

Edmilson Gigante; Rodrigo Abdalla Romão; Fátima de Jesus Passador Valério
DOI: 10.5935/0004-2749.20180046
ABSTRACT
Purpose: To conduct a 10-year follow-up on the surgical correction of large-angle esotropia using monocular surgery, verifying surgical stability over time in both adults and children, and investigating the presence of consecutive exotropia among reviewed patients.
Methods: The angles of deviation in primary position were measured using prism cover testing in patients with good vision in both eyes and the Krimsky method in those with severe amblyopia. Among the 46 patients who underwent surgery, 40 were evaluated 10 years post-surgery. Student's t-test and McNemar's test were used for statistical analyses.
Results: No significant differences in the angles of deviation in primary position were found between measurements taken 6 months and 10 years post-surgery (p=0.922), as well as between children and adults (p=0.767). Among the 40 reviewed patients, only five presented with exotropia, all of which were small (the largest being XT 15Δ). Therefore, large consecutive exotropia over time was not observed.
Conclusion: Our results suggest that monocular surgery to correct large-angle esotropia using large medial rectus recessions and broad lateral rectus resections was viable and safe in both adults and children over short and long terms.
Keywords: Strabismus; Esotropia; Exotropia; Oculomotor muscles; Refractive errors
RESUMO
Objetivo: Conduzir um acompanhamento de 10 anos de correção cirúrgica de esotropias de grande ângulo com cirurgia monocular, verificando a estabilidade cirúrgica ao longo do tempo em adultos e crianças, investigando a presença de exotropias consecutivas entre os pacientes revisados.
Métodos: Os ângulos de desvio em posição primária foram medidos usando teste de cobertura prismática em pacientes com boa visão em ambos os olhos e o método de Krimsky naqueles com ambliopia severa. Entre os 46 pacientes operados, 40 foram avaliados 10 anos após a cirurgia. O teste t-Student e o de McNemar foram usados para análises estatísticas.
Resultados: Não foram encontradas diferenças significativas nos ângulos de desvio em posição primária entre as medidas realizadas 6 meses e 10 anos pós-operatórios (p=0,922, assim como entre crianças e adultos (p=0,767). Entre os 40 pacientes revisados, apenas cinco apresentaram exotropias, todas pequenas (sendo o maior XT 15Δ). Portanto grandes exotropias consecutivas ao longo do tempo não foram observadas.
Conclusão: Nossos resultados sugerem que a cirurgia monocular para corrigir a esotropias de grande ângulo usando amplos recuos do reto medial e grandes ressecções do reto lateral foi viável e segura tanto em adultos quanto em crianças em curto como a longo prazo.
Descritores: Estrabismo; Esotropia; Exotropia; Músculos oculomotores; Erros de refração
INTRODUCTION
As demonstrated in several studies, large-angle esotropia has been generally corrected through bilateral surgery of the four horizontal muscles (or at least three of them)(1-4). This procedure had become commonplace among academic circles after the 1922 study by Jameson(5) demonstrated a new surgical technique, i.e., medial rectus recession with scleral suturing a few millimeters from the muscle’s original insertion. This technique was of substantial importance given that it made strabismus surgeries more predictable compared to primitive surgeries, which simply excised the muscle (myotomy)(6,7) or tendon (tenotomy)(8-10) without suturing. However, the author's initial challenge was to determine exactly how many millimeters of muscle recession was needed in each case, as well as the maximum possible recession, considering the absence of any previous parameters in the literature. Given that the distance from the insertion of the medial rectus to the equator of the eye was already known at the time to be approximately 5-6 mm, Jameson considered it more prudent to make a recession of 5 mm at most. Thus, the muscle would not be inserted beyond the equator, which could weaken it to the point where secondary exotropia could develop over time as had already been observed in cases involving myotomy and tenotomy.
Therefore, 5 mm had been established as the maximum medial rectus recession to be used in esotropia surgeries at the time. Although monocular surgeries were sufficient for correcting small and medium esotropia cases, large-angle esotropia could be only corrected through bilateral surgeries. This fact was accepted by the academic community and became a rule (practically dogma) that was followed by all ophthalmologists of the time - a rule that continues to be followed today to a certain extent(11-13). This rule has remained prevalent perhaps because of the expectation that medial rectus recessions larger than 6 mm would cause consecutive long-term exotropias and limited short-term motility in the operated eye, thereby impairing its rotation.
