

Virgilio Galvis1,2,3; Alejandro Tello1,2,3; Johanna Otero1; Andrés A. Serrano1; Luz María Gómez1; Yuly Castellanos1,2
DOI: 10.5935/0004-2749.20170088
ABSTRACT
Purpose: The aim of this study was to establish the frequency of refractive errors in children and adolescents aged between 8 and 17 years old, living in the metropolitan area of Bucaramanga (Colombia).
Methods: This study was a secondary analysis of two descriptive cross-sectional studies that applied sociodemographic surveys and assessed visual acuity and refraction. Ametropias were classified as myopic errors, hyperopic errors, and mixed astigmatism. Eyes were considered emmetropic if none of these classifications were made. The data were collated using free software and analyzed with STATA/IC 11.2.
Results: One thousand two hundred twenty-eight individuals were included in this study. Girls showed a higher rate of ametropia than boys. Hyperopic refractive errors were present in 23.1% of the subjects, and myopic errors in 11.2%. Only 0.2% of the eyes had high myopia (≤-6.00 D). Mixed astigmatism and anisometropia were uncommon, and myopia frequency increased with age. There were statistically significant steeper keratometric readings in myopic compared to hyperopic eyes.
Conclusions: The frequency of refractive errors that we found of 36.7% is moderate compared to the global data. The rates and parameters statistically differed by sex and age groups. Our findings are useful for establishing refractive error rate benchmarks in low-middle-income countries and as a baseline for following their variation by sociodemographic factors.
Keywords: Refractive errors; Myopia; Hyperopia; Astigmatism; Anisometropia; Children
RESUMO
Objetivo: O objetivo deste estudo foi estabelecer a frequência de erros refrativos em crianças e adolescentes com idade entre 8 e 17 anos, residentes na região metropolitana de Bucaramanga (Colômbia).
Métodos: Este estudo foi uma análise secundária de dois estudos descritivos transversais que aplicaram levantamentos sociodemográficos e avaliaram a acuidade e a refração visuais. As ametropias foram classificadas como erros miopicos, erros hipermetrópicos e astigmatismo misto. Os olhos eram considerados emétropes se nenhuma dessas classificações fosse feita. Os dados foram coletados usando software livre e analisados com STATA/IC 11.2.
Resultados: Mil e duzentos e vinte e oito indivíduos foram incluídos neste estudo. As meninas mostraram uma maior taxa de ametropia do que os meninos. Erros refrativos hipermetrópicos estavam presentes em 23,1% dos indivíduos e erros miópicos em 11,2%. Apenas 0,2% dos olhos apresentavam miopia alta (≤-6,00 D). O astigmatismo misto e a anisometropia eram incomuns e a frequência de miopia aumentava com a idade. Houve leituras queratométricas mais acentuadas estatisticamente significativas em míopes em comparação com os olhos hipermétropes.
Conclusões: A frequência de erros de refração que encontramos em 36,7% é moderada em comparação com os dados globais. As taxas e os parâmetros diferiram estatisticamente por sexo e grupos etários. Nossas descobertas são úteis para estabelecer padrões de referência de erro de refração em países de baixa renda média e como base para seguir sua variação por fatores sociodemográficos.
Descritores: Erros de refração; Miopia; Hipermetropia; Astigmatismo; Anisometropia; Criança
INTRODUCTION
In recent decades, the prevalence of myopia has significantly increased, especially in some Asian countries(1). In the last 6 years, studies from Taiwan, China, and Korea have reported very high rates of myopia, between 80.7 and 96.5%, in older adolescents and young adults(2-4). Increases in the prevalence of myopia have also been identified in children from other countries, including Australia and India(5,6). If these trends continue, according to the findings of a recent meta-analysis by Holden et al., by 2050, almost half of the world's population will have myopia (spherical equivalent [SE] of ≤-0.50 diopters [D]) and almost 10% will have high myopia (SE of ≤-5.00 D)(7). Myopia is related to genetic risk factors (myopia in parents) and environmental factors such as extended time spent on near-vision activities (additionally influenced in recent years by increased use of technologies such as electronic tablets and smartphones), shorter distance from text to the eyes, less time spent outdoors, and living in urban areas(6,8-10). Additionally, some researchers have suggested that diet may play a role in the increased prevalence of myopia(8,11,12).
