

Jéssica Carolinne Damasceno1; Jordan Isenberg2; Laíse Rondon Lopes3; Bernardo Hime4; Bruno F. Fernandes5; Marcia Lowen6; Luis Marcelo Aranha Camargo7; Rubens N. Belfort6
DOI: 10.5935/0004-2749.20180004
ABSTRACT
Purpose: Malignant lesions of the eyelid are the most common eye cancers. Although rarely lethal, late diagnosis can lead to serious visual morbidity. Definitive diagnosis of neoplastic lesions is pathological. Indications and types of eyelid lesions in a single high-volume ophthalmic reference center in Sao Paulo, Brazil, were analyzed.
Methods: The surgical pathological reports of patients who underwent eye removal procedures between January 2000 and December 2012 were retrieved from the electronic database of the Ophthalmology Department and retrospectively reviewed. Data regarding the final anatomopathological diagnosis, sex, and age were analyzed via the χ2 test with Yates' correction.
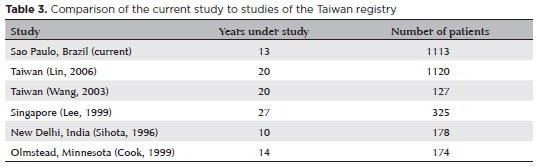
Results: Of the 1,113 eyelid tumors resected over the 13-year study period, 324 (29%) lesions were malignant. The most prevalent lesions were basal cell, squamous cell, and sebaceous gland carcinomas. The median ages of patients (females, n=165, 51%; males, n=159, 49%) with a diagnosis of basal cell, squamous cell, and sebaceous gland carcinomas were 65, 75, and 70 years, respectively.
Conclusion: This is the largest retrospective cohort analysis of eyelid tumors in a Latin American population. These findings are in agreement with those from large centers in other countries and regions.
Keywords: Eyelid neoplasms; Basal cell carcinoma; Squamous cell carcinoma; Melanoma; Brazil
RESUMO
Objetivo: As lesões malignas de pálpebras são os cânceres oftalmológicos mais frequentes. Embora raramente letal, o diagnóstico tardio pode levar a diversas complicações severas e a uma alta taxa de morbidade visual. O diagnóstico definitivo de lesões neoplásicas é patológico. No presente estudo, revisamos casos de um único centro de referência oftalmológica de maior volume em São Paulo, Brasil.
Métodos: Avaliação retrospectiva de todos os tumores palpebrais operados entre os anos de 2000 e 2012 no Departamento de Oftalmologia. Dados incluindo diagnóstico anatomopatológico final, sexo e idade - foram analisados através do método χ2 YATES.
Resultados: Dentre os 1.113 tumores palpebrais ressecados no período de estudo de 13 anos, 324 (29%) dos pacientes com lesões únicas eram malignas. A lesão mais prevalente foi Carcinoma Basocelular (CBC), seguido por carcinoma espinocelular (CEC) e carcinoma de células sebáceas (CCS). A média da idade dos pacientes com diagnóstico de CBC, CCS e CEC foi 65, 75 e 70 respectivamente distribuídos entre 165 (51%) mulheres e 159 (49%) homens.
Conclusão:
Essa é a maior análise de coorte retrospectivo de tumores palpebrais da América Latina. Nossos achados estão de acordo com outros grandes centros de outros países e continentes.
Descritores: Neoplasias palpebrais; Carcinoma basocelular; Carcinoma de células escamosas; Melanoma; Brasil
INTRODUCTION
A variety of benign and malignant tumors commonly develop on the eyelids(1). Often clinically similar in appearance, but with vastly different natural histories, it can be challenging for the general ophthalmologist to accurately differentiate and diagnose malignancy. Although only 15%-20% are malignant(2), periocular epithelial skin lesions can have important esthetic complications, block vision, and change the normal shape and function of the eyelid.
Among malignant tumors, basal cell carcinomas (BCCs) and squamous cell carcinomas (SCCs) are the most common whereas sebaceous gland carcinomas (SGCs) are considered the most aggressive(3). As such histopathological analysis is always required.
Globally the incidence of malignant eyelid lesions is increasing, its global distribution is variable(4). The incidence of age-adjusted eyelid malignancies ranges from 5.1 per 100,000 per year in Singapore(5) to 6.5 in Taiwan(6) and 15.7 in the Minnesota, United States(7).
The present study was performed to characterize the prevalence of eyelid tumors at our center, identify the occurrence of cases of malignant eyelid tumors and to determine the relationship between sex and age in patients with these neoplasms, with the goal of better understanding our regions disease burden as it related globally. To date there are no studies describing eyelid lesions in either Brazil or Latin America generally.