The first author to go against this rule was Rodríguez-Vásquez(14), who, in 1974, proposed a new surgical technique to correct the syndrome of bilateral limitation of abduction (also known as Ciancia's syndrome) by performing large medial rectus recessions (6-9 mm) in both eyes depending on the magnitude of the ocular deviation. Other authors(2-4,15-17) had been able to confirm Rodriguez-Vasquez's surgery in practice. However, despite its status as a groundbreaking study, the former rule regarding binocular surgery for correcting large-angle esotropia had been maintained.
Recently, however, a number of new studies have proposed monocular surgery for the correction of large-angle esotropia using large recessions of the medial rectus(18-22). Among such research, the study by Gigante and Bicas(18) stands out. Their study analyzed 46 patients who had undergone surgery at the University Hospital of UNOESTE School of Medicine in Presidente Prudente, São Paulo, Brazil from 2000 to 2006. All of the patients, which included children and adults of both genders with and without amblyopia, presented with esotropia of 50Δ or more and relatively comitant deviations. Surgeries were performed using large recessions of the medial rectus (6-10 mm) and broad resections of the lateral rectus (8-10 mm) in the non-fixating eye (which generally had worse vision). The eye exhibiting better vision was always spared. General anesthesia was used during surgery, while the surgical technique employed was that normally used during resection and recession with non-readjustable suturing.
Measurements of the angle of deviation in primary position (PP) obtained by the authors were comparable with those in the literature. Moreover, no significant differences had been observed between children and adults or between cases with and without amblyopia. However, lateroversion measurements were not consistent with the substantial limitations reported in the literature. Nonetheless, good motility of the operated eye was observed with only slight limitation in adduction and none in abduction.
Given the innovative nature of the original study, we found it imperative to conduct a follow-up study on the operated patients included therein. This study had been conducted between 2013 and 2014, approximately 10 years post-surgery. The purpose of this study was to describe long-term (10 years) surgical outcomes among patients who underwent monocular surgery to correct large-angle esotropias. Accordingly, the current study compares the angles of deviation in PP measured 6 months and 10 years post-surgery and outcomes between children and adults (defined based on their ages at the time of surgery) 10 years later while determining whether the presence of exotropia was a consequence of large medial rectus recession 10 years post-surgery.
METHODS
A total of 46 patients underwent surgery in the study by Gigante and Bicas(18). The aforementioned study included patients with esotropia of 50Δ or more and excluded those with muscular paralysis, high myopia, Ciancia syndrome, dissociated vertical divergence, accommodative esotropias, large vertical deviations associated with esotropia, alphabetic syndromes, and previous surgeries in either eye. Of the 46 patients, 41 regularly attended their follow-up visits until 6 months post-surgery. Among the 41 patients, 36 were included in the study. Their characteristics at the time of surgery, surgical treatment, and surgery dates are presented in table 1.
Of the five patients not included in this follow-up study, ICS had already died, FCM was living in Portugal, and DBB had been incarcerated and has had no contact with his family. The other two had not been found.
Five patients did not complete their 6 months of follow-up visits. Among them, four were found and evaluated, revealing the following angles of deviation in PP: AMS, ET 4Δ; RPS, ET 20Δ; OJS, ET 8Δ; and PHCM, ET 18Δ. The aforementioned patients were excluded from statistical analysis given the unavailability of results for their 6-month follow-up. However, we consider it important to cite them in order to show that none of them experienced consecutive exotropia.
The methods used to measure the angles of deviation in PP included prism cover test in patients with no or moderate amblyopia and the Krimsky method in cases with severe amblyopia. The angle of deviation used in the tables was calculated with the patient looking at a distant set-point using his or her preferred eye (i.e., the eye not operated on) and his or her best possible optical correction.
Although lateroversion angles of deviation were not measured, all of the patients were photographed in these positions (dextro and levoversion), subsequently showing maintenance of motility in the operated eyes 10 years post-surgery.
Evaluation criteria were similar to those used in the original study: the outcome was considered good when the angle of deviation in PP was up to 15Δ, fair when the angle was between 16Δ and 20Δ, and poor when the angle was above 20Δ.