There is little information on the frequency of refractive errors in children in Colombia and in Latin America in general, and the quality of the information in some of the few published articles is not optimal(13-21). It is striking, however, that one of the studies with an adequate study design carried out in Monterrey, Mexico, in 1999, found a high prevalence of myopia in at least one eye (44%) among 1,035 children aged 12-13 years old(18). Another study performed in the city of Nezahualcóyotl (part of the Mexico City Metropolitan Area) in 2001 also showed a high rate of myopia (33%) in children between 6 and 15 years of age(19). The aim of the present study was to establish the rate of refractive errors in children and adolescents living in an urban area (the metropolitan area of Bucaramanga, Colombia), as well as its distribution according to different sociodemographic characteristics. The analysis included the health services affiliation; the Colombian health system includes the so-called "contributory" and "special" schemes. Both public and private companies operate as insurers and administrators, and are responsible for hiring health service providers. In these schemes, the affiliate (or the company hiring that person) makes a monthly direct payment. The third system is called the "subsidized scheme," the aim of which is to provide coverage for poor and vulnerable populations; in this scheme, the affiliate does not make any payments. A small percentage of the population does not have any health affiliation.
METHODS
Design and sample characteristics
A secondary analysis of the study population in two descriptive cross-sectional studies was conducted. These studies were "Association between cardiorespiratory and muscular capacity with metabolic risk factors in Colombian children" (known by its acronym in Spanish, ACFIES) and "Determination of the prevalence of myopia and its association with environmental influences in Colombian urban and rural population" (known by its acronym in Spanish, MIOPUR). The information was taken from the databases constructed in those two previous cross-sectional studies, which had similar methods of sample selection and data collection. The ACFIES study was performed between April and September 2013, and MIOPUR (in Bucaramanga) between September 2013 and February 2014. The age groups included in the two studies were similar (8 to 17 years old). All the participants were living in the metropolitan area of Bucaramanga (Colombia).
In Colombia, there is an official national social classification of houses and properties by strata, in an attempt to categorize the inhabitants of these houses according to their socioeconomic status. The criteria include characteristics of the dwelling such as whether or not it has a garage, a front yard, a backyard, and also the quality of the neighborhood in general. There are six strata: level one is lower-low, two is low, three is upper-low, four is medium, five is medium-high, and six is high. Children from all six different socioeconomic strata of the city were included, and were chosen by non-probabilistic sampling by intention. At the time of arriving in each neighborhood, members of the studies' fieldwork team tried to contact the children of the neighborhood by various means, to ask them to attend the screening tests. We selected a non-probabilistic sampling design in both original studies (ACFIES and MIOPUR) because there was no list of the population of children in each area; further, these studies were considered as exploratory research to find out the magnitude of a problem not previously studied in the population of Bucaramanga, namely, the refractive errors among children, in a quick and inexpensive manner. We applied the convenience sampling technique because it was the easiest method for the time and resources available for the studies.
Information collection
A questionnaire was administered to each participant to collect demographic and socioeconomic data, including information regarding their health services affiliation (schemes with and without direct payment by the user) and the mean monthly household income, taking as reference point one minimum legal salary in Colombia (about USD201). Data collection was conducted from April 2013 to February 2014.
Refractive status and keratometry determination
Visual acuity, using a Snellen chart at 6 m, noncycloplegic retinoscopy (asking the patient to fixate on a target set at a distance of 6 m in order to relax the accommodation reflex, i.e., so-called static retinoscopy), and subjective manifest refraction evaluation were performed by optometrists. An autorefractor was not used for the refraction evaluation. Keratometry was performed using an auto-keratometer (ARK-530A; Nidek, Tokyo, Japan).
ACFIES and MIOPUR were declared minimal risk investigations, and were approved by the CEI-FOSCAL Research Ethics Committee.
