Bergamo; Leticia Sant'ana Cardoso Silva; Nilva Simeren Bueno Moraes
DOI: 10.5935/0004-2749.20180048
ABSTRACT
Here we report the case of a 78-year-old male patient with a 2-day history of low visual acuity and fundus and who was diagnosed with central retinal artery occlusion. In addition, the patient had an allergy to fluorescein. A fundus examination of the left eye found a pink optic disc with blurred margins, diffuse pallor in the retina with arterial attenuation, and a normal band of the retinal area in the macular region. Optical coherence tomography revealed increased thickness of the inner retina. Optical coherence tomography angiography (OCT-A) revealed a decreased flow signal in the superficial layers, with reduced flow signal in the choriocapillaris. OCT-A is a valuable alternative during the follow-up period in patients with central retinal artery occlusion, particularly in those with an allergy to contrast agents. The use of this as a non-invasive examination can improve the prognosis of patients and future studies investigating the treatment of central retinal artery occlusion.
Keywords: Optical coherence tomography; Retinal artery occlusion
RESUMO
Paciente de 78 anos do sexo masculino com história de dois dias de baixa acuidade visual em olho esquerdo e exame fundoscópico sugestivo de oclusão da artéria retiniana, além de história de alergia a fluoresceína sódica. Em exame de fundoscopia de olho esquerdo pode ser observado disco óptico róseo, mal delimitado, palidez difusa da retina, com banda em área macular apresentando cor rósea preservada. A tomografia de coerência óptica apresentava aumento de espessura de retina interna em áreas de palidez e espessura e camadas preservadas em área poupada. A tomografia de coerência óptica-A mostrou sinal diminuído em camadas superficiais, com sinal de fluxo diminuído em coriocapilar. A tomografia de coerência óptica-A é uma alternativa válida para seguimento de pacientes com oclusão da artéria retiniana, em casos de alergia ao contraste ou contra indicação ao exame. O exame é não invasivo e pode melhorar não somente a avaliação dos pacientes nos dias de hoje como aumenta possibilidades em futuros estudos e tratamentos da oclusão da artéria retiniana.
Descritores: Tomografia de coerência óptica; Oclusão da artéria retiniana
INTRODUCTION
Non-arteritic central retinal artery occlusion (CRAO) is a rare condition and is estimated to occur in 1 in 100,000 people(1). It presents as subtle, complete, severe, and non-dolorous vision loss. In the acute phase of CRAO, an ophthalmological examination reveals a pale and edematous retina corresponding to non-perfused areas. These findings are secondary to an ischemia-induced increase in nerve fiber and ganglion retinal layer thickness(2).
The causes of CRAO are related to some conditions, and its prognosis is usually poor. The most common CRAO etiology is secondary to arteriosclerosis emboli, and its associated factors include systemic arterial hypertension, diabetes, smoking, and a previous cerebral vascular event(3). One prospective study from Hayreh in 2005 evaluated 260 eyes and concluded that 80% of patients with CRAO ended with 0.1 or worse visual acuity(3). Irreversible retinal damage occurs 240 min after the occlusive event(4), with poor prognosis ensuing after that. The cilioretinal artery, a branch of the short posterior ciliary artery, is present in approximately 49.5% of the general population, and it is responsible for supplying blood to the inner retina between the optic nerve and the macula in 14.6% of population(5). CRAO in patients with a patent cilioretinal artery yields a better visual acuity prognosis of 0.5 or better.
Current non-invasive acute treatments include reducing the intraocular pressure or ocular massage, while invasive therapies are often thrombolytic. These techniques are described as useful within 6 h after the occlusive event(1). Thus, a criteria-based diagnosis and improved follow-up are essential to evaluate and identify possible treatments.
The diagnosis of CRAO is made following a review of the patient's full clinical history and an ophthalmological fundus examination. Moreover, vascular and cardiology examinations can provide additional diagnostic insight into the progress and etiology. Ancillary examiations such as a color fundus photograph and fluorescein angiography (FA) may also be helpful during the initial diagnosis and the follow-up phase. FA uses fluorescein as a dye to evaluate retinal perfusion and to identify the presence or absence of a cilioretinal artery (suspected by a clinical and fundus examination). Nevertheless, fluorescein is not recommended in patients with an allergy or in those with clinical conditions such as kidney failure, pregnancy, moderate-severe asthma, and significant cardiac disease(5,6).
Optical coherence tomography (OCT) angiography (OCT-A) uses optical interferometry technology and relies on differences in motion captured between the neurosensory retina (static) and retinal vessels (dynamic). With OCT-A, it is possible to evaluate both retinal and choroid layers and establish a stratified vascular density map of the retina and choroid(7).