METHODS
The surgical pathological database of the Ophthalmology Department at the Universidade Federal de SãoPaulo'sHospitalwas queried for all specimens received from January 1, 2000 to December 31, 2012 inclusively. Data including ocular tissue of origin, patient's age, sex, histopathological diagnosis, and evaluation of margins were extracted. Cases were divided into non- and malignant eye lid lesions. Malignant cases were further classified by diagnoses. Statistical analysis was performed using OpenEpi(8) software; the Yates correction for continuity test (χ2 Yates), the hazard ratio (HR) and confidence interval (CI) were calculated. The results were considered statistically significant when p<0.05.
RESULTS
Over the three-year study period 3,446 unique patient's surgical specimens were submitted for anatomopathologic analysis by the Department of Ophthalmology. Eyelid lesions represented 1,113 cases (32.3%). Of these, 789 (70.9%) were benign and 324 (29.1%) were malignant.
The most common benign anatomopathological diagnoses (in descending order) were melanocytic nevi (n=120, 15.2%), seborrheic keratosis (107, 13.6%), chalazions (71, 9%), chronic inflammation (44, 5.6%), and actinic keratosis (36, 4.5%). Of the 324 malignant tumors, there were 226 (69.8%) BCCs, 55 (17%) SCCs, 22 (6.8%) SGCs, 6 (1.9%) melanomas, 5 (1.5%) undifferentiated carcinomas, 4 (1.2%) malignant tumors of vascular origin, 3 (0.9%) adenoid cystic carcinomas, and 3 (0.9%) malignant tumors of the lymphoreticular tissue (Table 1). Malignant tumors were more prevalent in men (Yates χ2=38.77; p<0.0000001; HR=1.789; 95% CI=1.492-2.145).
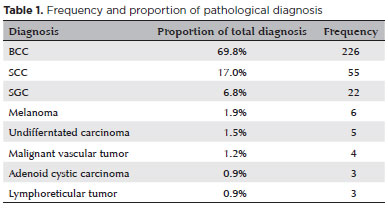
The most common malignant eyelid tumors (in descending order) were BCC (median patient age, 65 years; no sex predilection), SCC (median patient age, 75 years; 61.8% females; sex preference not statistically significant: Yates χ2= 2.64; p=0.052), and SGC (median patient age, 70 years; no sex preference). Six patients had melanoma (median patient age, 67 years). Although there was a higher prevalence in men (83.3%), this finding was not statistically significant (Yates χ2=1.52; p-value=0.10). Lentiginous melanoma was observed in one-third of these patients.
Moreover, other observed malignancies included undifferentiated carcinoma, malignant mesenchymal neoplasms of vascular origin (3 of 4 cases were Kaposi's sarcoma), adenoid cystic carcinoma, and non-Hodgkin lymphoma. Together, these cases accounted for 4.6% of malignant lesions of the eyelid. Malignant lesions were more frequent in patients older than 59 years (Yates χ2=53.17; p-value <0.0000001; HR=2.053; 95% CI= 1.680-2.509).
DISCUSSION
Eyelids commonly develop a variety of benign and malignant tumors. Although only 15%-20% are malignant, periocular epithelial skin lesions can have important esthetic complications, block vision, and change the normal shape of the eyelid. Although variable, the incidence of malignant eyelid lesions continues to increase globally.
The patient distributions and results of the present study, which has one of a largest number of samples and longest duration of all similar reports (Table 2), are similar to those of a study of the Taiwanese registry(6) (Table 3).
BCC is the most prevalent skin cancer with an average lifetime risk for Caucasians of approximately 30%(9). These lesions most commonly occur in those aged >65 years old and are rarely seen in children(10). BCC is more common in men with a male-to-female ratio of approximately 2:1, although the incidence in women aged <40 years is greater than that in men(11). This sex inversion can be partly explained by higher ultraviolet exposure of younger women from tanning beds(12). The role of UV irradiation in the development of BCC is underlined by its low occurrence among ethnicities with more intensely pigmented skin. In fact, Caucasians are at a 19-fold greater risk of BCC than more dark-skinned people(13).
More specifically, BCC is the most prevalent malignant eyelid tumor with an incidence ranging from 65.1% in a Taiwanese population(6) to 90.8% in a population from the state of Minnesota in the northern United States(7). Consistent with the literature, the results of the present study showed that BCC was the most prevalent malignant eyelid tumor, accounting for 69.8% of cases. Although this figure falls on the low end, lower ultraviolet radiation exposure may also explain the lack of a statistical difference between sexes(14).
The occurrence of BCC in individuals younger than 40 years is considered uncommon and relatively few pediatric cases have been documented in the literature, but only on the order of case reports(15,16). Here 12.8% of the BCC specimens were collected from patients aged <50 years and one was collected from a 7-year-old. Nevertheless, this rate was higher than that of a recent report of BCC prevalence in Brazil of just 2.9% of those aged <40 years(17).
SCC is the second most common malignant eyelid tumor, but much less common than BCC(18). SCC accounts for 3.4%(5) to 12.6%(7) of malignant eyelid lesions across frequently cited studies. Here, 17% of lesions were SCC with a larger non-statically significant occurrence in women at 61.8%, though men are often described as most at risk(19). SCC occurs most commonly in older individuals with a history of chronic sun exposure and subsequent skin damage. Most patients diagnosed with SCC are aged >60 years old, similar to the median age of 65 years in the present study. The higher incidence in women and as a proportion of lesions may be explained by increased ultraviolet exposure by this group.
SGC accounts for less than 0.5%(7) up to 10.2%(5) of eyelid malignancies and is generally considered the third most common eyelid malignancy following BCC and SCC. The incidence of SGC in the present study was 6.8%, in line with that reported in other studies(6) likely because SGC is ultraviolet independent.
The primary modifiable risk factor for melanoma is exposure to ultraviolet radiation(20). Melanoma accounts for less than 1% of eyelid malignancies globally(5-7). In contrast, of the malignant lesions in the present study, melanoma accounted for 1.9%, with 83.3% occurring in men. This slightly higher incidence of melanoma, as compared to that in the literature, and the effect in men can likely be explained by the small number of cases (n=6) encountered in our hospital over the 13-year study period.
The incidence of undifferentiated carcinomas in this study was 1.5%. However, it is difficult to compare our findings with those of previous studies because the incidence of undifferentiated carcinomas is often reported as "carcinoma not otherwise specified" at 2.4%(5), "other carcinoma" at 4.3%(6), or simply not reported as a BCC, SCC, SGC, or melanoma(7).
Malignant mesenchymal tumors of vascular origin represented 1.2% of cases described in this study. Two-thirds of these cases were Kaposi's sarcoma found in HIV-seropositive patients. Prior to the advent of highly active antiretroviral therapy, Kaposi's sarcoma presented in the ocular adnexa of approximately 5% of HIV/AIDS patients(21). However, recent studies have shown a decrease in this frequency to as low as 0.4%(22).
Adenoid cystic carcinoma is a rare subtype of sweat gland carcinoma that primarily affects middle-aged adults. Present in 0.9% of the malignant eyelid lesions in this study, it is known to be indolent for a prolonged period before the patient seeks medical attention, which corresponds to the author's findings. This tumor has a deceptively benign histologic appearance characterized by sluggish growth, is locally invasive, and has a high propensity for local recurrence(23), reinforcing the need for early diagnosis.
Lymphoreticular tissue tumors are neoplasms affecting the eye and its attachments in primary and secondary forms, including the conjunctiva and eyelid. An estimated 8% of cases of ocular adnexa lymphomas are non-Hodgkin lymphomas. The occurrence of lymphoid tumors in this study was 0.9%, all of which were non-Hodgkin lymphomas. Lymphoid tumors are considered rare eyelid neoplasms and affect all ages, but are mostly seen in individuals in the fifth and seventh decades of life. There is no sex preference in the literature, though a slight non-significant preponderance in men was observed in the present study (66.6%).
This is the first retrospective cohort analysis of eyelid tumors in a Latin American population to characterize the prevalence of eyelid tumors, identify the occurrence of malignant eyelid tumors, and to determine the relationship between patient sex and age with the incidence of these neoplasms, with the goal to better understand the burden of eyelid tumors in our region, as related globally. Unfortunately, at this time, we do not have access to perform a follow-up study of the rates of recidivism.
Our findings are in agreement with those from large centers conducted in other countries and regions. Understanding these data can aid in more effective therapeutic management. Future, region-specific (i.e., São Paulo State) studies of the incidence and prevalence of eyelid tumors are being planned for a more precise peer comparison.
REFERENCES
1. Margo CE, Mulla ZD. Malignant tumors of the eyelid: a population-based study of non-basal cell and non-squamous cell malignant neoplasms. Arch Ophthalmol. 1998;116(2):195-8.
2. Kersten RC, Ewing-Chow D, Kulwin DR, Gallon M. Accuracy of clinical diagnosis of cutaneous eyelid lesions. Ophthalmology. 1997; 104(3):479-84.
3. Bernardini FP. Management of malignant and benign eyelid lesions. Curr Opin Ophthalmol. 2006;17(5):480-4.
4. Myers M, Gurwood AS. Periocular malignancies and primary eye care. Optometry. 2001;72(11):705-12.
5. Lee SB, Saw SM, Au Eong KG, Chan TK, Lee HP. Incidence of eyelid cancers in Singapore from 1968 to 1995. Br J Ophthalmol. 1999;83(5):595-7.
6. Lin HY, Cheng CY, Hsu WM, Kao WH, Chou P. Incidence of eyelid cancers in Taiwan: a 21-year review. Ophthalmology. 2006;113(11): 2101-7.
7. Cook BE, Jr., Bartley GB. Epidemiologic characteristics and clinical course of patients with malignant eyelid tumors in an incidence cohort in Olmsted County, Minnesota. Ophthalmology. 1999; 106(4):746-50.
8. Dean A, Sullivan K, Soe M. OpenEpi: Open Source Epidemiologic Statistics for Public Health [updated 4 May 20143 April 2016]. Available from: http://www.OpenEpi.com.
9. Lear JT, Smith AG. Basal cell carcinoma. Postgraduate medical journal. 1997;73(863):538-42.
10. Rogers HW, Weinstock MA, Harris AR, Hinckley MR, Feldman SR, Fleischer AB, et al. Incidence estimate of nonmelanoma skin cancer in the United States, 2006. Arch Dermatol. 2010;146(3):283-7.
11. Staples M, Marks R, Giles G. Trends in the incidence of non-melanocytic skin cancer (NMSC) treated in Australia 1985-1995: are primary prevention programs starting to have an effect? Int J Cancer. 1998;78(2):144-8.
12. Lim JL, Stern RS. High levels of ultraviolet B exposure increase the risk of non-melanoma skin cancer in psoralen and ultraviolet A-treated patients. J Invest Dermatol. 2005;124(3):505-13.
13. Roewert-Huber J, Lange-Asschenfeldt B, Stockfleth E, Kerl H. Epidemiology and aetiology of basal cell carcinoma. Br J Dermatol. 2007;157 Suppl 2:47-51.
14. Popim RC, Corrente JE, Marino JA, de Souza CA. [Skin cancer: use of preventive measures and demographic profile of a risk group in the city of Botucatu]. Ciênc Saude Colet. 2008;13(4):1331-6. Portuguese.
15. Efron PA, Chen MK, Glavin FL, Kays DW, Beierle EA. Pediatric basal cell carcinoma: case reports and literature review. J Pediatr Surg. 2008;43(12):2277-80.
16. Christenson LJ, Borrowman TA, Vachon CM, Tollefson MM, Otley CC, Weaver AL, et al. Incidence of basal cell and squamous cell carcinomas in a population younger than 40 years. JAMA. 2005; 294(6):681-90.
17. Ferreira FR, Pevide Bda C, Rodrigues RF, Nascimento LF, Lira ML. Differences in age and topographic distribution of the different histological subtypes of basal cell carcinoma, Taubate (SP), Brazil. An Bras Dermatol. 2013;88(5):726-30.
18. Donaldson MJ, Sullivan TJ, Whitehead KJ, Williamson RM. Squamous cell carcinoma of the eyelids. Br J Ophthalmol. 2002;86(10): 1161-5.
19. Soares LH, Bello CV, Reis AK, Nunes RR, Mason EM. Malignant eyelid tumors. Arq Bras Oftalmol. 2001;64:287-9.
20. Gandini S, Sera F, Cattaruzza MS, Pasquini P, Picconi O, Boyle P, et al. Meta-analysis of risk factors for cutaneous melanoma: II. Sun exposure. Eur J Cancer. 2005;41(1):45-60.
21. Shuler JD, Holland GN, Miles SA, Miller BJ, Grossman I. Kaposi sarcoma of the conjunctiva and eyelids associated with the acquired immunodeficiency syndrome. Arch Ophthalmol. 1989;107(6):858-62.
22. Jabs DA, Van Natta ML, Holbrook JT, Kempen JH, Meinert CL, Davis MD, et al. Longitudinal study of the ocular complications of AIDS: 1. Ocular diagnoses at enrollment. Ophthalmology. 2007; 114(4):780-6.
23. Jaso J, Malhotra R. Adenoid cystic carcinoma. Arch Pathol Lab Med. 2011;135(4):511-5.
Submitted for publication:
March 14, 2017.
Accepted for publication:
August 8, 2017.
Funding: No specific financial support was received for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.
Approved by the following research ethics committee: Hospital São Paulo (# 0115/07).