

Dayane Cristine Issaho1; Serena Xiaohong Wang2; David Robert Weakley Jr.3
DOI: 10.5935/0004-2749.20170087
ABSTRACT
Purpose: To report the outcomes in patients undergoing surgical correction of intermittent exotropia and to compare the age at surgery to motor and sensory success.
Methods: This was a retrospective cohort study. The results of patients with intermittent exotropia treated with surgery over a 4-year period were reviewed. Patients were divided into two groups based on age at first surgery (<4 years vs. ≥4 years), and motor and sensory outcomes were compared between the two groups.
Results: One hundred thirty-six patients were evaluated, with 67 and 51 patients undergoing surgery before and after the age of 4 years, respectively. The mean age at surgery was 6.8 ± 2.6 years. The reoperation rate for the patients who underwent surgery before 4 years of age was 48% versus 42% for the ones who underwent surgery after this age (p=0.93). Postoperative stereopsis showed an inverse linear association with age at surgery (p<0.001). For each month younger at the time of surgery, there was 0.69 s of arc worsening in the Titmus test. Conversely, when we separately analyzed the patients in whom the first postoperative alignment was esotropic vs. orthophoric/exotropic, we found no correlation between the immediate postoperative alignment in the first week and sensory outcome at the last visit.
Conclusions: When indicated, patients with intermittent exotropia can be operated upon safely under 4 years of age, and may even present better motor results than older patients. Postoperative stereoacuity in younger children revealed to be worse than in older children; however, this result is unlikely to be due to inadequate age for surgery, but rather, immaturity for performing the stereopsis test.
Keywords: Exotropia/surgery; Oculomotor muscles/surgery; Ophthalmologic sur gical procedures; Age factors; Humans; Child
RESUMO
Objetivo: Descrever os resultados em pacientes submetidos à correção cirúrgica de exotropia intermitente e comparar o sucesso motor e sensorial em relação à idade na cirurgia.
Métodos: Estudo tipo coorte retrospectivo. Os resultados cirúrgicos de pacientes com exotropia intermitente foram avaliados em um período de 4 anos. Os pacientes foram divididos em 2 grupos de acordo com a idade na primeira cirurgia (antes ou após os 4 anos de idade) e foram comparados quanto aos resultados motores e sensoriais.
Results: 136 pacientes foram avaliados, 67 operados antes dos 4 anos e 51 operados após esta idade. A idade média na cirurgia foi de 6,8 ± 2,6 anos. A taxa de reoperação em pacientes operados antes dos 4 anos foi de 48% versus 42% naqueles operados mais tarde (p=0,93). A estereopsia pós-operatória mostrou uma associação linear inversa com a idade na cirurgia (p<0,001). Para cada mês mais jovem na idade da cirurgia, houve uma piora de 0,69 segundos de arco no teste de Titmus. Por outro lado, não foi encontrada correlação entre o alinhamento pós-operatório na primeira semana e o resultado sensorial na última visita, quando avaliamos separadamente os pacientes que se apresentaram com esotropia ou orto/exotropia na primeira semana pós-cirúrgica.
Conclusão: Havendo critério para cirurgia, os pacientes com exotropia intermitente podem ser operados com segurança antes dos 4 anos de idade, e podem muitas vezes apresentar um melhor resultado motor do que os pacientes operados mais tarde. A estereopsia pós-operatória em crianças mais jovens foi pior, mais provavelmente por imaturidade ao realizar o teste do que por idade inadequada na cirurgia.
Descritores: Exotropia/cirurgia; Músculos oculomotores/cirurgia; Procedimentos ci rúrgicos oftalmológicos; Fatores etários; Humanos; Criança
INTRODUCTION
Intermittent exotropia is the second most common type of strabismus (19%) and the most prevalent type of exotropia in childhood (52%)(1).
As with any type of strabismus, surgical intervention is directed toward preservation or restoration of binocular vision, prevention of amblyopia, as well as cosmesis. Many surgeons delay surgery in intermittent exotropia until 4 years of age or after, largely because of concerns that consecutive esotropia (even for a short period of time postoperatively) may lead to amblyopia and/or reduction of stereopsis in young patients(2). Contrarily, some authors have argued that better results can be achieved when surgery is performed before 4 years of age(3,4).
In this study, we report the outcomes of patients undergoing surgical correction of intermittent exotropia and assess the association between age at surgery and motor and sensory success.
METHODS
This study was approved by the Institutional Review Board at the Children's Medical Center Dallas (TX, USA).