This non-invasive examination allows the evaluation of retinal vascularity without using any dye/contrast agent. Furthermore, OCT-A is typically performed in a multimodal platform that renders a color fundus photograph and OCT image in the same capture. Thus, it can be a useful tool to help in diagnosing and subsequently monitoring patients with CRAO.
CASE REPORT
We report the case of a 78-year-old Caucasian male who was born and raised in São Paulo, SP - Brazil. The patient presented to an emergency room in Hospital São Paulo (EPM-UNIFESP, São Paulo-SP, Brazil) with the chief complaint of subtle visual loss in bands in the left eye for the past 2 days. He reported profound visual loss and denied any history of trauma, pain, or associated factors.
The patient's medical history included systemic arterial hypertension, type-2 diabetes mellitus, and a fluorescein allergy. He denied any family history of ocular diseases.
At his initial presentation, his arterial blood pressure was 140/80 mmHg. The ophthalmological examination revealed that his best-corrected visual acuity was 20/20 in the right eye and 20/25 in the left eye. His slit-lamp exam showed a deep anterior chamber, transparent cornea and conjunctiva, and phakic intraocular lenses without cataracts and without anterior chamber reaction in the right and left eyes. He had no changes in his slit-lamp exam and presented with an intraocular pressure of 16 mmHg in the right eye and 14 mmHg in the left eye (as measured with a Goldmann tonometer).
A fundus examination of the right eye showed a pink optic disc with sharp margins, a cup-disc ratio of 0.5, increased venous and arterial tortuosity with broadening of the light reflex in the arteries, diffuse retinal pigment epithelium rarefaction, and an attached retina (Figure 1; left picture).
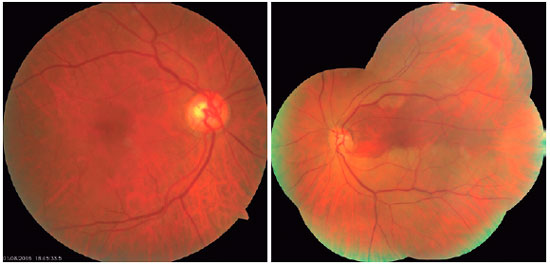
In the left eye, the fundus examination showed a pink optic disc with blurred margins and increased venous tortuosity with arterial narrowing. Further, we observed a diffuse pale retina, sparing of the superior band of the macular area, diffuse retinal pigment epithelium rarefaction, and an attached retina (Figure 1; right picture).
The initial diagnostic hypothesis was CRAO with a patent cilioretinal artery in the left eye and hypertensive retinopathy in both eyes (Grade II in the Keith-Wagener-Barker classification).
Ancillary examinations performed at the emergency room included an electrocardiogram assessment, Doppler carotid ultrasound, and comprehensive blood examinations. An electrocardiogram showed a previously missed supraventricular arrhythmia (not yet diagnosed). Doppler carotid ultrasound showed multiple heterogeneous plaques within the common carotid artery and anterior and posterior walls of the carotid bulb on the left and right side. The examination did not reveal stenosis that impacted hemodynamics but showed vulnerable plaques at the left carotid bulb. Complete blood count, erythrocyte sedimentation rate, C-reactive protein levels, and renal and hepatic function were normal.
The patient indicated that he had an allergy to contrast agents, with a history of anaphylaxis; thus, our clinical recommendation was to avoid using any contrast agent.
The ophthalmological ancillary examination, color fundus photography, OCT, and OCT-A, were performed by TOPCON® Triton (Topcon Corporation, Tokyo, Japan). OCT of the macular region of the right eye showed normal retinal thickness and structures in all layers, with the foveal depression preserved. Choroidal layers presented usual thickness. OCT of the left eye showed increased thickness of the internal retinal layers in pale areas that was compatible with CRAO, sparing of the band in the macular area, that may correspond to the cilioretinal perfusion region (Figure 2). Choroidal layers also had usual thickness.