Inclusion criteria
Children were included in the present study if static retinoscopy, manifest refraction, and keratometry could be properly performed (i.e., those who did not present with corneal irregularity or media opacity to prohibit these tests from being performed) and if their corrected VA was better than 20/40. These criteria were decided on to ensure that the subjective manifest refraction results were reliable. In addition, eyes with a history of ocular surgery or corneal disease (including evident keratoconus) were excluded.
Refractive errors classification
The refractive status of each eye was classified into four groups as follows:
• Emmetropia: SE greater than -0.50 D and less than +0.50 D, provided that the absolute value of the cylinder was less than or equal to 0.75 D.
• Myopia: SE less than or equal to -0.50 D, and sphere value less than or equal to zero. Therefore, the myopia group included those with myopia and simple and compound myopic astigmatisms (eyes were included in the subgroup of high myopia: if they had an SE ≤-6.00 D).
• Hyperopia: SE greater than or equal to +0.50 D, sphere greater than or equal to zero, and an absolute value of the cylinder less than or equal to the absolute value of the sphere. This group included those with hyperopia and simple and compound hyperopic astigmatisms.
• Mixed astigmatism: Sphere value greater than zero, absolute value of the cylinder greater than or equal to 1.00 D, and absolute value of the cylinder greater than the absolute value of the sphere.
Participants were classified as emmetropes when emmetropia was found in both eyes. If at least one eye had ametropia, the participants were classified according to the identified refractive error. When both eyes differed regarding ametropia, the patient was included in the anisometropia group.
Statistical analysis
We described the sample using counts, percentages, and 95% confidence intervals (95% CI), with their means and standard deviation (SD), for discrete and continuous variables, respectively. Associations between independent variables and refractive errors were evaluated with the chi-square test for categorical variables and analysis of variance (ANOVA) for continuous variables. We used a two-sided significance level of 5%, and the analysis was performed using STATA/IC 11.2 statistical package (StataCorp, College Station, TX, USA).
RESULTS
The study included 1228 participants, with 616 (50.2%) girls. The age range was 8 to 17 years (mean 11.4 ± 2.1 years), and 691 (56.3%) were affiliated to a contributory or special health system. Further, 781 (63.6%) had a mean monthly household income of higher than one minimum legal salary for Colombia.
The rates of refractive errors with respect to sex, age group, health affiliation system, and monthly household income are shown in table 1.
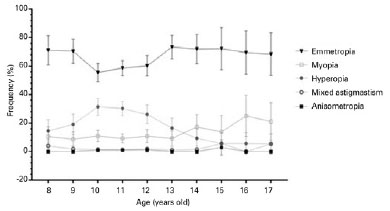
The rate of ametropia, taking into account the whole group of children from 8 to 17 years old, was 36.7% (95% CI: 34.0-39.4). We found statistically significant differences in the frequency of refractive errors by sex and age groups, but not by health affiliation system or monthly household income. Girls had higher rates of both hyperopic and myopic errors. Additionally, the rate of myopic errors increased with age, whereas hyperopic errors diminished with age.
Figure 1 shows the rates of refractive errors by age and their respective intervals. Hyperopia was the most common refractive error until 13 years of age, peaking at 10 years of age, at 31.4% (95% CI: 25.4-27.5). Between 14 and 17 years of age, myopia was the most common refractive error, with its highest frequency found among 16-year-olds, at 15% (95% CI: 10.6-39.4) (Figure 1 and Table 1).
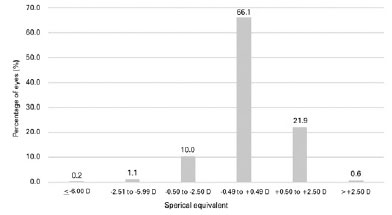
The correlation between the SE of the right and left eyes was 0.887 (p<0.001). Therefore, the SE of the right eye was taken as the reference in figure 2, which shows the distribution of the SE in the entire study population. Six hundred forty-one (11.4%) eyes had a myopic SE (≤-0.50 D), two (0.2%) eyes had high myopia (≤-6.00 D), and 276 (22.5%) eyes had a hyperopic SE (≥+0.50 D).