We reviewed the records of all patients undergoing primary surgery for intermittent exotropia at the Children's Medical Center Dallas over a 4-year period (January 2008 through December 2011), with a minimum follow-up of 3 years. All procedures were performed by two of the authors (Serena Wang or David Weakley).
The patients' records were analyzed for the following parameters: (1) gender and race, (2) age at first visit and age at surgery, (3) cycloplegic refraction, (4) angle of exotropia at the time of surgery and at most recent follow-up, (5) type and number of procedures performed, and (8) visual acuity and stereopsis at the last visit. Patients were excluded if there was any prior strabismus surgery, no report of stereopsis, presence of other significant ocular comorbidity (e.g., cataract, optic nerve hypoplasia, laser-treated retinopathy of prematurity, etc.), or significant developmental delay or neurologic disorders.
The visual acuity at the most recent follow-up was tested using Snellen optotypes ("E" chart, numbers or letters) or Allen pictures, and acuities were converted to logMAR for statistical analysis. Stereoacuity was tested using the Titmus stereotest.
Amblyopia was defined as the difference of two lines or more (on an eye chart test of visual acuity) between the eyes.
Preoperative cycloplegic refraction was converted to the spherical equivalent and averaged between the eyes for statistical analysis. Hyperopia was defined as spherical equivalent refractive errors ≥2.00 D, astigmatism as cylinder refractive errors ≥0.75 D, and myopia as spherical equivalent refractive errors of -0.5 D or more(5).
Pre- and postoperative alignments were measured with alternate prism cover testing at near (33 cm) and at distance (6 m). The distance deviation was considered for the purpose of analysis. Burian's modification of Duane's classification for exotropic deviations was used(6,7). The presence of pseudo-divergence excess was tested using +3.00 D lenses during the near fixation measurements.
For the purpose of statistical analysis, motor success was defined as a postoperative horizontal deviation of ≤10 prism diopters (PD), and failure as those with >10 PD or those requiring a second procedure during the follow-up period. We attempted to determine whether the age at surgery is correlated with motor or sensory success or failure.
Data were analyzed using IBM SPSS Statistics v.20 (IBM Corp., Armonk, NY, USA). Quantitative variables were described as the mean, median, standard deviation, minimum, and maximum, and categorical variables were described as percentages.
Patients were divided into two groups based on their age at the first surgery (younger than 4 years vs. 4 years or older) and compared. Analysis of quantitative variables was performed using Student's t-test for independent samples or the Mann-Whitney U-test for non-parametric samples, where appropriate. Regarding dichotomous categorical variables, the groups were compared using Fisher's exact test. The association between quantitative variables was made by estimating Spearman's correlation coefficient. P-values less than 0.05 were considered statistically significant.
RESULTS
A total of 136 patients underwent surgery for intermittent exotropia during the study period, and all patients were followed up for at least 3 years. Eighteen patients were excluded, eight for other ocular anomalies, seven for no reported stereopsis, and three for significant neurologic deficits, resulting in 118 patients being included in the study. Seventy patients (59%) were female, 54 (45.8%) were Caucasian, 14 (11.9%) Black, 37 (31.4%) Hispanic, 6 (5%) were Asian, and 2 (1.7%) were from other ethnicities. The ethnicity was not reported for five patients.
Onset of drifting was reported at a mean age of 1.4 ± 1.9 years (range 0 to 8 years), and the mean age at the first visit was 3.6 ± 2.6 years (range 0 to 12.6 years). The mean time between the first visit and the surgery was 8.7 ± 13 months (range 0.1 to 79 months).
Intermittent exotropia of basic or pseudo-divergence excess type was present in 86% of the patients, 11% had divergence excess, and 3% had convergence insufficiency.
The mean spherical equivalent refractive error was 0.47 D ± 1.4 (range -3.00 to +5.00 D). The mean difference in spherical equivalent between the two eyes was 0.076 D. Five patients in each group had anisometropia of over 1 D. Twenty-five (21%) patients were prescribed spectacles at the first visit, eight to treat myopia, one for hypermetropia, seven for hyperopic astigmatism, and nine for myopic astigmatism. There were no patients using minus lenses to control the exotropia.
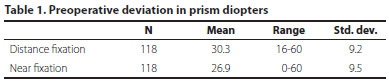
The overall mean preoperative deviation was 30 ± 9 PD at distance and 27 ± 10 PD at near fixation (Table 1).