RESULTS
Measurements of the angle of deviation in PP 6 months post-surgery with the patient fixating using the unoperated eye
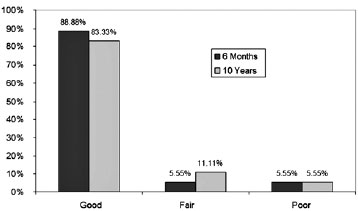
Surgical outcomes of the 36 patients included in this study are presented in table 1. The mean [standard deviation (SD)] of the angles of deviation 6 months post-surgery was 9.89Δ (6.30). As shown in figure 1, 32 patients (88.88%) experienced good outcomes, 2 (5.55%) experienced fair outcomes, and 2 (5.55%) experienced poor outcomes. Table 1 also shows the measurements of angles of deviation in lateroversion 6 months post-surgery, presenting them according to abduction and adduction of the operated eye. These results demonstrated preservation of motility with good amplitude in most of the operated eyes, suggesting no significant limitation in ocular rotation (see Figures 2, 3, and 4 for case examples).



Measurements of the angle of deviation in PP 10 years post-surgery with the patient fixating using the unoperated eye
Surgical outcomes of the 36 patients included in the 10-year post-operative follow-up are presented in table 1. The mean (SD) of the angles of deviation 10 years post-surgery was 10.00Δ (7.61). As shown in figure 1, 30 patients (83.33%) experienced good outcomes, 4 (11.11%) experienced fair outcomes, and two (5.55%) experienced poor outcomes (see Figures 2, 3, and 4 for case examples).
Comparison of outcomes 6 months and 10 years post-surgery measured in PP
Table 1 compares the outcomes 6 months and 10 years post-surgery.
A bar graph was also used to describe both groups as shown in Figure 1. Using Student's paired t-test at a significance level of 0.05 to compare the angles of deviation 6 months and 10 years post-surgery (Table 1), we observed no statistically significant differences between both studied groups [mean 6 m (SD)=9.89Δ (6.30); mean 10y (SD) 10.00Δ (7.61); p=0.922]. This result reflects the stability of surgical outcomes over time (10 years).
To supplement our study, we also determined whether significant qualitative differences existed in the proportion of patients classified as experiencing good, fair, or poor surgical outcomes using McNemar’s test (Figure 1). Accordingly, no statistically significant differences were observed among the groups (p=0.283).
We also measured the amount of correction 6 months and 10 years after surgery. The pre-surgical mean (SD) angle of deviation was 66.41Δ (12.59), while the mean (SD) amount of correction 6 months and 10 years after surgery was 57.63Δ (11.62) and 58.47Δ (14.51), respectively. No statistically significant differences were observed between the mean amount of correction 6 months and 10 years post-surgery (p=0.551).
Comparison of the angles of deviation in PP between children and adults 10 years post-surgery
For this analysis, children were defined as patients up to 16 years of age at the time of surgery, while adults were defined as those older than 16 years. Thereafter, developments within both groups 10 years post-surgery were compared. Of the 36 patients, 18 (50%) were children and 18 (50%) were adults.
First, only children were analyzed. The mean (SD) angle of deviation at the 6th postoperative month [9.83Δ (7.16)] was compared to that 10 years post-surgery [11.39Δ (9.41)] using Student's paired t-test (p=0.05). Despite the relatively small sample size (18 patients), statistically significant differences were not found between both groups (p=0.283). In other words, surgical outcomes among children remained stable over the 10-year postoperative period.
To compare outcomes between children and adults, we considered the mean absolute differences in the angles of deviation 6 months and 10 years post-surgery. The mean values for adults and children were found to be 6.0Δ and 6.56Δ, respectively. Using Student's unpaired t-test (p=0.05) for this analysis, we found no statistically significant differences between both groups (p=0.763), which suggests that monocular surgery to correct large-angle esotropia can be used safely in both children and adults.
Measurements of the angles of deviation in PP among patients with consecutive exotropia 10 years post-surgery
An analysis of Table 1 shows that during the 10-year postoperative follow-up, only 5 of the 36 patients presented consecutive exotropia with the following outcomes: JRB, XT4Δ; TBG, XT10Δ; PHFB, XT15Δ; TOL, XT4Δ; and JCAP, XT4Δ. These were all clear cases of slight exotropia and were considered good outcomes in the evaluation criteria used in this study. No cases of large exotropia were found as was expected based on the literature and considering the large medial rectus recessions used in majority of the patients.