The correlation between the mean keratometry of the right and left eyes was r=0.973 (p<0.001). Therefore, the right eyes of the children were taken as the reference for the keratometry analysis. When comparing the mean keratometries of the four groups (emmetropes, myopes, hyperopes and eyes with mixed astigmatism), a statistically significant difference was observed between hyperopic and myopic eyes after applying Bonferroni correction (p=0.022) (Table 2).
DISCUSSION
Various transverse and longitudinal studies in schoolchildren have shown an increase in the frequency of myopic defects and a corresponding decrease in the rate of hyperopia as age increases(1,5,22-24). We observed the same trend in these frequencies in our study.
With a cut-off of the SE of +2.00 D or higher for significant hyperopia, we found that 1.1% of our sample population had this condition (in at least one eye), which is similar to the rate found in Malaysia(25). In India, a higher frequency of 7.7% was found(23). Similarly, in children aged 10-13 years in Saudi Arabia, a higher hyperopia rate of 9% was reported, compared to our findings in this age group (1.3%)(26). In a group of 12-year-old children of diverse ethnic origin living in Australia, 2.4% had hyperopia of +2.00 D or more; interestingly, while the rate of this condition was 3.0% in Caucasian, the frequency was 0% in Asian children. In 17-year-olds, the overall rate was 1.5%: 2.0% in Caucasians and 0.9% in Asians(5). The rate of hyperopia in 17-year-olds in our study was 0%. In Chile, in 1998, a 7.5% prevalence of +2.00 D hyperopia or greater was found in children aged 14-15 years(17). In this age group, we found a 0.9% rate of this condition. In all those studies reporting on hyperopia, the researchers, unlike us, used the cycloplegic refraction method.
In 2000, the prevalence of myopia in children in Taiwan was found to be 21% and 61% in 7- and 12-year-olds, respectively(1). More recently, in 2015, the prevalence of myopia in Shanghai, China, was found to be 16.3%, 49.6%, and 75.5% in 8-, 12-, and 16-year-olds, respectively(24). Lower rates of 9.4% and 29.4% were reported in a study performed in the UK among 6-7- and 12-13-year-olds, respectively(27). In Malaysia, myopia rates of 13.6% and 23% were reported in 8- and 12-year-olds, respectively(25). Further, in a group of 12-year-old Australian children, the frequency of myopia was reported to be 18.9%; however, this frequency differed between Caucasian and Asian children, with rates of 8.6% and 52.5%, respectively(5). In our study group, the frequency of myopic errors in 12-year-olds was 10.8%. A previous study showed a 46% rate of myopic refractive errors in 10-13-year-olds in Saudi Arabia(26); we found a rate of 10% in the same age group. Recently, a prevalence of 80.7% in 16-18-year-olds was reported in Mainland China(3). In a group of 17-year-olds from Australia, a prevalence of 30.8% was found; however, the prevalence differed between Caucasians and Asians, at 17.7% and 59.1%, respectively(5). We found much lower rates in our study population: 25% and 21% in 16- and 17-year-olds, respectively. A recent report from India found a prevalence of 15.3% in 11-15 year-olds(6). In 1998, in Chile, a myopia prevalence of 12.5% was found in children aged 14-15 years(17). In our study, the rates for these age groups were 9.6% and 16.2% in children aged 11-13 and 14-15 years, respectively.
Two studies in India showed lower rates in rural communities than those found by us and those reported in children living in cities. For 8-year-olds, these rates were 2.9% in rural areas and 5.7% in urban areas; for 12-year-olds, these rates were 4.8% and 9.7%, respectively; and for 15-year-olds, these rates were 6.7% and 10.8%, respectively(22,23). We found rates of 10.5%, 10.8%, and 13.9% in 8-, 12-, and 15-year-olds living in urban neighborhoods.