The mean age at surgery was 6.8 ± 2.6 years (range 8 months to 13 years). All patients underwent bilateral lateral rectus recession as the initial procedure, using standard surgical dosing as described by Parks(8). The mean amount of recession performed in the first surgery was 6.3 ± 0.9 mm (range 4.25 to 8 mm).
At the most recent follow-up (mean age 4.5 ± 1.2 years, range 3 to 7 years), 64 of the patients (54%) had undergone only one procedure, 48 (41%) two procedures, 5 (4%) three procedures, and 1 (1%) four surgeries. The reoperation rate for the patients operated on before 4 years of age was 48% versus 42% for those operated on later (p 0.93).
Amblyopia was present in 11/118 (9.3%) of the patients. Overall, 11/118 (9%) of the patients required inferior oblique recession at some point during follow-up.
Overall, 41/118 (35%) achieved success with one procedure. Undercorrection was found in 96% (74) and overcorrection in 4% (3) of the unsuccessful cases after the first surgery. Satisfactory alignment at the last follow-up (<10 PD), including patients who underwent additional surgery, was achieved in 78/118 (66%) patients.
We evaluated the existence of any linear association between age at surgery and each of the quantitative variables included in the study. Table 2 lists the estimated angular coefficients in each model, with 95% confidence intervals (CIs).
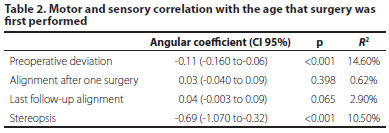
For the variable preoperative deviation, for example, the null hypothesis of no association between preoperative deviation and age at surgery was rejected (p<0.0001). Thus, there is evidence that variation of age at surgery is associated with variation of preoperative deviation. For each month older at the time of surgery, there is a 0.11 PD lower variation on the preoperative distance deviation. It is estimated that 14.6% of the preoperative deviation variations can be explained by age at the time of surgery.
Postoperative stereopsis showed an inverse linear association with age at surgery (p<0.001) (relative risk [RR]: -0.69; 95% CI: -1.07 to -0.32; R2: 10.5%). For each month younger at the time of surgery, there was 0.69 s of arc worsening in the Titmus test.
Tables 3 and 4 summarize the patients' general characteristics and motor and sensory outcomes, comparing the patients undergoing surgery prior to the age of 4 years (67 patients) and those undergoing surgery at the age of 4 years or older (51 patients).
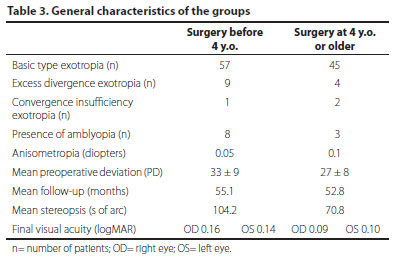
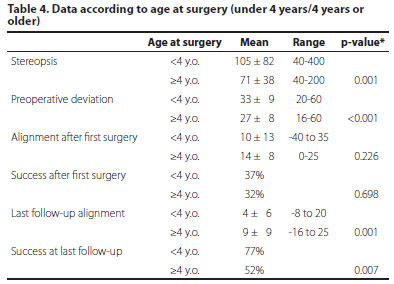
There was no significant difference between the two groups in terms of success after the first surgery (p=0.69) or the need for additional surgery (p=0.71). However, the chance of success at the last follow-up increased by 104% when the initial surgery was performed at a younger age (RR: 2.04; 95% CI: 1.21-3.46).
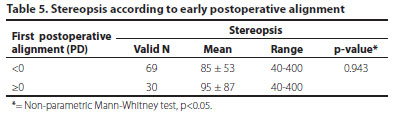
We found no correlation between the immediate postoperative alignment in the first week and sensory outcome at the last visit when we separately analyzed the patients that were esotropic versus those that were orthophoric/exotropic in their first postoperative alignment (Table 5).
Stereopsis was recorded at the last visit, when the mean age in the first and second groups was 6.9 and 11.1 years, respectively.
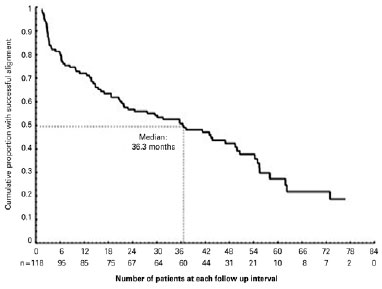
Survival analysis was performed using survival curves of the time from surgery to failure. We observed 77 unsuccessful cases, with the earliest and latest cases detected at 1.5 and 73 months after surgery, respectively. The longest follow-up was 83 months, and this case had a successful outcome. The mean time until the loss of success was 36.3 months (Figure 1).
