

Marina Gonçalves Monteiro Viturino1; Frederico Castelo Moura1,2
DOI: 10.5935/0004-2749.20180016
ABSTRACT
Recurrent idiopathic neuroretinitis is an inflammatory optic neuropathy characterized by optic nerve edema and macular star, associated with painless and recurrent episodes of visual loss, poor visual prognosis, and visual field defects related to nerve fiber layer injury. The disorder is sometimes mistaken for atypical optic neuritis. However, early diagnosis is important for visual recovery. Long-term immunosuppression has been shown to reduce the rate of recurrence and protect against severe and irreversible vision loss.
Keywords: Retinitis; Optic nerve diseases; Optic disk; Anti-inflammatory agents; Immunosuppression; Recurrence
RESUMO
Neurorretinite recorrente idiopática é uma neuropatia óptica inflamatória caracterizada por edema do nervo óptico e estrela macular associada a episódios recorrentes de perda visual indolor, baixo prognóstico visual e desfeitos de campo visual relacionados a injúria da camada de fibras nervosas. Essa condição pode ser confundida com neurite óptica atípica e seu correto diagnóstico é importante para o prognóstico visual, uma vez que a imunossupressão continua previne episódios recorrentes que podem levar a perda visual severa e irreversível.
Descritores: Retinite; Doenças do nervo óptico; Disco óptico; Anti-inflamatórios; Imunossupressão; Recidiva
INTRODUCTION
Optic neuritis is most commonly observed in women aged 20-50 years. The condition is characterized by acute unilateral visual loss (visual acuity better than 20/200) and ocular pain, followed by visual recovery. Some patients present atypical features, such as severe visual loss (i.e., counting fingers or worse), signs of intraocular inflammation, absence of pain, and failure to recover vision. Neuromyelitis optica, chronic relapsing inflammatory optic neuropathy, and autoimmune optic neuropathy are examples of atypical optic neuritis.
Neuroretinitis is a self-limiting inflammatory optic neuropathy characterized by edema of the optic nerve associated with macular exudate in a star-shaped pattern, absence of recurrence and good visual prognosis. The most likely etiology of neuroretinitis is infection, although no specific etiology can be determined in half the cases of neuroretinitis. A subtype of neuroretinitis, recurrent idiopathic neuroretinitis (RINR), is characterized by recurrent episodes of visual loss and poor visual prognosis(1).
In this paper, we describe a case of RINR and discuss how to distinguish RINR from atypical optic neuritis.
CASE REPORT
A 38-year-old man presented with sudden painless visual loss in the right eye (OD) starting a week before the first consultation. The patient experienced three episodes in OD and one in the left eye (OS) during the preceding 4 years (one per year on average). All episodes were treated with corticosteroid pulse therapy without improvement of visual function. Long-term immunosuppression was not prescribed during these previous episodes.
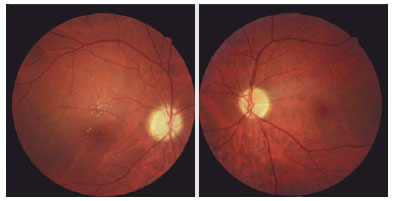
Ophthalmological examination at the time of the actual episode gave results for corrected visual acuity, measured by using an Early Treatment Diabetic Retinopathy Study chart, of hand movement in OD and 20/20 in OS; there was a relative afferent pupillary defect in OD. No changes were observed on anterior segment biomicroscopy in either eye. Ophthalmoscopy revealed the absence of vitreous cellularity (score 0 in the grading of vitreous haze proposed by the Standardization of Uveitis Nomenclature), pallor of both optic nerves, and macular exudate in OD (Figure 1). Color vision was altered, but ocular motility and eyelid function were normal.
Laboratory and cerebrospinal fluid tests were negative for infection (including syphilis, toxoplasmosis, bartonellosis, rubella, herpes, hepatitis, and cytomegalovirus), inflammation (including oligoclonal bands), and metabolic disorders. No anti-aquaporin 4 antibodies were detected on tissue-based indirect immunofluorescence. No brain or optic nerve abnormality was detected on magnetic resonance imaging.
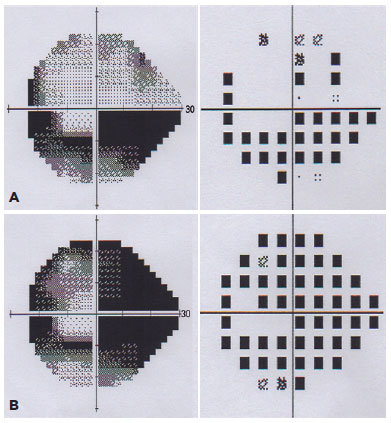
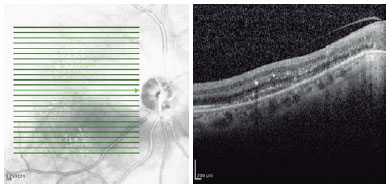
Visual field testing of OS revealed an inferior arcuate defect related to a previous episode of visual loss (Figure 2). The visual field of OD was not tested due to severe visual loss. Optical coherence tomography confirmed the presence of macular exudate in OD (Figure 3).