A study performed in 1999 in Mexico showed a high frequency of myopia of 44% in a group of 12-13-year-old children(18). In 2009, another group of researchers found a prevalence of myopia of 33% in 6-15-year-olds also living in Mexico(19). In contrast, the prevalence of myopia in a group of children aged 10-15 years in Brazil in 2007 was very low, at only 3.4%(20). Additionally, an extremely low frequency of myopia of 1.2% was reported in a group of Mennonite schoolchildren of European descent in Paraguay(21). However, the authors did not clearly indicate the myopic children's age (they only stated that children were aged 5-16 years), and therefore, it is not possible to make specific comparisons with our results
Recently, Rudnicka et al. performed a meta-analysis on 143 studies from 42 countries, and found that East and Southeast Asian children had the highest rates of myopia, reaching 69% in 15-year-olds (a rate of 86% was found among Chinese children in Singapore at that age). Black children in Africa showed the lowest prevalence in 15-year-olds, at 5.5%(10). In our group of Colombian children and adolescents living in an urban area, the frequency of myopia among 15-year-olds was moderate, at 13.9%.
Regarding high myopia (-6.0 D or greater), in 2000, rates of 3.4%, 13%, and 21% were found in 12-, 15-, and 18-year-olds in Taiwan, respectively(1). Further, in young adults aged 19 years in South Korea, a rate of 21.6% was reported in 2010(4). In 12-, 15-, and 17-year-olds in our study, we found much lower rates of high myopia (0.6%, 0%, and 0%, respectively).
There are few studies on the frequency of refractive errors in children in Colombia. In 1995, a study of schoolchildren living in an urban area (Medellín) showed a refractive error rate of 48% in a group of 17,697 children aged 5-14 years. Hyperopia of 0.25 D or greater was the most common refractive error (with a prevalence of approximately 33.2%), followed by astigmatism (13%) and myopia of 0.25 D or higher (1.4%). However, different age groups were not analyzed(13). A retrospective study analyzed 1502 Individual Provision of Health Services Records, known as RIPS (by its acronym in Spanish), collected from the files of a health institution in Pereira, Colombia, between 2006 and 2007. The average age of the patients was 11 years (25-75 percentile was 9-14 years), with myopia, hyperopia, and astigmatism reported in 11.45%, 50.6%, and 26.1% of the records, respectively. However, an analysis by age groups was not performed. Additionally, these types of records (RIPS) that are filled for statistical information, are generally unreliable in terms of the specific type of refractive error(14). Another study published in 2003 performed in 5-14-year-old schoolchildren in Bogotá, Colombia, showed that 59.2% had hyperopia, 28.2% astigmatism, 4% myopia, and 9% emmetropia. However, the authors did not specify the cut-off limits that were used to define the different refractive errors(15). Additionally, Figueroa et al. did not find any cases of myopia in a small group (n=50) of children aged 3-7 years in Bogotá, Colombia; however, the sample was too small for any conclusions to be drawn(16).
Regarding keratometry, myopic eyes have been found to have steeper corneas. When comparing 30 emmetropic eyes with 73 myopic eyes in young adult patients, Carney et al. reported that the corneas of emmetropic eyes were flatter than those of myopic eyes, and that as the severity of the myopia increased, the cornea became steeper(28). AlMahmoud et al. compared 3091 myopic with 284 hyperopic eyes in adults, and also found that myopic eyes had a mean keratometry steeper than hyperopic eyes (44.02 D versus 43.17 D)(29). We found no studies that analyzed keratometry versus refractive error in children. We found similar results in our sample to those of the abovementioned studies on adults. In addition, although the mean corneal curvature was only slightly steeper in the myopic group (43.42 D) than in the hyperopic group (42.95 D), the differences were statistically significant.