DISCUSSION
The optimal timing of therapeutic intervention in intermittent exotropia is very controversial in the literature. The main concern in these cases is the preservation or restoration of stereopsis and cosmesis.
The reported surgical success rates with one procedure in intermittent exotropia vary widely, which is largely due to differences in surgical techniques, length of follow-up, age at surgery, preoperative deviations, and criteria of success. Our overall success rate was 35% with one procedure and 66% at the last follow-up. These low success rates when compared to other studies can be justified by the long minimum follow-up required (3 years or longer) and the success criteria that we adopted. Kang and Lee analyzed patients with a shorter minimum follow-up (6 months), and reported success in 83.33%, 66.67%, and 64.29% of patients with good, fair, and poor control before surgery (p=0.28)(9). Keenan and Willshaw achieved favorable outcomes in a much higher percentage of children operated on for exotropia (93%); however, they defined success as a final alignment for near and distance fixation within ±10 D of orthotropia, or within ± 20 D of orthotropia with evidence of binocular single vision(10).
Pineles et al. analyzed the long-term outcomes of the surgical management of intermittent exotropia, and found results similar to ours(11). With a minimum follow-up of 10 years, they found that, when using combined motor/sensory criteria for surgical success, 38% of the patients achieved an excellent outcome. Conversely, when only the motor criteria were used, 64% had an excellent outcome at the last follow-up, and 60% of the patients required at least one reoperation. In our series, 46% of the patients required more than one procedure.
Despite the presence of good stereopsis, surgically corrected intermittent exotropes may show a gradual outward shift with time. We observed 77 unsuccessful cases during the study, with the earliest and latest unsuccessful cases detected at 1.5 and 73 months after surgery, respectively. The mean time until the loss of success was 36.3 months. Maruo et al. also showed a strong tendency (50.4%) for intermittent exotropia to recur and drift into permanent exotropia over at least 4 years of follow-up(12). Two other studies included results on the survival analysis of patients with constant and intermittent exotropia, and estimated a mean time from surgery to recurrence of 68 and 48.3 months, respectively(13,14).
Many factors can lead to surgical failure, including stereopsis, amblyopia, and larger angles of deviation(15,16). Regarding stereopsis, Beneish and Flanders suggested that it is peripheral rather than central fusion that keeps the eyes well aligned after surgery and prevents the recurrence of exodeviation. They found that poor preoperative stereopsis combined with early overcorrection significantly improved the surgical success rate(17).
Many investigators agree that surgical treatment should be delayed until 4 years of age, because consecutive esotropia could potentially lead to amblyopia and affect stereopsis at a younger age(2). Some authors found no significant difference in the results between early and late surgery(4). On the contrary, others agree that even better results can be achieved when surgery is performed before 4 years of age(3).
In our study, no significant difference was found between the groups when amblyopia (p=0.341), success after the first surgery (p=0.698), and the need for additional surgery (p=0.712) were considered. However, we did find a higher chance of success at the last follow-up (104%) when surgery was performed at a younger age. Although the reoperation rate was also higher in this group (48% vs. 42% for the patients who underwent surgery later), the difference was not statistically significant (p=0.93). Maruo et al. also found that the rates of orthotropia or mini-microtropia were higher when the patients were operated before 3 years and after 11 years of age(12).
When comparing the postoperative alignment in the first week over all the patients, we failed to demonstrate any influence on the sensory outcome. Although the majority of the cases of unsatisfactory stereopsis were patients who had undergone surgery before 4 years of age, our data suggests that this may not be due to inadequate age at surgery, but rather, immaturity for performing the Titmus test(18-20). The mean age when stereopsis was assessed was 7 and 11 years in children operated on before the age of 4 years and at 4 years or older, respectively. Interestingly, worse stereopsis was also found in those who presented ortho- or exotropia at the first postoperative visit in the younger group.
A limitation of our series is that the control grade of the intermittent exotropia and the quality of life score were not reported. In basic intermittent exotropia, better control grade is usually accompanied by better stereoacuity and a higher surgical success rate(9). The majority of unsatisfactory outcomes in our study were undercorrections; however, patients with residual exotropia over 10 PD and with good control grades were not referred for additional surgery even though they were not classified as successful outcomes.
In intermittent exotropia, one of the most important indications for surgical intervention is an increasing tropia phase(1). Younger children tend to be referred for surgery when they have a poor control grade, usually worse than the grade considered for surgery in older children. In our series, the preoperative deviation was significantly worse in the younger group (p<0.001).