We also note the importance of mentioning the four patients who did not receive follow-up care 6 months post-surgery (for this reason, they were not included during analysis) but were found and included in this study. The aforementioned patients presented with the following angles of deviation in PP: AMS, ET4Δ; RPS, ET20Δ; OJS, ET8Δ; and PHCM, ET18Δ. As shown in the data, no cases of consecutive exotropia were observed among these four patients. Therefore, out of the 40 patients actually included in this study, only five were found to have developed consecutive exotropia, all of which included small angles of deviation in PP.
DISCUSSION
Until now, two main orthodox conceptions have discouraged the performance of studies evaluating monocular surgery with large medial rectus recession (up to 10 mm). The first conception suggested that the operated eye would experience substantial postoperative lateral motility limitations and would essentially be “frozen” in PP(11,12,23). Subsequently, the second conception suggested that the operated eye would begin to move outward in the long term due to large medial rectus recessions, likely leading to consecutive exotropia, particularly in children(5,10). The first conception was dispelled by the authors of the original study through measurements of lateral angles of deviation, as well as postoperative photographs and videos, which demonstrated good motility in the operated eye(18). In the present 10-year follow-up of the study, new lateral photographs of all patients had been taken, showing preservation of motility in the operated eyes. The second conception was the motivation for this 10-year follow-up with the following three findings demonstrating the weakness of this theoretical conception.
1) Angles of deviation in PP: Table 1 shows the angles of deviation of the 36 patients included in the present study, which were measured 6 months and 10 years post-surgery. Accordingly, statistical comparisons demonstrated no significant differences between both groups, thus reflecting the stability of these deviations over time. In other words, our results suggest that monocular surgery to correct large-angle esotropia is viable over short and long terms.
2) Analysis of surgical outcomes in children: Statistical analysis was used to compare outcomes among children 6 months and 10 years post-surgery. We also compared outcomes between the children and adults 10 years post-surgery. Once again, our analysis revealed no statistically significant differences in outcomes between children and adults. In other words, our results suggest that monocular surgery to correct large-angle esotropia displayed long-term safety in both children and adults.
3) Consecutive exotropia: The main criticism of the study reviewed herein was that because of the large medial rectus recession, the tendency would be for patients to develop consecutive exotropia over time, which would likely be large(5,10). However, the current 10-year postoperative follow-up suggested otherwise. Of the 40 patients studied (four of whom were unable comply with 6-month postoperative follow-up), only five developed exotropia. One patient presented with an exotropia of 15Δ, another presented with an exotropia of 10Δ, and three patients presented with an exotropia of 4Δ. In other words, expected cases of large exotropia based on the theoretical interpretation of this new surgical technique had not been observed. It is also worth noting that among the five patients who developed exotropia 10 years after surgery, two already had exotropia 6 months post-surgery (patients TOL and PHFB). In other words, only three patients had developed esotropia 6 months post-surgery, subsequently becoming exotropic 10 years post-surgery. It should also be emphasized that two patients had developed exotropia 6 months post-surgery, subsequently becoming esotropic 10 years post-surgery (patients JS and SDS) - a completely unexpected outcome based on theory. What actually occurred, as suggested by our results, was that a large majority of patients included in the follow-up had developed esotropia 6 months post-surgery and remained esotropic 10 years post-surgery.
CONCLUSION
The results obtained in this follow-up study satisfied all three objectives established. The angles of deviation in PP did not significantly differ 6 months and 10 years post-surgery; no significant differences in outcomes between children and adults had been found; and cases of large consecutive exotropia, which were theoretically expected as a consequence of large medial rectus recessions, had not been found 10 years post-surgery. These results therefore suggest that monocular surgery to correct large-angle esotropia using large medial rectus recessions and broad lateral rectus resections is safe and reliable over short and long terms.
REFERENCES
1. Foschini RM, Bicas HE. Cirurgias de músculos retos horizontais: análise de planejamentos e resultados. Arq Bras Oftalmol. 2001; 64(5):523-34.
2. Prieto-Diaz J. Large bilateral medial rectus recession in early esotropia with bilateral limitation of abduction. J Pediatr Ophtalmol Strabismus.1980;17(2):101-5.