Having ruled out infectious causes and considering the recurrence of episodes, the presence of macular exudate, and the observed VF defect pattern, a diagnosis of RINR was considered and the patient was started on azathioprine at 200 mg/day.
After 2 years on azathioprine, the patient experienced an episode of bilateral visual loss. Visual acuity was hand movement in OD and 20/20 in OS. On visual field, superior arcuate scotoma was observed in OS (in addition to the previous occurrence of inferior arcuate scotoma), with tubular vision remaining (Figure 2). The patient was treated with corticosteroid pulse therapy followed by a combination of azathioprine (200 mg/day) and prednisone (10 mg/day).
DISCUSSION
Neuroretinitis is an inflammatory optic neuropathy characterized by optic nerve edema, followed 1-2 weeks later by the appearance of macular star. The pathogenesis involves localized inflammation of the optic nerve vessels with increased vascular permeability and consequent leakage of liquid that accumulates in the macular region, with subsequent resorption and deposition of hard exudate. Vascular inflammation is most often associated with infectious diseases (e.g., cat-scratch disease, Lyme disease, and syphilis), but it may also be idiopathic and occasionally involve a viral process(1). Neuroretinitis is not associated with multiple sclerosis despite being classified as an inflammatory optic neuropathy(2).
In most cases, neuroretinitis is a self-limiting disease associated with mild or moderate visual function impairment, absence of ocular pain, and visual recovery. Central scotoma is the most common pattern of visual field defect(3).
Although RINR shares a number of features with classical neuroretinitis (e.g., optic nerve edema, macular exudate in star-shaped pattern, relatively young age at onset, and painless visual loss), visual loss is recurrent and much more severe and visual prognosis is poor(3), suggesting an immune-mediated mechanism. On the other hand, lab testing rarely confirms the presence of systemic disease. In fact, few cases of RINR associated with immune-mediated disorders (e.g., sarcoidosis(4) and ulcerative colitis(5)) have been described.
Our patient presented with recurrent and painless visual loss associated with hard macular exudate. The absence of the typical star-shaped pattern (Figure 1) may be explained by the long time elapsed between the appearance of the exudate and retinal imaging(1).
The visual field pattern is an important distinguishing mark between RINR and classical neuroretinitis. Central scotoma is more common in the latter because of the relationship between visual loss and macular exudate. In the former, however, visual loss is secondary to optic neuropathy associated with primary vasculitis(3). Cecocentral and arcuate scotoma associated with nerve fiber layer injury are therefore more common in RINR.
RINR may be mistaken for atypical optic neuritis (e.g., neuromyelitis optica and chronic relapsing inflammatory optic neuropathy) since both neuromyelitis optica and chronic relapsing inflammatory optic neuropathy feature recurrent, severe, and painless visual loss with poor visual prognosis. Patients may also be misdiagnosed as having nonarteritic anterior ischemic optic neuropathy (NAION) because of the absence of pain, macular exudate, and arcuate defect, which can mimic altitudinal scotoma. However, RINR can be distinguished from NAION by the epidemiological patient profile and recurrence in the same eye.
Treating RINR with corticosteroids during acute attacks is insufficient to revert visual loss(6). The visual function of our patient did not improve with pulse therapy or oral corticosteroids, and the rate of recurrence remained high (one episode per year). Following the example of Purvin et al.(6), we treated our patient with long-term immunosuppression using azathioprine, which eventually reduced the rate of recurrence to 0.5 episodes per year.
RINR should be included in the differential diagnosis of atypical optic neuritis combined with visual loss. Recurrence, poor visual recovery, macular exudate, and nerve fiber-related visual field defects are important clues for early diagnosis(6).
REFERENCES
1. Purvin V, Sundaram S, Kawasaki A. Neuroretinitis: review of the literature and new observations. J Neuroophthalmol. 2011;31(1): 58-68.
2. Parmley VC, Schiffman JS, Maitland CG, Miller NR, Dreyer RF, Hoyt WF. Does neuroretinitis rule out multiple sclerosis? Arch Neurol. 1987;44(10):1045-8.
3. Sundaram SV, Purvin VA, Kawasaki A. Recurrent idiopathic neuroretinitis: natural history and effect of treatment. Clin Exp Ophthalmol. 2010;38(6):591-6.
4. Eggenberger ER. Inflammatory optic neuropathies. Ophthalmol Clin North Am. 2001;14(1):73-82.
5. Shoari M, Katz BJ. Recurrent neuroretinitis in an adolescent with ulcerative colitis. J Neuroophthalmol. 2005;25(4):286-8.
6. Purvin V, Ranson N, Kawasaki A. Idiopathic recurrent neuroretinitis: effects of long-term immunosuppression. Arch Ophthalmol. 2003;121(1):65-7.
Submitted for publication:
January 24, 2017.
Accepted for publication:
November 15, 2017.
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.