In this study, patients with unsatisfactory motor results had similar preoperative deviations, and none of the possible associated factors evaluated had any significant effect on success.
CONCLUSIONS
Patients with intermittent exotropia can be operated upon safely under 4 years of age, and may even present better motor results than older patients. However, they need to be followed closely. Stereoacuity was found to be worse in children who underwent surgery at a younger age; however, this finding is unlikely to be due to inadequate age for surgery, but rather, immaturity for performing the stereopsis test, as worse stereopsis results were also found in those who presented ortho- or exotropia at the first postoperative visit.
REFERENCES
1. Wright KW, Strube YNJ. Pediatric Ophthalmology and Strabismus. 3th ed. New York: Oxford University Press; 2012.
2. Edelman PM, Murphree AL, Brown MH, Wright KW. Consecutive esodeviation, then what? Am Orthopt J. 1988;38:111-6.
3. Pratt-Johnson JA, Barlow JM, Tillson G. Early surgery in intermittent exotropia. Am J Ophthalmol. 1977;84(5):689-94.
4. Richard JM, Parks MM. Intermittent exotropia. Surgical results in different age groups. Ophthalmology. 1983;90(10):1172-7.
5. Negrel AD, Maul E, Pokharel GP, Zhao J, Ellwein LB. Refractive error study in children: sampling and measurement methods for a multi-country survey. Am J Ophthalmol. 2000:129(4):421-6. Comment in: Am J Ophthalmol. 2000;129(4):525-7.
6. Duane AA. New Classification of the motor anomalies of the eye based upon physiologic principles. New York, NY JH Vai;. 1897.
7. Burian HM, Franceschetti AT. Evaluation of diagnostic methods for the classification of exodeviations. Trans Am Ophthalmol Soc. 1970;68:56-71.
8. Parks MM. Atlas of strabismus surgery. Lippincott, 1983.
9. Kang KT, Lee SY. Relationship between control grade, stereoacuity and surgical success in basic intermittent exotropia. Korean J Ophthalmol. 2015;29(3):173-7.
10. Keenan JM, Willshaw HE. The outcome of strabismus surgery in childhood exotropia. Eye (Lond). 1994;8(Pt 6):632-7. Comment in: Eye (Lond). 1996;10(Pt 1):151.
11. Pineles SL, Ela-Dalman N, Zvansky AG, Yu F, Rosenbaum AL. Long-term results of the surgical management of intermittent exotropia. JAAPOS. 2010;14(4):298-304.
12. Maruo T, Kubota N, Sakaue T, Usui C. Intermittent exotropia surgery in children: long term outcome regarding changes in binocular alignment. A study of 666 cases. Binocul Vis Strabismus Q. 2000;16(4):265-70. Comment in: Binocul Vis Strabismus Q. 2002;17(2):78; author reply 78-9.
13. Stoller SH, Simon JW, Lininger LL. Bilateral lateral rectus recession for exotropia: a survival analysis. J Pediatr Ophthalmol Strabismus. 1993;31(2):89-92.
14. Oh JY, Hwang JM. Survival analysis of 365 patients with exotropia after surgery. Eye (Lond). 2006;20(11):1268-72.
15. Jang JH, Park JM, Lee SJ. Factors predisposing to consecutive esotropia after surgery to correct intermittent exotropia. Graefe's Arch Clin Exp Ophthalmol. 2012;250(10): 1485-90.
16. Chiu AK, Din N, Ali N. Standardising reported outcomes of surgery for intermittent exotropia- a systematic literature review. Strabismus. 2014;22(1):32-6.
17. Beneish R, Flanders M. The role of stereopsis and early postoperative alignment in long-term surgical results of intermittent exotropia. Can J Ophthalmol. 1994;29(3): 119-24.
18. Simons, K. Stereoacuity norms in young children. Arch Ophthalmol. 1981;99(3):439-45.
19. Simons K. Visual acuity norms in young children. Surv Ophthalmol. 1983;28(2):84-92.
20. Donzis PB, Rappazzo JA, Bürde RM, Gordon M. Effect of binocular variations of Snellen's visual acuity on Titmus stereoacuity. Arch Ophthalmol. 1983;101(6):930-2.
Submitted for publication:
January 10, 2017.
Accepted for publication:
July 17, 2017.
Funding: Issaho DC was supported by the CAPES Foundation.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.
Approved by the following research ethics committee: The University of Texas, Southwestern Medical Center (# 032010-021).