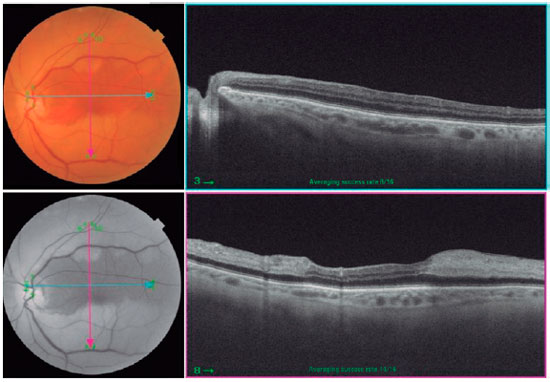
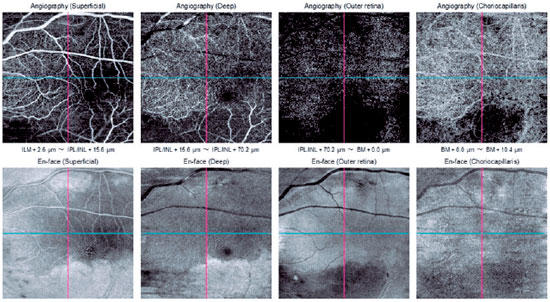
OCT-A of the right eye showed signs of normal flow and vascularization in all slabs. OCT-A of the left eye showed signs of a decrease in the superficial retinal plexus slab, except in a well-delimited band of the macular area that extended from the optic disc to the temporal macula. The same decreased blood flow was found in the deep retinal plexus slab and in the outer retinal slab. Signs of decreased flow in the choroidal slab were also found (Figure 3).
The patient has since been followed-up by the ophthalmology, vascular, and cardiology departments.
After 6 months, he had the same visual acuity but suffered an ischemic encephalic event during the follow-up period.
DISCUSSION
Although central retinal artery occlusion is a rare condition in the general population, it is relatively common in elderly and hypertensive patients due to the associated morbidity(1,3). The most important means to prevent CRAO are treating associated factors, such as hypertension and diabetes, and lifestyle risk factors such as smoking(1). However, after the condition is diagnosed, it is essential to detect the mechanism of occlusion with cardiologic and vascular examinations(1). Furthermore, other ancillary examinations can be useful for determining the presence and severity of changes in vascular flow.
In our case, the patient presented with classic symptoms of CRAO with cilioretinal sparing, which is responsible for macular vascularization and visual acuity. Although classical symptoms were observed at the initial ophthalmological examination, the patient presented only two days after the occlusive event, which made acute treatment impossible(3). In addition to clinical history taking and an ophthalmological fundus examination that diagnosed the condition, FA can be useful as an ancillary examination. In this case, the recommendation to avoid the use of contrast agents precluded the use of this examination; therefore, other ways to analyze blood flow can be useful in similar situations(5,6).
OCT-A has proven to be a valuable alternative examination, in this case, to follow-up ischemic regions with restrictions in the visual field, decreased visual acuity, and possible retinal neovascularization focus.
In the present case, OCT-A showed areas of decreased blood flow within the superficial retinal plexus outside an area that may correspond to the cilioretinal artery. Decreased blood flow was also noted in choroidal slabs, but this could be an artifact from the increased thickness of the inner retinal layers as originally suspected in the fundus examination and confirmed in B-scans in OCT. Artifacts from inner retinal edema can also decrease superficial retinal sign flow, but with probably minor impact.
Alterations in perfusion may be discerned from artifacts in OCT and OCT with a follow-up and resolution of retinal edema.
The costs of the examinations do not justify their use as the primary means of diagnosis as a patient's clinical history and fundus examination itself can yield a diagnosis without the need for expensive testing. The possibility of using OCT-A to assess and follow changes in retinal blood flow is promising, and its use as a non-invasive tool can serve as a useful tool not only during the follow-up period but also in clinical and treatment research trials.
OCT-A is a valuable diagnostic alternative that can be used during the follow-up period in patients with CRAO, particularly in those with an allergy to contrast agents. The use of this non-invasive examination can improve the prognosis of patients and future studies investigating the treatment of CRAO.
REFERENCES
1. Varma DD, Cugati S, Lee AW, Chen CS. A review of central retinal artery occlusion: clinical presentation and management. Eye (Lond) 2013;27(6):688-97.
2. Brown GC, Magargal LE, Sergott R. Acute obstruction of the retinal and choroidal circulations. Ophthalmology. 1986;93(11):1373-82.
3. Hayreh SS, Zimmerman MB. Central retinal artery occlusion: visual outcome. Am J Ophthalmol. 2005;140(3):376-91.
4. Hayreh SS, Zimmerman MB, Kimura A, Sanon A. Central retinal artery occlusion. Retinal survival time. Exp Eye Res. 2004;78(3): 723-36.
5. Justice J Jr, Lehmann RP. Cilioretinal arteries. A study based on review of stereo fundus photographs and fluorescein angiographic findings. Arch Ophthalmol. 1976;94(8):1355-8.
6. Spaide RF, Klancnik JM Jr, Cooney MJ. Retinal vascular layers imaged by fluorescein angiography and optical coherence tomography angiography. JAMA Ophthalmol. 2015;133(1):45-50.
7. Lavinsky F, Lavinsky D. Novel perspectives on swept-source optical coherence tomography. Int J Retina Vitreous. 2016;2:25.
Submitted for publication:
November 17, 2017.
Accepted for publication:
February 8, 2018.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose