

Nelson Chamma Capelanes1; André Vasconcellos Diniz2; Érika Pacheco Magalhães1; Karise de Oliveira Marques3
DOI: 10.5935/0004-2749.20180009
ABSTRACT
Purpose: To compare postoperative changes in retinal nerve fiber layer thickness in patients with macular holes treated with vitrectomy with Brilliant Blue-assisted internal limiting membrane peeling.
Methods: Twenty-two eyes of 20 patients with macular holes were studied. Each eye was selected to undergo Brilliant Blue-assisted internal limiting membrane peeling. The circumferential retinal nerve fiber layer thickness was determined using spectral domain optical coherence tomography preoperatively and 2 months postoperatively. Mean overall and sectoral retinal nerve fiber layer thicknesses were obtained for each patient.
Results: There was no statistically significant difference (p≥0.05) between the pre- and post-treatment measurements in relation to each CFN variable, i.e., on average, pre-treatment measures were the same as post-treatment measures. Furthermore, despite the differences between the pre- and post-treatment measures always being positive (pre-post >0), they are not statistically significant.
Conclusions: This study showed no significant decrease in retinal nerve fiber layer thickness measurements after macular holes surgery, regardless of age or sex.
Keywords: Nerve fibers; Retinal perforations/surgery; Retinal nerve fiber layer thickness; Macular hole
RESUMO
Objetivo: Comparar as alterações pós-operatórias na espessura da camada de fibras nervosas da retina em pacientes com buracos maculares submetidos à vitrectomia via pars-plana associada à remoção de membrana limitante interna.
Métodos: Foram estudados 22 olhos de 20 pacientes consecutivos diagnosticados com buraco macular. Todos os pacientes foram submetidos à vitrectomia via pars-plana e remoção de membrana limitante interna corada com azul brilhante. A espessura da camada de fibras nervosas da retina em região peripapilar foi determinada por tomografia de coerência óptica de domínio espectral antes e 2 meses após a cirurgia. As espessuras totais e espessuras setoriais da camada de fibras nervosas da retina foram obtidas para cada paciente.
Resultados: Os resultados mostram que não existe diferença estatisticamente significativa (p≥0,05) entre as medidas pré e pós-operatórias em relação a cada uma das variáveis.
Conclusão: Este estudo não demonstrou diminuição significativa nas medidas da espessura da camada de fibras nervosas retinianas após a cirurgia de buraco macular, independente da faixa etária ou sexo.
Descritores: Fibras nervosas; Perfurações retinianas/cirurgia, Espessura da camada de fibras nervosas da retina, Buraco macular
INTRODUCTION
Idiopathic macular hole is a controversial genesis retinal defect, primarily involving the foveola. It mainly affects women (67%-91%) between the fifth and seventh decades of life and is bilateral in approximately 3%-27% of cases(1-2).
Internal limiting membrane (ILM) peeling in macular hole surgery has become an important procedure to improve anatomic success and decrease recurrence rates(1-3).
Staining ILM with Brilliant Blue has been a standard technique for their removal around macular hole because of reduced cytotoxicity relative to indocyanine green(1-4).
However, anatomical changes have been observed around the area of peeling, including the retinal nerve fiber layer (RNFL) where nerve fibers are concentrated(1-3).
The development of spectral domain optical coherence tomography (SD-OCT) has made morphological study of different retinal layers possible with a high level of detail(3-8).
RNFL, which is most important for this study, is located between ILM and the ganglion cell layer of the retina, and its thickness can be easily evaluated(9).
Some notable studies have reported RNFL loss after ILM peeling, either as a result of dye-related toxicity, mechanical injury, or increased intraocular pressure (IOP) during vitrectomy(10-12).
Our study aimed to determine if there is a significant nerve fiber loss to justify the visual field defects described in the literature and assess whether macular hole surgery is a risk factor for nerve fiber loss around the optic nerve. We also evaluated the correlation with sex, age, and regions around the nerve with major postoperative changes by evaluating the difference in RNFL thickness before and after macular hole surgery using SD-OCT (Spectralis, Heidelberg Engineering).
METHODS
A retrospective study from SD-OCT analysis was performed for all patients undergoing pars plana vitrectomy with ILM peeling from January 2014 to September 2015. We included all sizes of full-thickness macular holes in this study.
We excluded patients who had undergone retinal surgery or had a previous diagnosis of glaucoma or traumatic macular hole. Eyes with lamellar macular holes were also excluded.
All surgeries were performed by the same surgeon under the same conditions and using the same instruments.
Pars plana 25-gauge vitrectomy using the Alcon Constellation® device was performed. When viewed, the posterior hyaloid was still attached to the optical disc, and this detachment was "manually" induced by active aspiration through a vitrectomy cutter using only the aspiration mode. Brilliant Blue was used to view ILM.
ILM peeling was performed using 23G Alcon ILM forceps to start the ILM peel just central to the lower temporal arcade, creating a tear and then a flap, and the peeling was performed using the same forceps, in an area of ≥ 1 disk diameter around the macular hole. Fluid-air exchange and tamponade with C3F8 gas (perfluoropropane) were performed in all cases.
During the fluid-air exchange, the air pressure was set at 40 mmHg. Next, an exchange of air-gas was performed using 14% perfluoropropane, and the patient was instructed to stay in a prone position for at least 4 days.
Spectralis software was used to evaluate RNFL thickness around the optic nerve head automatically. Circular scans of 1.8 mm radius were performed preoperatively and 60 days postoperatively (Figure 1). The RNFL measurements were checked and confirmed by two different examiners, and there was no need to correct the measures manually in any of the eyes. Preoperative and postoperative measurements were made on the same site using OCT tracking.
The results are expressed as means ± standard deviations (SDs), and the Levene test was used to find the homogeneity of the variances of each studied variable by group. The objective of this test is to verify whether the variances are different between the two groups regarding the variable of interest. In the present study, we decided to assume heterogeneity of the variances in the majority of cases. Thus, choosing to use the values of the t test assuming non-equality of variances contributes to more robust results.
This study was conducted with the approval of the ethics committee of the institution (SOEBRAS) and submitted to Plataforma Brasil for approval.
RESULTS
In total, 22 eyes of 20 patients (6 men and 16 women) were included in the study. The macular hole was closed in all cases after the initial surgery. No intraoperative or postoperative complications, including elevation of IOP, were observed. There was no statistically significant difference (p≥0.05) in pre- and postoperative RNFL measurement in all patients.
There were no sustained increases in IOP and no recorded incidence of postoperative IOP >30 mmHg.
Changes in RNFL thickness from baseline to postoperatively and averages of the absolute values of the RNFL thickness obtained by sectoral analyses are shown in table 1. No statistically significant difference (p≥0.05) was seen between pre- and post-treatment measurements in relation to each RNFL variable, i.e., on an average, the pre-treatment measurements are the same as post-treatment measurements. Further, despite the positive differences between the pre- and post-treatment measurements (pre-post>0), these differences were not statistically significant. As shown in figures 2 and 3, the averages of each of the RNFL variables for pre-treatment are higher than those for post-treatment, but this was not statistically significant (p≥0.05).
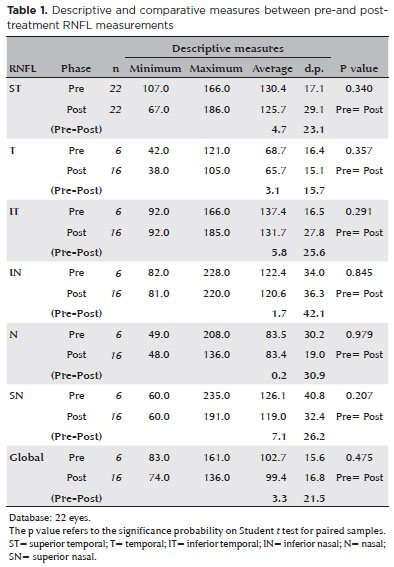
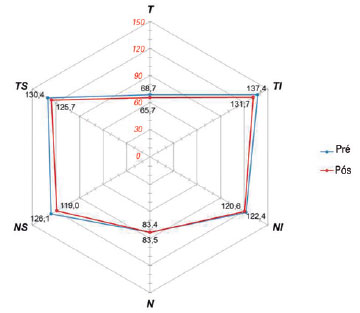
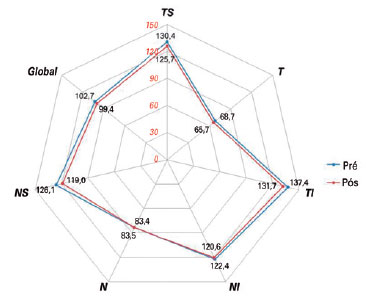
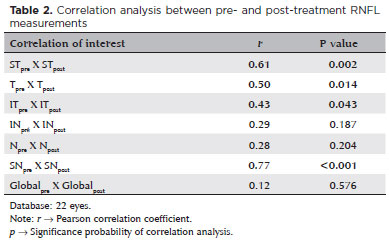
Table 2 shows that statistically significant correlations were observed (p<0.05) with positive correlation (r>0) in four RNFL variables between pre- and post-treatment measurements, with the greatest degree of correlation obtained between N values (r=0.77 (r) R2=59.3%). A significant positive correlation indicates that cases with high scores on the pre-treatment variable tend to score high on the post-treatment variable. In contrast, those with low scores on the pre-treatment variable also tend to have low scores on the post-treatment variable (in this case, the correlation was positive).
DISCUSSION
Visual field defects after pars plana vitrectomy have been a frequent topic of discussion in recent years. Possible mechanisms include RNFL "dehydration" during fluid-air exchange(4-5), elevated IOP during vitrectomy, or mechanical trauma to the optic nerve head during the manual detachment of the posterior hyaloids(6).
As shown in the Results section, there was no statistically significant difference between pre- and postoperative RNFL thickness around the optic nerve in any of the studied regions; this difference was also not significant when comparing sex and age.
It is important to note that the patients in this study were not tested for visual field defects pre- or postoperatively. These results only demonstrate that ILM peeling has no direct impact on RNFL thickness, and the visual field defects shown in the literature might not be related to RNFL thickness changes.
The strong correlation between the extent of nasal and superior nasal thickness and pre-and postoperative global thicknesses must be considered. As described above, the analysis assumes that knowing the extent of both pre- and postoperative nasal thickness, it is possible to determine an approximate value for the global measurement (and vice versa). However, further studies with a greater number of eyes are necessary to justify this finding.
In some eyes, a possible cause for increased postoperative thickness is edema of the inner retinal layers in the first postoperative week, which leads to greater RNFL thickness measurements using OCT.
In conclusion, there appears to be no significant reduction in RNFL thickness measurements after macular hole surgery, regardless of age or sex, in patients not diagnosed with glaucoma or undergoing prior retinal surgery.
REFERENCES
1. Brooks Jr HL. Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology. 2000;107(10):1939-49.
2. Christensen UC, Krøyer K, Sander B, Larsen M, Henning V, Villumsen J, et al. Value of internal limiting membrane peeling in surgery for idiopathic macular hole stage 2 and 3: a randomised clinical trial. Br J Ophthalmol. 2009;93(8):1005-15.
3. Lois N, Burr J, Norrie J, Vale L, Cook J, McDonald A, Boachie C, Ternent L, McPherson G. Full-thickness Macular Hole and Internal Limiting Membrane Peeling Study (FILMS) Group. Internal limiting membrane peeling versus no peeling for idiopathic full-thickness macular hole: a pragmatic randomized controlled trial. Invest Ophthalmol Vis Sci. 2011;52(3):1586-92.
4. Welch JC. Dehydration injury as a possible cause of visual field defect after pars plana vitrectomy for macular hole. Am J Ophthalmol. 1997;124(5):698-9.
5. Hirata A, Yonemura N, Hasumura T, Murata Y, Negi A. Effect of infusion air pressure on visual field defects after macular hole surgery. Am J Ophthalmol. 2000;130(5):611-6.
6. Hutton WL, Fuller DG, Snyder WB, Fellman RL, Swanson WH. Visual field defects after macular hole surgery. A new finding. Ophthalmology. 1996;103(12):2152-8; discussion 2158-9.
7. Ejstrup R, la Cour M, Heegaard S, Kiilgaard JF. Toxicity profiles of subretinal indocyanine green, Brilliant Blue G, and triamcinolone acetonide: a comparative study. Graefes Arch Clin Exp Ophthalmol. 2012;250(5):669-77.
8. Toba Y, Machida S, Kurosaka D. Comparisons of retinal nerve fiber layer thickness after indocyanine green, brilliant blue G, or triamcinolone acetonide-assisted macular hole surgery. J Ophthalmol. 2014;2014:187308. doi: 10.1155/2014/187308.
9. Schuman JS. Spectral domain optical coherence tomography for glaucoma (An AOS thesis). Trans Am Ophthalmol Soc. 2008;106: 426-58.
10. Arora S, Goel N, Arora T, Sharma P, Raina UK, Thakar M, Ghosh B. Comparative evaluation of retinal nerve fiber layer thickness after conventional brilliant blue assisted internal limiting membrane peeling versus brilliant blue selective staining using whole blood in macular hole surgery. Ophthalmic Surg Lasers Imaging Retina. 2016;47(5):436-42.
11. Balducci N, Morara M, Veronese C, Torrazza C, Pichi F, Ciardella AP. Retinal nerve fiber layer thickness modification after internal limiting membrane peeling. Retina. 2014;34(4):655-63.
12. Tosi GM, Martone G, Balestrazzi A, Malandrini A, Alegente M, Pichierri P. Visual field loss progression after macular hole surgery. J Ophthalmol. 2009;2009:617891. doi: 10.1155/2009/617891.
Submitted for publication:
April 24, 2017.
Accepted for publication:
August 31, 2017.
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.