

Remzi Karadag; Bahar Gunes; Ahmet Demiorok
DOI: 10.5935/0004-2749.20170096
ABSTRACT
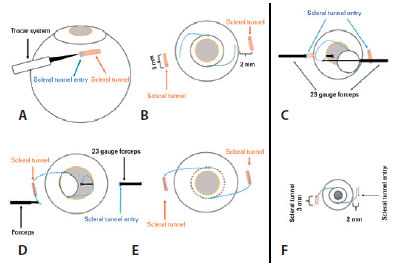
Trocar-assisted intraocular lens (IOL) reposition surgery using a scleral fixation method was performed for a patient with a dislocated sulcus IOL. Two 3-mm-long scleral tunnels 2 mm from and parallel to the limbus were formed using a 23-gauge vitrectomy trocar transconjunctivally entering the sclera at an angle of approximately 10°. Haptics were collected using a 23-gauge serrated retinal forceps entering from the trocar cannula and externalized from the scleral tunnels together with the trocar. The same procedure was applied for the other haptic. Both haptics were pushed into the scleral tunnel and a transconjunctival secure 10-0 nylon suture was placed at the scleral tunnel entry site around the haptic. Sutures were removed 1 week later. No complications occurred intraoperatively or postoperatively. At a 10-month follow-up, IOL was stabilized. IOL reposition surgery using the trocar-assisted IOL scleral fixation method is a viable alternative to intrascleral fixation surgery.
Keywords: Lens, intraocular; Lens implantation, intraocular; Sclera/surgery; Prosthesis failure; Ophthalmologic surgical procedures; Humans; Case reports
RESUMO
Relatamos uma cirurgia de reposição de lentes intraoculares (LIO) usando o método de fixação escleral de lentes intraoculares usando o trocarte em paciente com lentes intraoculares deslocada no sulco. Nós formamos dois túneis esclerais de 3 mm de comprimento, de 2 mm e paralelos ao limbo, com trocarte de vitrectomia de calibre 23 passando pela esclera transconjonctivalmente em um ângulo de aproximadamente 10 graus. Os hápticos foram capturados por uma pinça dentária dentada de calibre 23 que entrou na cânula do trocarte e os hápticos foram externalizados pelos túneis esclerais, através do trocarte. O mesmo procedimento aplicado para o outro háptico. Ambos os hápticos foram empurrados para o túnel escleral e uma sutura segura transconjuntival é colocada no local de entrada do túnel escleral em torno do háptico com uma sutura de nylon 10-0. As suturas foram removidas uma semana depois. Não foram observadas complicações intraoperatórias ou pós-operatórias. Após o período de seguimento de 10 meses, a lentes intraoculares foi vista estabilizada. A cirurgia de reposição de lentes intraoculares usando o método de fixação escleral de lentes intraoculares assistido com trocarte é uma cirurgia alternativa de fixação intraescleral.
Descritores: Lentes intraoculares; Implante de lente intraocular; Esclera/cirurgia; Falha de prótese; Procedimentos cirúrgicos oftalmológicos; Humanos; Relatos de casos
INTRODUCTION
Intraocular lens (IOL) malposition/dislocation is a possible complication of cataract surgery. The most common causes of postoperative IOL dislocation is insufficient capsular support in the early period and dislocation of the bag due to progressive zonular dialysis in the late period(1,2). The choice of decentralized vs. dislocated IOL treatment is dependent on the clinical features of the patient and the experience and preference of the surgeon. When a decentralized or dislocated IOL is extracted, it could be re-implanted in another position or switched with anoth er type of IOL. It is important to evaluate residual capsular support to choose an optimal IOL reposition. IOL reposition may be adequate for patients with capsular support for whom scleral fixation methods are preferred in case of insufficient capsular support(2,3).
Current sutureless scleral fixation methods are popular for the treatment of aphakic patients without sufficient capsular support(4-8). Furthermore, Singh and Bhalekar used a sutureless pars plana vitrectomy method with 23-gauge serrated retinal forceps for treatment of dislocated IOL(9). We report reposition of a decentralized IOL previously implanted in the sulcus with a trocar-assisted, sutureless, scleral fixation method.
CASE REPORT
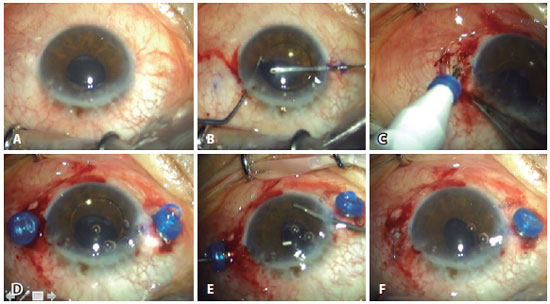
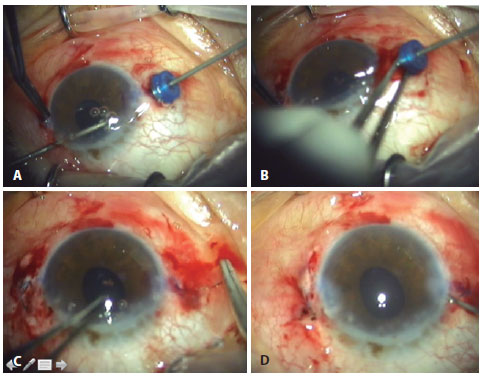
A 70-year-old male presented with low vision and glare 3 months after cataract surgery. An inferiorly dislocated three-piece IOL was observed in the sulcus at the initial examination (Figure 1 A). We planned to fix the implanted IOL with our sutureless technique(7,8), which requires less manipulation since IOL was not explanted. After marking the peripheral cornea at 180° between the 3 to 9 o'clock positions, two opposite corneal incisions were made with a microvitreoretinal knife. The anterior chamber was filled with an ocular viscoelastic substance and the three-piece IOL was passed into the anterior chamber with the help of two Sinsky hooks (Figure 1 B). After this point, the procedure was similar to the trocar-assisted scleral fixation method, as described in our previous reports(7,8). A 3-mm scleral tunnel was formed 2 mm from and parallel to the limbus with a 23-gauge vitrectomy trocar entering the sclera transconjunctivally at an angle of approximately 10° (Figure 1 C). A second scleral tunnel was formed with the same technique 180° from the first (Figure 1 D). Afterward, 23-gauge retinal forceps were entered into the posterior camera through one of the prepared cannulas, whereas a 23-gauge retinal forceps was entered into the anterior chamber through the paracentesis to grasp the contralateral IOL haptic. The haptic was grasped by the tip then advanced to the 23-gauge forceps. The haptic and 23-gauge cannula were explanted simultaneously from the sclerotomy (Figure 1 E). The same procedure was applied to the other haptic (Figure 2 A, B). Both haptics were pushed into the scleral tunnel and a transconjunctival safety 10-0 nylon suture was placed at the scleral tunnel entry site (Figure 2 C). The sutures were removed 1 week later. No complications occurred intraoperatively or postoperatively (Figure 2 D and 3). At a 10-month follow-up exam, IOL was stabilized.
DISCUSSION
Many complications of cataract surgery can cause IOL decentralization, such as asymmetric IOL implantation, capsular tearing, and zonular dialysis. Surgical treatment is necessary in case of glare, diplopia, or loss of visual acuity due to severe IOL decentralization or dislocation(1-3). In the literature, numerous surgical methods have been described to treat such cases. The choice of an optimal and convenient method is dependent on the condition of the capsule(2,3). In case of insufficient capsular support, IOL extraction followed by anterior chamber IOL implantation is a viable option. Alternatively, IOL fixation to the iris or sclera with a suture may be preferred. Each of these methods have unique advantages and disadvantages(10). IOL reposition in the sulcus is a viable option for patients with sufficient capsular support(1-3).
Recently, sutureless scleral fixation methods have been commonly favored(4-8). These methods are generally used as three-piece IOL implantation for aphakic patients without sufficient capsular support. The main advantage of these methods is the avoidance of sutures for scleral fixation, which prevents suture-related complications. Short and midterm results seem to be acceptable(4-8). In the present case, a decentralized three-piece IOL in the sulcus was repaired with a trocar-assisted sutureless scleral fixation method, as described previously. IOL implantation was chosen to avoid IOL exchange. At the same time, numerous intraocular manipulations, as required in sutured scleral fixation techniques, are avoided, resulting in less damage to the surrounding tissue. In addition, since this method is performed transconjunctivally, the conjunctiva is preserved for possible further intervention. Entering the instruments through a trocar also helped to avoid possible damage to the surrounding tissue(7,8). There have been relatively few reports of complications with sutureless scleral fixation, such as IOL decentralization (incidence, 1.97%-5%), cystoid macular edema (1.97%-13.3%), optic capture (2.6%-14.3%), subconjunctival haptic (19%), conjunctival erosion due to haptic exposure (12,5%), transient vitreous hemorrhage (6%-18%), and retinal detachment. None of these complications occurred in the present case(4-8). To the best of our knowledge, this is the first case of sutureless reposition IOL with the aid of a trocar.
In conclusion, IOL reposition surgery using a trocar-assisted IOL scleral fixation method is a viable alternative to intrascleral fixation surgery.
REFERENCES
1. Por YM, Lavin MJ. Techniques of intraocular lens suspension in the absence of capsular/zonular support. Surv Ophthalmol. 2005;50(5):429-62. Comment in: Surv Ophthalmol. 2006;51(3):288; author reply 288.
2. Kim SS, Smiddy WE, Feuer W, Shi W. Management of dislocated intraocular lenses. Ophthalmology. 2008;115(10):1699-704.
3. Smiddy WE. Management of dislocated foldable intraocular lenses. Retina. 2005;25(5): 576-80.
4 Gabor SG, Pavlidis MM. Sutureless intrascleral posterior chamber intraocular lens fixation. J Cataract Refract Surg. 2007;33(11):1851-4. Comment in: Retina. 2014;34(4): 812-5.
5. Prakash G, Agarwal A, Kumar DA, Saleem A, Jacob S, Agarwal A. Translocation of malpositioned posterior chamber intraocular lens from anterior to posterior chamber along with fibrin glue-assisted transscleral fixation. Eye Contact Lens. 2010;36(1):45-8.
6. Karadag R, Celik HU, Bayramlar H, Rapuano CJ. Sutureless intrascleral fixated intraocular lens implantation. J Refract Surg. 2016;32(9):586-97.
7. Totan Y, Karadag R. Trocar-assisted sutureless intrascleral posterior chamber foldable intra-ocular lens fixation. Eye (Lond). 2012;26(6):788-91.
8. Totan Y, Karadag R. Two techniques for sutureless intrascleral posterior chamber IOL fixation. J Refract Surg. 2013;29(2):90-4.
9. Singh R, Bhalekar S. Repositioning a dislocated intraocular lens in the ciliary sulcus using 23-gauge sutureless pars plana vitrectomy. J Cataract Refract Surg. 2011;37(3): 438-40.
10. Wagoner MD, Cox TA, Ariyasu RG, Jacobs DS, Karp CL; American Academy of Ophthalmology. Intraocular lens implantation in the absence of capsular support: a report by the American Academy of Ophthalmology. Ophthalmology. 2003;110(4):840-59.
Submitted for publication:
April 7, 2017.
Accepted for publication:
August 8, 2017.
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.