In this study, we decided to perform noncycloplegic static retinoscopy (the patients were asked to fixate on a distant target in an attempt to relax the accommodation reflex), and subjective manifest refraction as described by Marsh-Tootle & Frazier(30). However, without cycloplegia, it is impossible to assure that the refraction is completely "static." For this reason, cycloplegic refraction is more accurate for determining the refractive state of eyes, especially hyperopic eyes. On the other hand, cycloplegia is associated with a number of disadvantages, including undesirable side effects, longer testing time, discomfort, cost, and inconvenience. In fact, in children 8 years or older, some experts prefer static retinoscopy, which involves asking the child to fixate on a high-contrast, detailed target presented at a specific distance under binocular conditions. An advantage of this method is that the accuracy of retinoscopy is improved with smaller pupils; further, children in this age group are old enough to cooperate during subjective refraction and respond better without a dilated pupil. We believed that this static retinoscopy technique would be more appropriate for our study in children aged 8 years or older. However, it could be considered a weakness of our study. We might have overestimated the frequency of myopia and underestimated that of hyperopia, and this could have caused some of the differences found between ours and other studies. In addition, although we included children from all the socioeconomic strata (1-6 according to the characteristics of the houses in each neighborhood), we did not use strict probability-based sampling; thus, we cannot generalize the results from our sample to the whole population. Furthermore, biases in our sample could have occurred because of the convenience sampling technique that we used, which could have led to under- or overrepresentation of particular groups of refractive errors within the sample. However, the information obtained on the frequency of refractive errors in this group of 1228 children is a good starting point for the possible implementation of public health measures in our region and for designing future population studies.
CONCLUSION
In a group of 1228 children and adolescents living in an urban area in Northeast Colombia, we found that the frequency of refractive errors was not influenced by health system affiliation modality or household income level. We found higher rates of ametropia in girls than in boys. Over the whole age group (8-17 years), 11.2% had myopic errors, 23.1% hyperopic errors, and 1.7% mixed astigmatism. We also found that the frequency of myopic refractive errors increased with age, and myopic eyes had steeper corneas than hyperopic eyes.
REFERENCES
1. Lin LLK, Shih YF, Hsiao CK, Chen CJ. Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann Acad Med Singapore. 2004;33(1):27-33.
2. Lee Y-Y, Lo C-T, Sheu S-J, Yin L-T. Risk factors for and progression of myopia in young Taiwanese men. Ophthalmic Epidemiol. 2015;22(1):66-73.
3. Wu LJ, You QS, Duan JL, Luo YX, Liu LJ, Li X, et al. Prevalence and associated factors of myopia in high-school students in Beijing. PLoS One. 2015;10(3):e0120764.
4. Jung SK, Lee JH, Kakizaki H, Jee D. Prevalence of myopia and its association with body stature and educational level in 19-year-old male conscripts in Seoul, South Korea. Investig Ophthalmol Vis Sci. 2012;53(9):5579-83.
5. French AN, Morgan IG, Burlutsky G, Mitchell P, Rose KA. Prevalence and 5- to 6-year incidence and progression of myopia and hyperopia in Australian schoolchildren. Ophthalmology. 2013;120(7):1482-91.
6. Saxena R, Vashist P, Tandon R, Pandey RM, Bhardawaj A, Menon V, et al. Prevalence of myopia and its risk factors in urban school children in Delhi: The North India myopia study (NIM study). PLoS One. 2015;10(2):1-11.
7. Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-42.
8. Galvis V, Tello A, Camacho PA, Parra MM, Merayo-Lloves J. Bio-environmental factors associated with myopia: An updated review. Arch Soc Esp Oftalmol. 2017;92(7):307-25.
9. Ramamurthy D, Lin Chua S, Saw S. A review of environmental risk factors for myopia during early life, childhood and adolescence. Clin Exp Optom. 2015;98(6):497-506.
10. Rudnicka AR, Kapetanakis V V, Wathern AK, Logan NS, Gilmartin B, Whincup PH, et al. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol. 2016;100(7):882-90.
11. Cordain L, Eaton SB, Brand Miller J, Lindeberg S, Jensen C. An evolutionary analysis of the aetiology and pathogenesis of juvenile-onset myopia. Acta Ophthalmol Scand. 2002;80(2):125-35.
12. Galvis V, López-Jaramillo P, Tello A, Castellanos-Castellanos YA, Camacho PA, Cohen DD, et al. Is myopia another clinical manifestation of insulin resistance? Med Hypotheses. 2016;90:32-40.
13. Rodríguez MA, Castro González M. Salud visual de escolares en Medellín, Antioquia, Colombia. Bol Of Sanit Panam. 1995;119:11-4.
14. Gómez M del P, Betancur CL, Garzón MN. Alteraciones visuales y oculares en pruebas tamiz, Pereira, 2006-2007. Cienc Tecnol Salud Vis Ocul. 2009;7(2):57-65.
15. Hernandez CP, Barrera D, Rodriguez J, Ludeman W, Gomez S. Estudio de prevalencia en salud visual en una población escolar de Bogotá, Colombia, 2000. Cienc Tecnol Salud Vis Ocul. 2003;1:11-23.
16. Figueroa LF, Molina NP. Errores refractivos en niños de tres a siete años en la localidad de Chapinero de la ciudad de Bogotá. Cienc Tecnol Salud Vis Ocul. 2011;9(2):55-61.
17. Maul E, Barroso S, Munoz SR, Sperduto RD, Ellwein LB. Refractive error study in children: Results from La Florida, Chile. Am J Ophthalmol. 2000;129(4):445-54.
18. Villarreal GM, Ohlsson J, Cavazos H, Abrahamsson M, Mohamed JH. Prevalence of myopia among 12- to 13-year-old schoolchildren in northern Mexico. Optom Vis Sci. 2003;80(5):369-73.
19. Rodriguez-Abrego G, Sotelo-Dueñas HM. Prevalencia de miopía en escolares de una zona suburbana. Rev Med Inst Mex Seguro Soc. 2009;47(1):39-44.
20. Moraes Ibrahim F, Moraes Ibrahim M, de Camargo JR, Veronese Rodrigues M de L, Scott IU, Silva Paula J. Visual impairment and myopia in Brazilian children: a population-based study. Optom Vis Sci. 2013;90(3):223-7.
21. Carter MJ, Lansingh VC, Schacht G, del Amo MR, Scalamogna M, France TD. Visual acuity and refraction by age for children of three different ethnic groups in Paraguay. Arq Bras Oftalmol. 2013;76(2):94-7.
22. Dandona R, Dandona L, Srinivas M, Sahare P, Narsaiah S, Muñoz S, et al. Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci. 2002;43(3):615-22.
23. Murthy GVS, Gupta SK, Ellwein LB, Muñoz SR, Pokharel GP, Sanga L, et al. Refractive error in children in an urban population in New Delhi. Invest Ophthalmol Vis Sci. 2002; 43(3):623-31.
24. Yu H, Shao Y, Yuan H, Yan B. Age-determined referral criteria of myopia for large-scale vision screening. Eye Sci. 2015;30(4):151-5.
25. Goh PP, Abqariyah Y, Pokharel GP, Ellwein LB. Refractive error and visual impairment in school-age children in Gombak District, Malaysia. Ophthalmology. 2005;112(4):678-85.
26. Aldebasi YH. Prevalence of correctable visual impairment in primary school children in Qassim Province, Saudi Arabia. J Optom. 2014;7(3):168-76.
27. Logan NS, Shah P, Rudnicka AR, Gilmartin B, Owen CG. Childhood ethnic differences in ametropia and ocular biometry: The Aston Eye Study. Ophthalmic Physiol Opt. 2011; 31(5):550-8.
28. Carney LG, Mainstone JC, Henderson BA. Corneal topography and myopia: A cross-sectional study. Invest Ophthalmol Vis Sci. 1997;38(2):311-20.
29. AlMahmoud T, Priest D, Munger R, Bruce Jackson W. Correlation between refractive error, corneal power, and thickness in a large population with a wide range of ametropia. Investig Ophthalmol Vis Sci. 2011;52(3):1235-42.
30. Marsh-Tootle WL, Frazier MG. Infants, toddlers and children. In: Benjamin WJ, ed. Borish's Clinical Refraction. 2nd ed. Philadelphia: Buiterworth Heinemann Elsevier; 2006. p.1400-1401;1415-1416.
Submitted for publication:
December 12, 2016.
Accepted for publication:
July 18, 2017.
Funding: This study was partially financially supported by the Science, Technology and Innovation Administrative Department (Colciencias), a government agency of the Republic of Colombia
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.
Approved by the following research ethics committee: Fundación Oftalmológica de Santander (#651756933785).