3. Szmyd SM, Nelson LB, Calhoun JH, Spratt C. Large bimedial rectus recessions in congenital esotropia. Br J Ophthalmol. 1985; 69(4):271-4.
4. Nelson LB, Calhoun JH, Simon JW, Wilson T, Harley RD. Surgical management of large angle congenital esotropia. Br J Ophthalmol. 1987;71(5):380-3.
5. Jameson PC. Correction of squint by muscle recession with scleral suturing. Trans Am Ophthalmol Soc. 1922;20:166-81.
6. Martins BJ. Dissertação sobre o estrabismo: seguida de algumas observações [tese]. Rio de Janeiro: Faculdade de Medicina do Rio Janeiro, 1845.
7. Mascarenhas, BD. Tratamento cirúrgico do estrabismo funcional [tese]. Rio de Janeiro: Faculdade de Medicina do Rio de Janeiro; 1922.
8. Bulcão JL. Do valor do tratamento cirúrgico na cura do estrabismo [tese]. Porto Alegre: Faculdade de Medicina de Porto Alegre; 1927; p. 36-40.
9. Munoa Roiz JL. Especialidades quirúrgicas: la oftalmología. In: Laín Entralgo P. Historia Universal de la Medicina. Barcelona: Salvat; 1974. Vol. 6, p. 327-36.
10. Von Noorden GK. The history of strabismology. Belgium: JP Wayenborgh; 2002.
11. Pueyo AC. Tratamiento quirurgico. In: Pueyo AC. Estrabismos Y heteroforias. 2a ed. Madrid: Paz Montalvo; 1958. p. 420-1.
12. Hugonnier R, Clayette-Hugonnier S. Surgical indications in concomitant strabismus. In: Hugonnier R, Clayette-Hugonnier S. Strabismus, heterophoria, ocular motor paralysis: clinical ocular muscle imbalance. Saint Louis: The C. Mosby; 1969. p. 637-43.
13. Helveston EM. Diagnostic categories and classification of strabismus. In: Helveston EM. Surgical management of strabismus. 5th ed. Belgium: J.P. Wayenborgh; 2005. p.127.
14. Rodríguez-Vásquez R. Retroinsercion ampla en cirurgia de endotropia alternas. In: Actas dell IV Congresso del Clade. México. 1974.
15. Vroman DT, Hutchinson AK, Saunders RA, Wilson ME. Two-muscle surgery for congenital esotropia: rate of reoperation in patients with small versus large angles of deviation. J AAPOS. 2000; 4(5):267-70.
16. Bayramlar H, Karadag R, Yildirim A, Oçal A, Sari U, Dag Y. Medium-term outcomes of three horizontal muscle surgery in large-angle infantile esotropia. J Pediatr Ophthalmol Strabismus. 2014;51(3):160-4.
17. Weed MC, Di Menna M, Donaghy CL, Triantafilou D, Larson SA. Long-term outcomes of surgical treatment for large-angle esotropia in children. JAAPOS 2016;20(4):e10.
18. Gigante E, Bicas HEA. Cirurgia monocular para esotropias de grande ângulo: um novo paradigma. Arq Bras Oftalmol. 2009;72(1):47-56.
19. Meireles-Teixeira JA, Cunha RP, Mendonça TS. Resultado da correção cirúrgica de esotropias de grande ângulo, em portadores de baixa acuidade visual unilateral. Arq Bras Oftalmol. 2000; 63(5):365-8.
20. Corrêa BA, Bicas HE. Estudo comparativo de cirurgias moleculares para esotropias sob anestesia geral e sob anestesia tópica, com ou sem reajuste. Rev Bras Oftalmol. 1998;57(10):747-55.
21. Ganguly S, Pradhan R. Effect of monocular surgery for large-angle horizontal deviation in adults. Nepal J Ophthalmol. 2011;3(1):27-30.
22. Millán T, de Carvalho KM, Minguini N. Results of monocular surgery under peribulbar anesthesia for large-angle horizontal strabismus. Clinics (São Paulo). 2009;64(4):303-8.
23. Kirby DB. Cirurgia do estrabismo. Rev Bras Oftalmol. 1948;6(2):135-44.
Submitted for publication:
July 3, 2017.
Accepted for publication:
November 16, 2017.
Approved by the following Research Ethics Committee: Universidade do Oeste Paulista (#447.274)
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose